Exploring what works, what doesn’t, and why.

Standout voices in African public health
- Share on LinkedIn
- Share on Twitter
- Share on Facebook
- Share on WhatsApp
- Share through Email
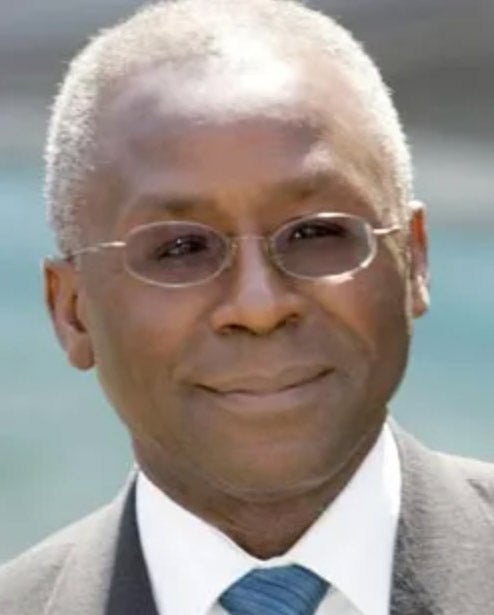
These are some of the notables making a new path for the field. They represent an increasingly deep bench of leaders shaping policy and practice on the continent.

Quarraisha Abdool Karim
Notable for: Developing HIV prevention solutions for women. Led South Africa’s first community-based HIV prevalence study in 1990, discovering disproportionately high rates of infection among adolescent girls. Helped establish and is associate scientific director of the Centre for the AIDS Programme of Research in South Africa (CAPRISA). Developed several woman-controlled HIV prevention methods, including vaginal microbicides. Co-chairs a UN expert group advising governments on using science and technology for sustainable development. Is a professor of epidemiology at the Columbia University Mailman School of Public Health . — Linda Nordling

Salim Abdool Karim
Notable for: Prevention and treatment of HIV and tuberculosis. Karim’s clinical research revealed that antiretrovirals can prevent sexually transmitted HIV infection and genital herpes in women. Co-invented patents used in HIV vaccine candidates. Leads the South African Ministerial Advisory Committee on COVID-19. Chairs the UNAIDS Scientific Expert Panel and WHO’s HIV Strategic and Technical Advisory Committee , and is a member of the WHO TB-HIV Task Force. — Gilbert Nakweya

Akinwumi A. Adesina
Notable for: Boosting food security. As Nigeria’s minister of agriculture and rural development, leveraged mobile phones to increase access to improved seeds and fertilizers for 15 million farmers, boosting food production by 21 million metric tons. Rooted out corruption in Nigeria’s agriculture sector, prompting Forbes Africa magazine to name him its Person of the Year in 2013. An economist, he is currently in his second term as president of the African Development Bank Group . — Esther Nakkazi

Agnes Binagwaho
Notable for: Global health equity and social justice. Vice chancellor and co-founder of Rwanda’s University of Global Health Equity , an initiative of Partners In Health . UGHE aims to refocus health education on expanding access to services. As Rwanda’s minister of health became known for #MinisterMondays, regular Twitter discussions on global health policy. — Esther Nakkazi
Sign up for Harvard Public Health
Delivered to your inbox weekly.
- Email address By clicking “Subscribe,” you agree to receive email communications from Harvard Public Health.
- Phone This field is for validation purposes and should be left unchanged.
Winnie Byanyima
Notable for: Expanding access to health services. As UNAIDS executive director , drives attention to the public health impacts of social justice and gender equality. Works to remove barriers to health services for women and vulnerable groups through the elimination of discriminatory laws. Has expanded HIV/AIDS prevention, testing, and treatment services to key populations. — Paul Adepoju

Kelly Chibale
Notable for: Drug discovery in Africa. In 2010, Zambia-born Chibale founded his drug discovery and development center H3D at the University of Cape Town , where his team developed antimalarial drugs now in early-phase human clinical trials – a first for an African drug discovery team . Works to optimize medicines for African populations, by studying how their livers digest common drugs. Also collaborates with industry to create jobs for young African scientists. — Linda Nordling
Mohammed Malick Fall
Notable for: Response to COVID-19. As UNICEF regional director for Eastern and Southern Africa , the native of Senegal led a large team to coordinate responses to COVID-19 across the continent. Worked with countries and other partners to procure, mobilize, and distribute vaccine doses and other tools to fend off the pandemic. Has been involved in UN initiatives in Afghanistan, France, Haiti, Indonesia, Mongolia, and Switzerland. —Paul Adepoju

Temie Giwa-Tubosun
Notable fo r : Supply chain logistics. Nigerian entrepreneur who founded LifeBank , a healthcare technology and logistics company that started with improving access to blood units for transfusion services in Nigeria and beyond. Has since expanded into medical oxygen access for patients. She works to develop and spread technologies that can be used to predict need for health commodities to create more efficient supply chains. — Paul Adepoju

Christian Happi
The professor of molecular biology and genomics at Nigeria’s Redeemer’s University leads a center crucial for pathogen genomic surveillance in Africa. It serves as a reference laboratory for the WHO and Africa CDC. Produced the continent’s first genomic sequence for COVID-19. Also helps other African countries with sequencing, research, and more. —Paul Adepoju

Catherine Kyobutungi
Notable for: Health care systems research and capacity building. Worked as a medical officer in rural Uganda and as a lecturer at Mbarara University of Science and Technology. A 2019 Joep Lange Chair at the University of Amsterdam where she investigates chronic disease management in Africa. Co-directs the Consortium for Advanced Research Training in Africa which trains early-career researchers at PhD and post-doctoral level, and heads the African Population and Health Research Center. — Gilbert Nakweya

Zaakira Mahomed
Notable for: Menstrual hygiene and sanitation. South African businesswoman, social entrepreneur, and activist. Started the Mina Foundation to develop a sustainable, healthy, and eco-friendly alternative to current methods of period care. Mina menstrual cups have been distributed to more than 70,000 women through partnerships in six countries in Africa and the Middle East. Works to normalize menstruation promote period positivity and keep young women and girls in school during their periods. — Esther Nakkazi
Julie Makani
Notable for: Genomic research, advocacy, and awareness for sickle cell disease in Africa. Established the world’s largest study center for sickle cell disease at Tanzania’s Muhimbili University of Health and Allied Sciences . Founded the Sickle Cell Foundation of Tanzania to raise awareness of the disease. Makani is the principal investigator for the Sickle Pan African Research Consortium under the Sickle In Africa network. — Gilbert Nakweya

Mamello Makhele
Notable for: Improving access to maternal health for women in rural areas. Registered nurse-midwife based in Lesotho. During the pandemic traveled by donkey and on foot into rural Lesotho to bring maternal care services, healthcare, and contraceptives. Named a Bill Gates’ Heroes in the Field . A Shedecides leader for Lesotho, educating young people on child marriages, consent, and teenage pregnancy. Board member of Safe Abortion Action Fund in London. — Esther Nakkazi

Strive Masiyiwa
Notable for: Increasing vaccine access. Zimbabwean billionaire businessman and philanthropist was engaged to lead the African Union ‘s African Vaccine Acquisition Trust. Actively highlighted the vaccine inequity that plagued the early months of COVID-19 vaccination rollout. Led discussions and negotiations that resulted in the availability of vaccine doses from several sources, including the fill-and-finish agreement bringing the Johnson & Johnson COVID-19 vaccine to Africa. — Paul Adepoju

Matshidiso Moeti
Notable for: Reducing inequity. First female World Health Organization regional director for Africa . Marshaled global health actions by providing direction, leadership, and access to support for health ministries across Africa. Brought attention to health inequities and coordinated WHO response to COVID outbreaks across the continent through measures such as helping Somalia acquire medical oxygen infrastructure. Working to help African countries prepare for future pandemics. — Paul Adepoju

Jean-Jacques Muyembe
Notable for: The discovery of Ebola virus disease. The Congolese microbiologist leads public health emergency responses in the Democratic Republic of the Congo, including for COVID-19. He led the design of Ebola treatment and pioneered the deployment of experimental Ebola vaccines. Heads the DRC’s Institut National de la Recherche Biomédicale , a significant contributor to global knowledge of infectious diseases. — Paul Adepoju

Wilfred Ndifon
Notable for: Research on the immune system. Discovered a mechanism for T-cell generation, showed how influenza interferes with the immune system’s antibodies, and proposed an explanation for the idea of original antigenic sin , a well-known phenomenon in immunologic response systems. The Cameroonian virologist’s work could lead to the development of ‘zero-interference’ vaccines, expected to improve immune response. Currently chief scientific officer of the African Institute for Mathematical Sciences Global Network. — Esther Nakkazi

John N. Nkengasong
Notable for: Public health leadership. Cameroonian virologist was the first head of the Africa CDC and helped build frameworks for stronger health systems across Africa, emphasizing cross-border collaboration, capacity building, and resource mobilization. Led the African Union’s public health agency in responding to Ebola, Lassa fever, and COVID-19. First African to head PEPFAR , the U.S’s global effort to combat HIV/AIDS. —Paul Adepoju

Muhammad Pate
Notable for: Healthcare systems innovation and reform. In Nigeria, galvanized efforts to reduce polio and drove innovation across the country’s health sector, including launching the Midwives’ Service Scheme to help reduce maternal and childhood mortality. At the World Bank , Pate initiated a $100 million private-public partnership in Lesotho to build a new national referral hospital, completed in 2011. This was one of the first such development effort s in the health care sector in Africa. Co-chairs a Lancet commission aiming to improve global health systems and teaches at Harvard T.H. Chan School of Public Health . — Michael Fitzgerald

Notable for: Translating health research into policy and practice. An anti-apartheid activist doctor, she has led the Reproductive Health and HIV Institute at the University of the Witwatersrand in Johannesburg since 1994. Has served on a multitude of global health advisory bodies and committees on vaccines. Advises the South African government on Covid variants and vaccines. Co-leads South Africa’s arm on the WHO’s COVID-19 Solidarity Therapeutics Trial . Chairs the South African Health Products Regulatory Authority and fought vaccine disinformation during the pandemic. — Linda Nordling
David Moinina Sengeh
Notable for: Policy innovation. Being Chief Innovation Officer for Sierra Leone and also its minister for basic and secondary education does not sound like a public health job. But Sengeh and his team at the Directorate of Science, Technology, and Innovation became the fulcrum for the country’s fight against COVID-19, providing data and analysis to shape emergency response, lockdown policies, and school closings and reopenings. It also developed tools to share information with the populace, such as the Moi Minute, public health messages Sengeh recorded that were on Youtube and TV. — Michael Fitzgerald

Flavia Senkubuge
Notable for: Academic leadership. First Black female president and youngest ever (at age 39) of the Colleges of Medicine of South Africa , only the third woman president in its 66 years. CMSA sets the country’s standards for medical and dental education and care. She is deputy dean of health stakeholder relations at the University of Pretoria , Faculty of Health Sciences. Chairs the WHO/Afro African Advisory Committee on Research and Development ( AACHRD ). — Esther Nakkazi
Michel Sidibé
Notable for: Rallying support for the African Medicines Agency, established to coordinate pan-African regulatory structures and standards. Left position as Mali’s minister of health and social affairs to become African Union special envoy, lobbying governments to sign and ratify the AMA treaty . Helped establish the AMA. Had been the second executive director of UNAIDS . — Paul Adepoju
Oyewale Tomori
Notable for: Researching viruses. Established the African Regional Polio Laboratory Network, helping nearly eradicate poliovirus infections. Has studied Ebola, Lassa fever, Yellow fever, and Chikungunya, a virus that causes joints to swell. The Nigerian virologist, who also holds a DVM in veterinary medicine, isolated the properties of the Orungo arbovirus, which can cause encephalitis. — Esther Nakkazi
Notable for: Vaccine manufacturing. Spearheading Egypt’s private sector COVID-19 vaccine manufacturing initiative. Leads Egypt’s largest vaccine production facility, which has produced tens of millions of doses of the Sinovac vaccine. Plays a key role in helping the continent fulfill its goal of producing 60% of its own vaccines by 2040, developing vaccine production partnerships and transfer of vaccine manufacturing technology in other parts of Africa. — Paul Adepoju
This story has been updated to clarify Quarraisha Abdool Karim’s role in developing HIV prevention methods.
Contributors: Paul Adepoju is a Nigerian science journalist. Esther Nakkazi is a Ugandan science journalist and blogger. Gilbert Nakweya is a Kenyan science journalist. Linda Nordling is a science journalist based in South Africa. Michael Fitzgerald is Editor-in-Chief of Harvard Public Health.
Photos: Quarraisha Abdool Karim: Rajesh Jantilal; Salim Abdool Karim: Dean Demos, CAPRISA; Adesina: AfDB; Binagwaho: Courtesy of Agnes Binagwaho; Chibale: University of Capetown; Giwa-Tubosun: Courtesy of Temie Giwa-Tubosun; Happi, Moeti, Muyembe, and Nkengasong: Paul Adepoju; Kyobutungi: Florence Sipalla, APHRC; Mahomed: Courtesy of Zaakira Mahomed; Makhele: Lee-Ann Olwage; Masiyiwa: Gus Ruelas / Rueters; Ndifon: AIMS; Pate: Harvard Chan School; Rees: Wits University; Senkubuge: Courtesy of Flavia Senkubuge; Tomori: Courtesy of Oyewale Tomori.
Spring 2022
More in global health.

Cambodia’s new path for prosthetic care

How public health officials keep hope alive in Sudan’s civil war

How a deadly global crisis went unseen
HEALTH RESEARCH IN AFRICA
About the journal.
Health Research in Afr ica (HRA) is an open access, peer reviewed medical journal that is affiliated to Health Sciences and Disease . HRA values high quality research with impact on clinical care in order to improve human health in Africa. HRA covers all aspects of medicine, pharmacy, biomedical and health sciences, including public health and societal issues. Like HSD, it is an “online first” publication, which means that all the publications articles appear on the website before being included in the print journal. The papers are published in full on the website, with open access. Acceptance of manuscripts is based on the originality, the quality of the work and validity of the evidence, the clarity of presentation, and the relevance to our readership. Publications are expected to be concise, well organized and clearly written. Authors submit a manuscript with the understanding that the manuscript (or its essential substance) has not been published other than as an abstract in any language or format and is not currently submitted elsewhere for print or electronic publication. HRA is published by Afrimvoe Medical Services , Yaounde (Cameroon).
Current Issue
Front Cover Page
Please download the front cover page here, in this issue, please, download the full contents page here, about health research in africa, a few facts about your journal, research articles, mortality within 30 days of administration of a systemic anticancer therapy in a medical oncology unit of yaounde mortalité dans les 30 jours suivant l'administration d'une thérapie anticancéreuse systémique dans une unité d'oncologie médicale à yaoundé, determinants of the non-use of insecticide-treated mosquito nets in benin déterminants de la non-utilisation des moustiquaires imprégnées d'insecticide au bénin, knowledge, attitudes and practices related to blood donation among the population of kribi connaissances, attitudes et pratiques liées au don de sang des populations de kribi, iron overload in living children with major sickle cell syndrome la surcharge en fer chez les enfants vivant avec un syndrome drépanocytaire majeur, impact of reactive vaccination on the 2021 meningitis epidemic in banalia impact de la vaccination réactive sur l'epidémie de méningite de 2021 à banalia, serum creatinine as a predictive tool of adverse outcomes in covid-19 patients in douala créatinine sérique comme outil prédictif des résultats défavorables chez les patients atteints de covid-19 à douala., prevalence and characterization of adverse effects of proton pump inhibitors in brazzaville, congo prévalence et caractérisation des effets indésirables des inhibiteurs de la pompe à protons à brazzaville au congo., prevalence of gastrointestinal toxicity in patients receiving platinum-based chemotherapy at douala general hospital prévalence de la toxicité gastro-intestinale chez les patients recevant une chimiothérapie à base de platine à l'hôpital général de douala, evaluation of oxidative stress by plasma measurement of oxidized ldl in type 2 diabetics in mali évaluation du stress oxydatif par le dosage plasmatique des ldl oxydées chez les diabétiques de type 2 au mali, medicine and surgery in the tropics, skin diseases of diabetic patients in mali: prevalence and clinical presentation les dermatoses chez les patients diabétiques au mali : prévalence et aspects cliniques, epidemioclinical pattern of glenohumeral dislocations at owendo university hospital profil épidémioclinique des luxations gléno-humérales au chu d’owendo, outcome of surgical treatment of adult’s olecranon fracture in yaoundé résultat du traitement chirurgical de la fracture de l'olécrane de l'adulte à yaoundé, insulin therapy of diabetic patients at hopital du mali from 2016 to 2017 l’insulinothérapie chez les patients diabétiques à l’hôpital du mali de 2016 à 2017, spectrum of surgical emergencies in a national reference hospital of niger profil des urgences chirurgicales dans un hôpital de référence national du niger, medical secrecy in the context of the response against the covid-19 health crisis in cameroon: analysis from the united#covid-19 le secret médical dans le contexte de la réponse à la crise sanitaire du covid-19 au cameroun : analyse de united#covid-19, functional results and patient satisfaction after cataract surgery by phacoemulsification in gabon résultats fonctionnels et satisfaction des patients après chirurgie de la cataracte par phacoémulsification au gabon, clinical, paraclinical, therapeutic and evolutionary aspects of gout in brazzaville aspects cliniques, paracliniques, thérapeutiques et evolutifs de la goutte à brazzaville, factors associated with mortality of covid-19 patients hospitalized in conakry from 2020 to 2022 facteurs associés à la mortalité des patients covid-19 hospitalisés à conakry de 2020 à 2022, anatomical dissections and cultures: the teaching of anatomy and bantu beliefs dissections anatomiques et cultures: enseignement de l’anatomie et croyances bantu, case reports, inverted papilloma of right maxillary sinus with subdural and orbital extension : a case report inverted papilloma of right maxillary sinus with subdural and orbital extension : a case report, pheochromocytoma and neuromalaria: a disturbing morbid association pheochromocytome et neuro-paludisme: une association pathologique déroutante, an unexpected dystocia after head delivery, linked to a large sacrococcygeal teratoma in a situation of limited resources and insecurity due to terrorist armed groups in burkina faso dystocie après accouchement de la tête liée à un volumineux tératome sacrococcygien en situation de ressources limitées et d’insécurité liée aux groupes armés terroristes, author guidelines, please, download the guidelines for authors here, and read carefully before submitting.

Endorsed by

The University of Yaounde 1
Our Partners
Make a submission, follow us on social media.
HRA on facebook
Useful links
Conseil Africain et Malgache pour l'Enseignement Supérieur (CAMES)
Faculté de Médecine et des Sciences Biomédicales (UYI)
Afrimvoe Medical Services
African Union
Ministry of Higher Education
Ministry of Public Health
Information
- For Readers
- For Authors
- For Librarians
EDITORIAL POLICIES
EDITORIAL POLICIES, ETHICS AND PEER REVIEWING
HRA’s Publications Policy Committee follows the recommendations of the International Committee of Medical Journal Editors (ICMJE ), the World Association of Medical Editors (WAME) , and the Committee on Publication Ethics (COPE) for guidance on policies and procedures related to publication ethics. The policies for HRA have been adapted from those three advisory bodies and, where necessary, modified and tailored to meet the specific content, audiences, and aims of HRA. Review process
Research manuscripts are initially checked by the editor in chief or section editor for identification of gross deficiencies. At this stage, the proposal may be rejected. After this initial screening, articles are sent to one or two-reviewers whose names are hidden from the author and whose review is guided by a checklist (single anonymized review). The review summary is signed by the reviewer and is not posted with article. The review process may take days to weeks to reach a final decision that is the responsibility of the editor in chief. The duration from submission to publication may take one to six months (average: 6 months). So, the authors should avoid contacting the editorial office less than 6 weeks after the initial submission. Plagiarism, Scientific Misconduct Manuscripts proven of plagiarism will be returned to the authors without peer review. The editors reserve the right to request that the authors provide additional data collected during their investigations. The editors also reserve the right to send a copy of the manuscript and data in question to the author’s dean, university, or supervisor or, in the case of an investigation being funded by an agency, to that funding agency for appreciation. Conflict of Interest At the time of submission, authors are asked to disclose whether they have any financial interests or connections, direct or indirect, or other situations that may influence directly or indirectly the work submitted for consideration. Human and Animal Studies Manuscripts reporting results of prospective or retrospective studies involving human subjects must document that appropriate institutional review board (IRB) approval and informed consent were obtained (or waived by the IRB) after the nature of the procedure(s) had been fully explained. Authorship To be listed as an author, an individual must have made substantial contributions to all three categories established by the International Committee of Medical Journal Editors (ICMJE ) : (a) “conception and design, or acquisition of data, or analysis and interpretation of data,” (b) “drafting the article or revising it critically for important intellectual content,” and (c) “final approval of the version to be published.” Individuals who have not made substantial contributions in all three categories but who have made substantial contributions either to some of them or in other areas should be listed in acknowledgments. Please limit the number of authors to ten when this is feasible.
Content licensing - Open access compliance - Copyright Since its creation, articles published in HRA are Open Access and distributed under the terms of the Creative Commons Non-Commercial No-Derivatives License (CC BY-NC-ND 4.0) The authors publishing under this license with HRA retain all rights which means that the authors can read, print, and download, redistribute or republish (eg, display in a repository), translate the article (for private use only, not for distribution), download for text and data mining, reuse portions or extracts in other works, but they are not allowed to sell or re-use for commercial purposes or re-use for non-commercial purposes; without asking prior permission from the publisher, provided the original work is properly cited. Language HRA accepts publications in English and French . All the publications should have an abstract in both languages. Whenever possible, picture captions and table titles should be in both languages. All accepted manuscripts are copy-edited. Particularly if English is not your first language, before submitting your manuscript, HRA advises the work to have it edited for language. Artificial Intelligence (AI)–Assisted Technology At submission, the authors should disclose whether they used artificial intelligence (AI)–assisted technologies in the production of the publication and how AI was used. However, authors should not list AI and AI-assisted technologies as an author or co-author, nor cite AI as an author.
TYPES OF ARTICLES The main sections are original articles, clinical cases, brief reports, review articles, letters to the editor, pictures and disease, medicine and society or book reviews
CHECK LISTS 1. For studies dealing with diagnostic accuracy, use the Standards for Reporting of Diagnostic Accuracy (STARD) http://www.equator-network.org/reporting-guidelines/stard/ 2. For randomized controlled trials, use the CONSORT (Consolidated Standards of Reporting Trials) statement (BMJ 2010; 340). 3. For systemic reviews and meta-analyses of diagnostic test accuracy studies, follow the PRISMA-DTA (Preferred Reporting Items for Systematic Reviews-Diagnostic Test Accuracy) guidelines) http://www.prisma-statement.org/Extensions/DTA. 4. For observational studies, such as cohort, case-control, or cross-sectional studies, use the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) guidelines. https://www.strobe-statement.org/index.php?id=strobe-home
ARTICLE PROCESSING CHARGES (APC) Article submission is free of charges, but if your paper is accepted for publication, you will be asked to pay article processing charges to cover publications costs (220-250 $), depending on the type, complexity and length of the work, and on the number of authors. To guarantee HRA's independence, APC cover publication charges such as electronic archiving, plagiarism checking, editing, peer review process, site maintenance and web-hosting, proofreading, quality check, PDF designing and article maintenance. FAST TRACK Please, contact the editor-in-chief. Special article processing charges may apply.
Developed By
Address Health Research in Africa Afrimvoe Medical Services PO Box 17583, Yaoundé Cameroon.
Contact Info Samuel Nko'o-Amvene Phone: +237699970946 / 677257000 Email: [email protected]
Thank you for visiting nature.com. You are using a browser version with limited support for CSS. To obtain the best experience, we recommend you use a more up to date browser (or turn off compatibility mode in Internet Explorer). In the meantime, to ensure continued support, we are displaying the site without styles and JavaScript.
- View all journals
- Explore content
- About the journal
- Publish with us
- Sign up for alerts
- 05 September 2023
A new model for public health in Africa can become a reality

- Jean Kaseya 0
Jean Kaseya is director-general of the Africa Centres for Disease Control and Prevention (Africa CDC) in Addis Ababa, Ethiopia.
You can also search for this author in PubMed Google Scholar
You have full access to this article via your institution.
This year is a crucial one for the Africa Centres for Disease Control and Prevention (Africa CDC). Launched by the African Union (AU) in 2017 after the Ebola epidemic in West Africa, the organization was directed by Cameroonian virologist John Nkengasong for its first five years, including the first two years of the COVID-19 pandemic. I succeeded him as director-general in April after more than 25 years of managing public-health programmes across Africa, working with bodies such as the World Health Organization (WHO), the United Nations children’s charity UNICEF and GAVI, the vaccine alliance.
The Africa CDC faces many challenges, not least to apply the lessons learnt from COVID-19 ( C. T. Happi & J. N. Nkengasong Nature 601 , 22–25; 2022 ) as we strive to become a world-class, self-sustaining and agile institution. According to our 2022 priority ranking of infectious diseases, Ebola, cholera and COVID-19 have the highest epidemic potential across Africa, and the diseases the continent is least prepared for are the plague and Crimean–Congo haemorrhagic fever, as well as any as-yet unknown disease.

Africa is bringing vaccine manufacturing home
Our remit has also expanded to include non-infectious diseases and mental health. In many AU nations, people are more likely to die of non-communicable diseases — such as cardiovascular disease, cancer and diabetes — than of communicable, nutritional, maternal and perinatal conditions put together. Yet less than 20% of AU member states have surveillance programmes for non-communicable diseases.
In response to these challenges, our efforts to transform public health on the continent are focused on six areas:
Local manufacturing of vaccines, diagnostics and treatments. The Africa CDC must coordinate the continental agenda on local manufacturing of these fundamental health-care tools , targeting outbreak-prone as well as non-communicable diseases, and mental-health conditions. This includes working with various stakeholders to ensure that appropriate regulatory frameworks are in place, providing manufacturers with financial support and helping to create a conducive market environment. To help expand regional manufacturing capabilities, we have signed a memorandum of understanding with GAVI to work on market design and forecasting of vaccine demand.
Improved surveillance, intelligence and early-warning systems. A new partnership between the Africa CDC, the WHO and the Robert Koch Institute in Berlin will improve health security on the continent by strengthening integrated disease surveillance at the community level, democratizing genomic surveillance and strengthening epidemic intelligence. The first phase will be implemented in Gambia, Mali, Morocco, Namibia, Tunisia and South Africa.
We are also working to outfit all rural health clinics with tests for the 15 most common infectious diseases. Ruling out pathogens that researchers already know about is the best way for these clinics to reliably flag potential new diseases — and prevent them from jumping from rural to more densely populated urban areas.
Integrated health systems and robust primary care. Because of the crucial role of primary care in both infectious and non-communicable disease prevention and management, Africa CDC has secured a grant to fund primary health-care facilities in rural areas. Even in areas that don’t have a freezer capable of storing biological samples at −80 °C, much can be accomplished by improving information technology and empowering community-health workers to collect and process samples and send them to central laboratories.

Two years of COVID-19 in Africa: lessons for the world
As part of our mission to mentor and develop the next generation of public-health leaders, this year the Africa CDC has allocated US$3.9 million to training programmes, including for field epidemiologists. In partnership with the Kofi Annan Foundation, established by the Ghanaian former UN secretary-general, we have trained 40 leaders of public-health institutions from 31 AU member states; another 20 have just been accepted for training.
Expanded networks of laboratories. Since 2020, the Africa CDC’s Pathogen Genomics Initiative has conducted 5 training sessions and delivered sequencing and automation systems, equipment and reagents to 14 AU member states, broadening access to genomic surveillance.
Emergency preparedness and response. To improve cross-border coordination, the Africa CDC will harness technologies developed during the COVID-19 pandemic. One example is the PanaBIOS system, a transcontinental digital suite and mobile application for monitoring disease outbreaks, which will be used by 27 countries.
Strong national public-health institutes. The Africa CDC has begun bolstering national public-health institutes and emergency operations centres in 20 AU member states and will eventually establish a support team in each member state. We also met with a group of AU health ministers to devise shared negotiation strategies for the WHO’s proposed pandemic treaty and the UN High-Level Meeting on Universal Health Coverage.
All six of these actions will require sustained support from African communities, AU member states, donors and other partners. I am convinced that a new way of doing public health in Africa is within reach.
Nature 621 , 9 (2023)
doi: https://doi.org/10.1038/d41586-023-02749-5
Reprints and permissions
Competing Interests
The author declares no competing interests.
Related Articles

Africa: a new dawn for local vaccine manufacture
- Public health
- Developing world

Could bird flu in cows lead to a human outbreak? Slow response worries scientists
News 17 MAY 24

Neglecting sex and gender in research is a public-health risk
Comment 15 MAY 24
Interpersonal therapy can be an effective tool against the devastating effects of loneliness
Correspondence 14 MAY 24

Gut microbes linked to fatty diet drive tumour growth
News 16 MAY 24

Dual-action obesity drug rewires brain circuits for appetite
News & Views 15 MAY 24

Experimental obesity drug packs double punch to reduce weight
News 15 MAY 24
Imprinting of serum neutralizing antibodies by Wuhan-1 mRNA vaccines
Article 15 MAY 24

Vaccine-enhancing plant extract could be mass produced in yeast
News & Views 08 MAY 24

UTIs make life miserable — scientists are finding new ways to tackle them
News 02 MAY 24
Senior Postdoctoral Research Fellow
Senior Postdoctoral Research Fellow required to lead exciting projects in Cancer Cell Cycle Biology and Cancer Epigenetics.
Melbourne University, Melbourne (AU)
University of Melbourne & Peter MacCallum Cancer Centre
Overseas Talent, Embarking on a New Journey Together at Tianjin University
We cordially invite outstanding young individuals from overseas to apply for the Excellent Young Scientists Fund Program (Overseas).
Tianjin, China
Tianjin University (TJU)
Chair Professor Positions in the School of Pharmaceutical Science and Technology
SPST seeks top Faculty scholars in Pharmaceutical Sciences.
Chair Professor Positions in the School of Precision Instruments and Optoelectronic Engineering
We are committed to accomplishing the mission of achieving a world-top-class engineering school.
Chair Professor Positions in the School of Mechanical Engineering
Aims to cultivate top talents, train a top-ranking faculty team, construct first-class disciplines and foster a favorable academic environment.
Sign up for the Nature Briefing newsletter — what matters in science, free to your inbox daily.
Quick links
- Explore articles by subject
- Guide to authors
- Editorial policies
- Announcements
- About AOSIS
Journal of Public Health in Africa
- Editorial Team
- Submission Procedures
- Submission Guidelines
- Submit and Track Manuscript
- Publication fees
- Make a payment
- Journal Information
- Journal Policies
- Frequently Asked Questions
- Reviewer Guidelines
- Article RSS
- Support Enquiry (Login required)
- Aosis Newsletter

Quick links:
- Articles by Author
- Articles by Issue
- Articles by Section
- Find an Article
- Login / Log Out
Subscribe to our newsletter
Get specific, domain-collection newsletters detailing the latest CPD courses, scholarly research and call-for-papers in your field.
Journal of Public Health in Africa | ISSN: 2038-9922 (PRINT) | ISSN: 2038-9930 (ONLINE)
- Program Finder
- Admissions Services
- Course Directory
- Academic Calendar
- Hybrid Campus
- Lecture Series
- Convocation
- Strategy and Development
- Implementation and Impact
- Integrity and Oversight
- In the School
- In the Field
- In Baltimore
- Resources for Practitioners
- Articles & News Releases
- In The News
- Statements & Announcements
- At a Glance
- Student Life
- Strategic Priorities
- Inclusion, Diversity, Anti-Racism, and Equity (IDARE)
- What is Public Health?
Africa’s New Approach to Public Health
Related content.

A Brief History of Traffic Deaths in the U.S.

The Hunger Gap

Rewriting the Story of Life’s Later Years

Inside the Movement to Transform Mental Health in Sierra Leone

What to Know About COVID FLiRT Variants
- Open access
- Published: 11 December 2021
Measuring health science research and development in Africa: mapping the available data
- Clare Wenham ORCID: orcid.org/0000-0001-5378-3203 1 ,
- Olivier Wouters 1 ,
- Catherine Jones 2 ,
- Pamela A. Juma 2 ,
- Rhona M. Mijumbi-Deve 2 , 3 , 4 ,
- Joëlle L. Sobngwi-Tambekou 2 , 5 &
- Justin Parkhurst 1
Health Research Policy and Systems volume 19 , Article number: 142 ( 2021 ) Cite this article
5693 Accesses
9 Citations
33 Altmetric
Metrics details
In recent years there have been calls to strengthen health sciences research capacity in African countries. This capacity can contribute to improvements in health, social welfare and poverty reduction through domestic application of research findings; it is increasingly seen as critical to pandemic preparedness and response. Developing research infrastructure and performance may reduce national economies’ reliance on primary commodity and agricultural production, as countries strive to develop knowledge-based economies to help drive macroeconomic growth. Yet efforts to date to understand health sciences research capacity are limited to output metrics of journal citations and publications, failing to reflect the complexity of the health sciences research landscape in many settings.
We map and assess current capacity for health sciences research across all 54 countries of Africa by collecting a range of available data. This included structural indicators (research institutions and research funding), process indicators (clinical trial infrastructures, intellectual property rights and regulatory capacities) and output indicators (publications and citations).
While there are some countries which perform well across the range of indicators used, for most countries the results are varied—suggesting high relative performance in some indicators, but lower in others. Missing data for key measures of capacity or performance is also a key concern. Taken as a whole, existing data suggest a nuanced view of the current health sciences research landscape on the African continent.
Mapping existing data may enable governments and international organizations to identify where gaps in health sciences research capacity lie, particularly in comparison to other countries in the region. It also highlights gaps where more data are needed. These data can help to inform investment priorities and future system needs.
Peer Review reports
Introduction
Health sciences research (HSciR) has been defined to include basic, clinical and applied science on human health and well-being, as well as the determinants, prevention, detection, treatment and management of disease [ 1 , 2 , 3 ]. To date, the majority of HSciR has taken place in the Global North [ 4 , 5 , 6 ]. As of 2018, less than 1% of scientific articles published worldwide each year include at least one author based at an African institution [ 7 ].
In the past few years, however, a number of international organizations, including the African Union [ 8 ], WHO [ 9 ] and the World Bank [ 10 ], have called for political and economic investment in HSciR in Africa. Several high-profile reports have further raised awareness of the so-called 10/90 gap: only a 10th of global expenditure on health research is targeted to issues that affect the poorest 90% of the world’s population [ 5 ].
There are two key reasons why investments in HSciR in Africa may be particularly important from a developmental perspective. First, the promotion of a strong health science industry, as part of broader efforts to establish a robust research and development (R&D) landscape, can contribute to development goals by reducing national economies’ reliance on primary commodity and agricultural production; this can help governments develop knowledge-based economies, which may be important for macroeconomic growth [ 11 , 12 , 13 , 14 , 15 ]. In a seminal 1990 report, the Commission on Health Research and Development [ 4 ] stated that strengthening research capacity in low- and middle-income countries (LMICs) is “one of the most powerful, cost-effective and sustainable means of advancing health and development” (p. 71).
Second, HSciR may contribute to improvements in health, social welfare and poverty reduction through domestic application of the findings of the research itself [ 16 , 17 , 18 ]. The 2013 World Health Report stressed that all nations should be producers, users and consumers of HSciR [ 6 ]. Africa is home to nearly one sixth of the world’s population and is estimated to account for about a quarter of the global burden of disease [ 19 ]. Yet only a small fraction of global health research currently focuses on diseases which exclusively affect LMICs [ 20 , 21 ]. While there have been developments in the HSciR landscape over the past three decades, many LMICs have been unable to build up sufficient capacity to develop their own evidence base nationally to inform policy directly and/or to improve their population’s health [ 22 , 23 , 24 ]. The International Vaccines Task Force of the World Bank has highlighted the importance of building research capacity to lower the risk of emergent epidemics [ 25 ].
To date, few academic studies have evaluated HSciR capacity in LMICs. The most widely available indicator of health research capacity is the publication of health-related scientific journal articles. These have been the focus of research in the past, with bibliometric analyses undertaken to map the numbers of African publications related to cardiovascular diseases [ 26 , 27 ], genomics [ 28 ], health economic evaluation [ 29 ], health policies and systems [ 30 , 31 ], human immunodeficiency virus [ 32 ], neglected tropical diseases [ 33 ] and public health [ 34 ]. Four studies have also examined the total number of African publications on any health-related topic (as indexed in major bibliographic databases) [ 35 , 36 , 37 , 38 ]. Beyond publication outputs, however, researchers have also collected data on investments in health-related R&D [ 35 ], clinical trial infrastructures [ 25 , 35 ], healthcare workforce numbers [ 39 ] and the numbers of universities and “centres of excellence” [ 39 , 40 ] in African countries to estimate HSciR capacity.
Each of these studies can help to understand individual aspects of HSciR capacity in African countries, yet no single piece of information can fully capture the degree of capacity in a country or region. There remains a need for analyses which attempt to collect and analytically combine data on multiple indicators to provide a more comprehensive analysis of HSciR capacity across the continent.
The importance of knowledge economies
Science and innovation, if well-utilized, may play a core role in realizing sustainable development [ 1 , 41 ]. As seen from the experiences of many industrialized nations, scientific research and linked innovations have been core to economic and social advancement over the past two centuries—be it medical innovations such as vaccines and antibiotics, or industrial innovations in manufacturing, communications and computation [ 42 , 43 , 44 ].
More recently, questions have been asked as to whether scientific research supports development, or whether it represents a product of development [ 45 , 46 ]. Both these positions have their justifications. In terms of science resulting in development, it is research and knowledge generation, linked with subsequent innovation and application of that knowledge, that some argue has been critical to overcoming key development challenges in LMICs [ 45 ]. Under this position, the need to invest in capacity for mobilizing and using science and innovation can be viewed as an essential component of strategies for promoting sustainable development [ 47 , 48 , 49 ]. This argument appears to underpin the inclusion of research within the Sustainable Development Goals. Goal 3.B specifically focusses on health research for LMIC needs, calling for “supporting the development of research and development of vaccines and medicines for health conditions which affect LMICS”; goals 9.5 and 12.A call for increased scientific, technical and research capacity more generally in developing countries [ 50 ].
Many calls for the creation of so-called knowledge economies are linked to thinking of research activity as an end goal of development. It has been argued that the conceptualization of an economy of knowledge reproduces a growth and market-oriented rationale for knowledge production, accumulation and diffusion which has particularly influenced the international aid, education and development agenda [ 51 , 52 ]. For example, the Organisation for Economic Co-operation and Development (OECD) [ 11 ] defines knowledge-based economies as those “which are directly based on the production, distribution and use of knowledge and information’’ (p. 7). The World Bank has classified the knowledge economy into four areas: economic and institutional regime, education and skills, information and communication infrastructure, and an innovation system—with the agency going so far as to create a Knowledge Economy Index (KEI) as an indicator of a country’s “preparedness” for a knowledge economy [ 53 ].
Asongu and colleagues [ 54 ] found the overall trends in African countries’ performance between 1996 and 2010 differed across the World Bank’s KEI dimensions: Tunisia led in education, the Seychelles in information and communication technology, South Africa in innovation and Botswana and Mauritius in institutional regime. Oluwatobi and colleagues [ 55 ] have argued that the potential for knowledge production and innovation in Sub-Saharan Africa is mitigated by the level of human capital and quality of institutions. Overall, quality education and strong institutions are held to be imperative for the transformation into a knowledge economy [ 55 , 56 , 57 ]. Both educational and economic institutions may create enabling structures for developing knowledge and innovation and for economic growth, but their influence varies according to institutional arrangements, income and development levels in countries [ 57 , 58 , 59 ]. In particular, education plays a vital role in strengthening human capital, which directly influences the ability to create, absorb, transform, disseminate and use knowledge and innovation [ 55 , 60 , 61 , 62 ]. Education and training emphasizing the value of traditional knowledge and culture also strengthens human capital to innovate contextually relevant solutions for local development problems [ 54 , 59 , 63 ].
The contribution of HSciR
Within the broader remit of science for development, HSciR is vital in its own specific way. HSciR has led to collective human benefit, development of medical treatments, or better understanding of health risks of activities such as tobacco smoking. At a national level, HSciR can also specifically generate evidence that is useful for public service planning and programme implementation. It can provide policy-relevant information, including disease trends, risk factors, outcomes of interventions and patterns of care, as well as health systems and services costs and outcomes [ 64 ].
Grant and Buxton developed a framework to estimate the value that HSciR provides to countries [ 65 ]. Their analysis has included as benefits reduced expenditure on delivering existing services; service and provision delivery improvements; health service effectiveness improvements; greater overall improvements in health and equity with more consideration of allocation of resources and access to provision; and a healthy, performance-driven workforce.
Finally, Dobrow et al. have shown that HSciR evidence can in turn support development of the process of health policy-making through the identification of new issues worthy of bringing to the policy agenda in a particular context, supporting decision-makers in their analyses of policy content and continued direction and policy impact monitoring and evaluation [ 66 ]; Gilson has noted that health policy and systems research more specifically provides insights into how policy decisions are made and the factors affecting successful policy implementation [ 67 ]. In many ways, these examples capture the benefits widely seen to follow from a system of evidence-informed policy-making, whereby a more systematic and robust use of research evidence in decision-making is seen to improve planning effectiveness efficiency and policy implementation to serve the broader social good [ 16 , 68 ].
HSciR input and output by national governments are not uniform, with significant disparities between regions or income levels and also across countries within the same region or at similar levels of income [ 69 , 70 ]. On the African continent, for example, Tanzania and Lesotho had similar levels of GDP per capita (US$ 2365 and US$ 2494, respectively, in 2013); however, the percentage of GDP invested in research in Tanzania was more than three times as high as in Lesotho (0.28 vs 0.08), while the number of publications per million inhabitants was nearly 50 times as high, at 770 in Tanzania compared to 16 in Lesotho [ 71 ].
One of the most critical contextual determinants of HSciR outputs is historical evolution of research systems. For those African nations subject to colonial rule, for instance, modern forms of research were often developed in service to the economic interests of the colonizing power. The focus of research thus centred on key exports such as agriculture-, forestry- and mining-related activity, with little interest in HSciR to benefit local populations [ 72 , 73 ]. After independence, HSciR remained embryonic, with governments often choosing to invest in economies based on the commercialization of cash products and natural resources rather than in the development of research and technology [ 74 ]. Moreover, countries which have experienced conflict, instability and other sociopolitical crises have had to direct resources towards reconstruction and peacekeeping investments, rather than towards scientific research and innovation [ 75 ].
For some nations, the catalyst for investment and development of HSciR has mainly been through the emergence of health crises—new diseases such as HIV/AIDS and Ebola, or the rising incidence of tuberculosis and plague [ 76 , 77 ] (MTN, 2017). Outbreaks have also at times inspired new policies calling for investment in HSciR by global organizations such as WHO and UNESCO [ 78 , 79 ]. These calls for investment have allowed for a more open dialogue and progress on conceptualizing the importance of health research, even within low-income African states—with several governments now committed to investing in scientific research in connection with a country's economic and sustainable development priorities [ 80 , 81 , 82 ]. Despite these shifts, such as the Bamako Initiative, WHO’s efforts to regionalize research efforts and signs of increased attention to domestic HSciR, key drivers of research and research funding in the health sector remain exogenous to African states. Indeed, funding largely reflects global HSciR priorities, with limited options for investigator-initiated research on local health concerns.
How to measure HSciR?
While there is a strong case that HSciR in LMICs is important at national and global levels—for improving health, preventing epidemic spread, supporting health policy and systems and as an influential factor of national development more broadly—there is no single framework or consensus method to assess HSciR capacity across countries. Indicators for measuring and monitoring HSciR generally include standard output indicators of knowledge production and innovation, such as scientific journal articles per million inhabitants or patents per million inhabitants [ 53 ] and input and process indicators of health R&D. Such process indicators can include gross domestic R&D expenditure on health as a percentage of GDP, number of clinical trials per million inhabitants, research grants and full-time equivalent health researcher per million inhabitants [ 35 ]. From the perspective of decision-makers in national agencies, these indicators of knowledge production and human resources for research are helpful for benchmarking performance against regional and global comparators and for informing policy and strategy to strengthen R&D [ 83 ].
Researchers and international organizations have attempted to compile indicators and measure HSciR capacity in different ways. For example, WHO has created a Global Observatory on Health R&D which aims to “consolidate, monitor and analyse relevant information on health research and development activities” [ 84 ]. This uses a logic model perspective to assessing HSciR, tracking a range of indicators to monitor health R&D inputs, processes and outputs as identified and defined by Røttingen and colleagues [ 35 ]. While these indicators are useful for monitoring and benchmarking the state of HSciR and development activities, funding and performance at the national level, they do not provide information to assess the overall capacity of national health research systems as a set of “people, institutions and processes” for HSciR [ 4 ]. Moreover, there are incomplete or missing data for many of these indicators.
A second approach takes a systems perspective to assessing HSciR capacity, recognizing that R&D funds and personnel represent but two components of a nation’s HSciR capacity. Pang and colleagues [ 17 ] defined a national health research system within a conceptual framework considering four key tenets: stewardship, financing, creating and sustaining resources, and producing and using research. This framework has been operationalized under the Research for Health unit at the WHO Regional Office for Africa through the development of a “barometer” that aims to assess the evolution of national health research systems. The team collected data from surveys of individual health research focal points in countries (with rounds in 2003, 2009, 2014 and 2018) [ 85 , 86 , 87 , 88 , 89 ]. Key informants within national ministries of health and other institutions replied to questions about whether HSciR policies, institutions or other resources were currently in place in the country (e.g. national health research policy, national research ethics committee, national health research institute, national budget line for health research) [ 85 ].
In applying this approach, Kirigia and colleagues [ 86 ] analysed trends between 2003 and 2014 to show that although there have been positive gains across many functions, there are still considerable gaps in many African countries. For example, in sub-Saharan Africa, fewer than 50% of countries have a nationwide official health research policy, or a national health research strategy/policy plan, a HSciR law or regulation, or a much-needed budget line for HSciR within the ministry of health. Approximately half of states analysed have a national health research institute/council, a research programme at the governmental level, or an equivalent health research management forum. Public financing for HSciR is also typically measured to be very low, with minimal progress towards the goal of 2% of the national health expenditure allocated to HSciR. Instead, most funds for HSciR come from external sources such as international organizations, nongovernmental organizations (NGOs) or multilateral/bilateral partners. According to Kirigia et al., the weakest elements of African health research systems are human resources for HSciR, government spending on HSciR, publications in peer-reviewed journals, and research institutions to conduct HSciR [ 87 ].
Overall, there have been a variety of attempts to identify key elements of HSciR activity, performance and capacity in Africa. Some have assessed R&D potential, measured funding inputs or identified gaps in national HSciR systems. These efforts shed light on where strengths and weaknesses lie, but currently do not provide a comprehensive review and synthesis of data on which to comparatively evaluate HSciR knowledge and innovation, HSciR and development activities and HSciR systems at the national level across Africa.
The aim of this paper is to build on earlier work by collecting and aggregating data on a range of variables to consider HSciR activity, performance and capacity in all African countries. We develop a framework for evaluating a country’s capacity for HSciR based on publicly available global data sources. This framework incorporates and expands on indicators from previous studies. Using this framework, we present data on HSciR capacity in each of the 54 UN-recognized African states to map current capacity across the region for HSciR—providing one of the first analyses to systematically outline the contribution of African countries to HSciR across such a wide range of indicators.
Data collection
We reviewed data for each of the 54 UN-recognized states in Africa. This excluded any foreign departments (e.g. Mayotte), regions (e.g. Réunion) or territories (e.g. Saint Helena) located in Africa, as well as the disputed territory of Western Sahara. We collected population and gross domestic product (GDP) data from the World Bank [ 90 ] for each of these states to be able to benchmark our findings against broader development metrics.
We sought to identify a range of indicators which could help measure the HSciR capacity in each country. We used the indicators selected by the WHO Global Observatory on Health R&D database as a starting point, which comprised GERD as a proportion of GDP, health researchers per million inhabitants, number of institutions and official development assistance for the medical research and basic health sectors as a proportion of gross national income [ 91 ]. We then supplemented this with others measures of HSciR capacity which we identified through discussions between authors and members of a project oversight committee, Footnote 1 including bibliographic data, data on clinical trial infrastructures, regulatory environment, intellectual property rights and research funding. All data were acquired between June and September 2018.
To classify and conceptualize the various indicators available, we followed the Donabedian [ 92 ] model of healthcare quality measurement to categorize our indicators into one of three types: structural, process and output measures related to HSciR. Structural measures capture inputs into the system and thus comprised metrics such as workforce numbers, budget allocation to R&D and numbers of organizations, regulations and guidelines on human subject protections. Process measures are indicators of ongoing HSciR activities, including numbers of clinical trials registered and patent applications. Finally, output measures capture the outputs of research activities including numbers of peer-reviewed publications and citations for these publications.
Structural indicators
R&d expenditures and personnel.
Data on R&D expenditure and personnel were obtained from the United Nations Educational, Scientific and Cultural Organization (UNESCO) (2016, or the most recent available year) [ 91 ]. We collected data on the number of full-time-equivalent staff in the following categories: (i) R&D personnel (per million inhabitants), (ii) researchers (per million inhabitants) and (iii) researchers with doctoral or equivalent degrees (as a proportion of total number of researchers). From the same database, we also collected data on GERD in current purchasing power parity (PPP) dollars (in thousands); these figures were also shown as a proportion of GDP and per capita. Whenever possible, we collected expenditure and personnel data specific to medical and health sciences.
Research institutions
We collected data on the number of universities in each country, using a list based on information from the International Association of Universities [ 93 ]. We recognize that there may be limitations affecting the quality of data from this source; thus, we also identified the number of African universities listed on the most recent global university rankings of three influential publishers: Quacquarelli Symonds Limited ( QS World University Rankings ) [ 94 ], Times Higher Education ( THE World University Rankings ) [ 95 ] and Shanghai Ranking Consultancy ( Academic Ranking of World Universities ) [ 96 ]. Whilst this may not be comprehensive, it allows an indication of the number of institutions across the continent.
We further collected data on the number of institutional review boards [ 97 ] and WHO Collaborating Centres [ 98 ] in each country and noted whether or not there exists a national ethics committee [ 99 ] and national public health institute [ 100 ].
Research funding
We collected data on international funding awarded to researchers in each country (2008–2017) from the 10 largest public and philanthropic funders of health research globally (listed in order of size) [ 101 ]: (1) United States National Institutes of Health, (2) European Commission, (3) United Kingdom Medical Research Council, (4) French National Institute of Health and Medical Research, (5) United States Department of Defense (including the Congressionally Directed Medical Research Programs), (6) Wellcome Trust, (7) Canadian Institutes of Health Research, (8) Australian National Health and Medical Research Council, (9) Howard Hughes Medical Institute and (10) German Research Foundation.
The data were collected from each funder’s website. As we are seeking to understand current capacity, we only counted funding allocated to researchers based at institutions in African countries. We excluded funding for research projects in which the principal investigators were based at non-African institutions, even if these projects included collaborators, field sites or locations of research in Africa.
Foreign currencies were converted to dollars based on the yearly average exchange rates published by the World Bank [ 90 ]. All amounts were reported in 2018 US dollars based on the United States consumer price index adjustments to account for inflation.
Process indicators (clinical trial infrastructures, intellectual property rights and regulatory capacities)
Data on the numbers of clinical trials and records, as of 4 August 2018, were extracted from the WHO International Clinical Trials Registry Platform (ICTRP) [ 102 ] and United States National Institutes of Health database (ClinicalTrials.gov) [ 103 ]. ClinicalTrials.gov indexes trials of new investigational drugs, whereas the ICTRP indexes data from several sources, including the European Union Clinical Trials Register, ClinicalTrials.gov, International Standard Randomised Controlled Trial Number register and Pan African Clinical Trial Registry. A full list of data providers can be found on the ICTRP website [ 102 ]. The ICTRP registry accepts all types of clinical research studies, including trials of public health interventions.
We also collected information on the number of organizations, regulations and guidelines on human subjects protection in each country. These data, which are collected annually by the United States Department of Health and Human Services [ 104 ], reflect protections in each of the following categories: “general (i.e. applicable to most or all types of human subjects research)”, “drugs and devices”, “clinical trial registries”, “research injury”, “social-behavioural research”, “privacy/data protection”, “human biological materials”, “genetic” and “embryos, stem cells and cloning”. We used the 2018 edition of the compilation of protections [ 104 ].
Finally, we collected data from the World Intellectual Property Organization on the numbers of patents issued to residents in each country (2016, or most recent available year) [ 105 ].
Output indicators (publications and citations)
To systematically collect publication data, we searched Scopus, the largest global peer-reviewed literature abstract and citation database [ 106 ]. Scopus was chosen as it includes a larger volume of non-English-language journals than many other major bibliographic databases (e.g. Web of Science or PubMed/Medline) [ 106 ]. We searched for any articles published in the following Scopus subject areas: health sciences (medicine, nursing, veterinary, dentistry, health professions) and life sciences (agricultural and biological sciences, biochemistry, genetics and molecular biology, immunology and microbiology, neuroscience and pharmacology, toxicology and pharmaceutics). We included the following types of publications: articles, in press, books, chapters and conference papers.
We searched for articles published with at least one author based at an institution in each of the 54 countries, using the “Affiliation country” field in Scopus. We searched the names of each country in English, French and Portuguese, as well as variant spellings of country names. We restricted the searches to publications published in the 10-year period from 2008 to 2017. The search strategy, including the country names, can be found in Additional file 1 .
For each country, we extracted data on the number of publications with at least one author based in the country, as well as the number of publications first authored by a local researcher. We also collected citation data for all articles. For publications published in the 5-year period from 2013 to 2017, we collected data on the proportion of publications with international, institutional and national collaborators; these data were unavailable for articles published before 2013. These data were obtained in SciVal, a research information tool developed by Elsevier to synthesize bibliometric data from Scopus.
Data for each individual indicator are presented as a series of tables in Additional file 2 . We describe findings for each indicator in Additional file 3 , before providing a summary table in this section (see Table 1 ).
Table 1 below presents data for selected indicators. We have shaded each cell to reflect whether the data in that cell fall in the highest, middle or lowest tercile of the range, with green for the top tercile, yellow the middle and orange the bottom. The table shows that while there were some high achievers across the board, the results were varied for most states—suggesting high relative performance in some indicators, but lower in others (or missing data). For example, Libya was a relatively high achiever for publications, first author publications and number of research institutions, but lagged behind this success with the number of clinical trials conducted within the country. Conversely, Burundi had low numbers of publications, first author publications, number of clinical trials and GERD as a percentage of GDP, but performed relatively well in number of research institutions. While many of the higher-income countries unsurprisingly perhaps do well on numerous indicators, some lower-income countries also appear to perform well, such as Senegal or Kenya.
Additional file 2 presents a further set of 10 figures to illustrate associations between various metrics and GDP (gross and per capita). In general, there was a strong positive association between GDP and the various indicators collected. However, there could be significant spread around the linear trend lines plotted, indicating some countries performing particularly well or poorly relative to income level.
Limitations
This study has limitations. First, there is no single indicator for accurately ascertaining HSciR. Accordingly, we used a variety of available metrics that serve as proxy indicators. Thus, there is a risk that these proxies do not capture the full landscape we sought to map. For example, we have not accounted for broader financing and infrastructure which contributes to HSciR—such as buildings, routine access to electricity, and primary and secondary education attainment. Each of these may contribute to a country’s capacity for HSciR, but they may be part of broader development measures. Such indicators may not clearly demonstrate the impact of HSciR and can be difficult to disaggregate. However, there is support for the indicators we selected for our framework from the literature discussing measurement of health R&D globally and in Africa [ 35 , 107 ]. Nevertheless, we acknowledge that there are multiple challenges and issues with measuring HSciR performance using universal indicators in the contexts of African national health research systems [ 108 ].
Second, there are some important limitations of the sources of data used. Given the lack of consistent data on HSciR collected and reported at national levels, or indeed at the regional level, we restricted our searches to global-level data sets to try to ensure some degree of comparability. This approach fails to take into account the reality of what might be occurring within countries which is not reported formally or is not published at the national, regional or global level. Moreover, at the global level there was a lack of data for several indicators, or these data were outdated. The most comprehensive data sources were for publications and clinical trials, but many other indicators were missing results for numerous countries. In some data categories, there were issues of reliability and comparability between sources. Furthermore, while we aimed to collect data from 2007 to 2017, some data points had to come from before this time frame when more recent data were not available. This included data on patent applications and human resources. Ultimately, we decided that including data outside the period was better to get a fuller picture of the HSciR landscape.
Third, for the output indicators, it is important to note that research outputs are not always published in peer-reviewed journals; therefore, limiting the analysis to bibliometrics from SciVal could have led us to outputs in other sources and formats. Our approach does not include research published outside of peer-reviewed journals, including government or nongovernmental literature policy reports, open data sets, software or other grey literature. Scopus also does not index all journals published in African states. Similarly, we recognize that for the structural indicators, we only included universities, which may provide an incomplete picture of key research structures and institutions within a country. While the presence of universities was felt to be a reasonably comparable metric to serve as a proxy for infrastructure capacity, it is known that there are very important contributors to the HSciR landscape in Africa that are not affiliated to a specific university per se—for example, Tanzania’s Ifakara Health Institute, the Kenya Medical Research Institute and the African Population and Health Research Centre (APHRC). These entities undertake a large amount of work at national or regional levels. Indeed, some centres of excellence in Africa may be undertaking a very large share of HSciR in a given country, and not be affiliated with a university. While the activities of such organizations might be captured in publication metrics or clinical trials data, future efforts to evaluate HSciR capacity may need to consider ways to identify, count or compare the importance of centres of excellence as core hubs of institutional capacity [ 40 ].
Fourth, we were unable to find a consistent data source across the African continent to measure government budget allocation to HSciR. Instead, we used GERD as a proxy, which (see Table 1 ) captures investments in R&D (although not disaggregated by health sciences). Furthermore, data on GERD aggregate total expenditure on R&D from the government as well as university, private enterprise and not-for-profit sectors; yet this breakdown is rarely available for many African countries. The data available through internationally recognized and consistent sources on GERD for medical and health sciences are sparse (see Additional file 2 : Table S4). The WHO African Barometer survey collects data on health research budgets, which is self-reported by health research focal points at ministries of health. Data from 2018 reported that 24 countries had a dedicated budget line for health research and that 37 countries regularly tracked health research spending from all sources [ 89 ]. Whilst these data show a limited scope of HSciR funding, taking only the ministry of health budget and not other sources, it could contribute to better understanding of HSciR funding in countries. These data have not been made publicly available by intergovernmental sources, and we found no centralized data on national research funds on the continent in any comparable way, although in-depth qualitative case studies in a sample of nine African countries found these in five instances [ 109 ]. Future work evaluating HSciR could investigate which countries of the region have such funds, as there does not appear to be any data source indicating it at present despite a nascent literature on the topic [ 110 , 111 , 112 , 113 ]. Similarly, when measuring the number of universities in each state, we were not able to ascertain whether these universities undertake research or solely offer degrees or training in health sciences.
Fifth, these metrics are all aggregated at the national level, and thus this crude analysis fails to reveal any subnational interaction. A more in-depth analysis could reveal particular “hubs” of excellence, as well as institutional capacity or individual capacities which form key components of the national landscape.
Taken as a whole, the existing data we were able to analyse offer a nuanced view of current HSciR on the African continent. We hope that such mapping facilitates governments and international organizations in identifying gaps in HSciR capacity, particularly in comparison to other countries in the region, if important. Our findings importantly also highlight gaps where more data are very much needed. These data can help to inform investment priorities and future system needs.
Our findings have raised several issues for consideration:
There are some unsurprising high performers across the variety of indicators, such as South Africa, Egypt and Tunisia, which score highly across most metrics. However, it is worth noting that it is not simply the level of development (GDP) or international or national financing for HSciR (GERD and international research funding) that leads to success in HSciR. Nations which have had major donor investment in HSciR (per capita), including Uganda and Gambia, have not necessarily emerged as top performers across the range of proxy indicators used. Whilst the current level of economic development does not appear to play a significant role in a country’s HSciR capacity per se, our analysis shows a clear correlation between GDP and a range of individual metrics (Additional file 2 ), although this is not evidence of causality).
There are several possible explanations for these results. One explanation might be that reliance on donor funding has limited the sustainability of the health research sector when these collaborations end [ 114 , 115 ], or that donor investment focused on projects which lacked significant improvements in broader infrastructures within the national system. Alternatively, international arrangements may result in research agendas set by the Global North, which could imply that they either reflect the needs of the funding location [ 116 , 117 ], a focus on spotlight issues [ 118 ] or so-called parachute research [ 119 , 120 ] and bypass local research institutions and expertise [ 121 ], any of which may be limited in improving health research outcomes or capacity in the host location. The importance of local research development, however, has been highlighted as vital to building a knowledge economy and addressing domestic health concerns, as in-country researchers have the best understanding of the national agenda and cultural context which increased the likelihood of evidence uptake by policy-makers [ 22 , 122 ]. Yet, it is clear that several African governments have not met the commitment to ensure that 1% GDP is dedicated to research, and many have struggled to make even minimal investments in HSciR from public finances, being more reliant on international donors or private entities.
Another explanation is that using these indicators to measure performance does not capture the nuance of what is occurring within each system, particularly within each nation and the progress that research systems are making more holistically. For example, these metrics are not able to infer political commitment to HSciR, the relative importance of the HSciR landscape globally, how national systems have developed, where the success stories are and where barriers remain to solidifying knowledge economies. They are also unable to infer the historical contexts which led to the development of these systems, whether rooted in colonial science or postcolonial investments, each of which will lead to different-looking HSciR environments.
Moreover, there is a paucity of national data provided by governments across the African continent in the public domain. This was a notable gap and challenge for assessing the landscape of HSciR across the region. There may be few incentives in place to do so, but it would be important for governments to make more national-level data available for future studies. This would allow future research to provide a realistic picture of HSciR within each nation and thus be able to make meaningful assessments of country capacity or areas for future investment. Our hope is that with this mapping exercise, whilst limited to global data sources, governments will be able to identify where their gaps in HSciR lie, or their perceived relative performance compared to regional counterparts. This may offer meaningful analysis for investment priorities and future health research system needs.
There has been a growing awareness of the importance of building health research systems in lower-income settings over time, whether it is to provide useful evidence to inform policy and health systems performance, to develop so-called knowledge economies that support economic growth, or to ensure that there are research systems in place that can assist countries in responding to emergent and novel epidemic threats such as COVID-19. A range of stakeholders, including national governments, international donor agencies and global health policy-making bodies, may all be increasingly interested in ways to evaluate HSciR to guide future developments. We have sought to assess current capacity for HSciR across Africa based on a subset of proxy indicators for which we had more complete data considering structural, process and output indicators. In doing so, we contribute to quantifying current strengths and lack of capacity in the HSciR landscape. Importantly, we did not find particular differential trends between these indicators. Some countries performed well across all three types of indicators, with variation amongst those performing less well as to where strengths lay— there were some locations which had stronger output indicators, but this did not necessarily correlate to strong process and structural drivers, and vice versa.
Availability of data and materials
All data generated or analysed during this study are included in this published article and its additional information files.
This project oversight group comprised funders, researchers and policy officers based in Kenya, Ghana, South Africa, the United States and the United Kingdom, and was convened by Wellcome Trust.
Abbreviations
African Population and Health Research Centre
Gross domestic product
Gross domestic expenditure on R&D
- Health sciences research
International Clinical Trials Registry Platform
Knowledge Economy Index
Low- and middle-income countries
Purchasing power parity
Research and development
United Nations Educational, Scientific and Cultural Organization
Bates I, Akoto AYO, Ansong D, Karikari P, Bedu-Addo G, Critchley J, et al. Evaluating health research capacity building: an evidence-based tool. PLOS Med. 2006;3(8): e299. https://doi.org/10.1371/journal.pmed.0030299 .
Article PubMed PubMed Central Google Scholar
UK Clinical Research Collaboration. Health Research Classification System. 2018. http://www.hrcsonline.net/ .
Foundation ES. Health research classification systems—current approaches and future recommendations. Science Policy Briefing. 2011. http://archives.esf.org/publications/science-policy-briefings.html .
Commission on Health Research for Development. Health research: essential link to equity in development. New York: Oxford University Press; 1990.
Google Scholar
Global Forum for Health Research. The 10/90 report on health research 2000. Geneva: Switzerland; 2000.
World Health Organization. World Health Report 2013: Research for Universal Health Coverage. Geneva, Switzerland; 2013. https://www.who.int/whr/2013/report/en/ .
Duermeijer C, Amir M, Schoombee L. Africa generates less than 1% of the world’s research; data analytics can change that. Elsevier Connect. 2018. https://www.elsevier.com/connect/africa-generates-less-than-1-of-the-worlds-research-data-analytics-can-change-that . Accessed 17 Oct 2020.
African Union Commission. Science, Technology and Innovation Strategy for Africa 2024 (STISA-2024). Addis Ababas, Ethiopia; 2014.
World Health Organization Regional Office for Africa. Research for Health: a Strategy for the African Region 2016–2025, Report of the Secretariat. N’Djamena, Republic of Chad; 2015. https://www.who.int/evidence/africanregionstrategy.pdf?ua=1 .
The World Bank, Elsevier. A decade of development in sub-Saharan African science, technology, engineering and mathematics research. Washington, D.C.; 2014. http://documents.worldbank.org/curated/en/237371468204551128/A-decade-of-development-in-sub-Saharan-African-science-technology-engineering-and-mathematics-research .
Organisation for Economic Co-operation and Development. The knowledge-based economy. Paris: OECD; 1996.
Organisation for Economic Co-operation and Development. Integrating science and technology into development policies. Paris, France: OECD Publishing; 2007. 288 p. https://www.oecd-ilibrary.org/science-and-technology/integrating-science-technology-into-development-policies_9789264032101-en .
Organisation for Economic Co-operation and Development. International Science and Technology Co-operation. Paris, France: OECD; 2001. https://www.oecd-ilibrary.org/environment/international-science-and-technology-co-operation_9789264192348-en .
McKee M, Stuckler D, Basu S. Where there is no health research: what can be done to fill the global gaps in health research? PLOS Med. 2012;9(4): e1001209. https://doi.org/10.1371/journal.pmed.1001209 .
Fonn S. African PhD research capacity in public health: raison d’être and how to build it. In: Matlin S, editor. Global forum update on research for health. Geneva: Global Forum for Health Research Pro-book Publishing Limited; 2006. p. 80–3.
Agyepong IA, Sewankambo N, Binagwaho A, Coll-Seck AM, Corrah T, Ezeh A, et al. The path to longer and healthier lives for all Africans by 2030: the Lancet Commission on the future of health in sub-Saharan Africa. Lancet. 2017;390(10114):2803–59. https://doi.org/10.1016/S0140-6736(17)31509-X .
Article PubMed Google Scholar
Pang T, Sadana R, Hanney S, Bhutta ZA, Hyder AA, Simon J. Knowledge for better health: a conceptual framework and foundation for health research systems. Bull World Health Organ. 2003;81(11):815–20.
PubMed Google Scholar
Bates I, Boyd A, Aslanyan G, Cole DC. Tackling the tensions in evaluating capacity strengthening for health research in low- and middle-income countries. Health Policy Plan. 2015;30(3):334–44. https://doi.org/10.1093/heapol/czu016 .
World Health Organization. World health report 2006: working together for health. Geneva, Switzerland; 2006. https://www.who.int/whr/2006/en/ .
Ahen F, Salo-Ahen OMH. Governing pharmaceutical innovations in Africa: inclusive models for accelerating access to quality medicines. Cogent Med. 2018;5(1):1–22. https://doi.org/10.1080/2331205X.2018.1500196 .
Article Google Scholar
World Health Organization & UNICEF/UNDP/World Bank/WHO Special Programme for Research and Training in Tropical Diseases. Global report for research on infectious diseases of poverty 2012. Geneva, Switzerland; 2012. 168 p. https://apps.who.int/iris/handle/10665/44850 .
Franzen SRP, Chandler C, Lang T. Health research capacity development in low and middle income countries: reality or rhetoric? A systematic meta-narrative review of the qualitative literature. BMJ Open. 2017;7(1): e012332. https://doi.org/10.1136/bmjopen-2016-012332 .
Mony PK, Kurpad A, Vaz M. Capacity building in collaborative research is essential. BMJ. 2005;331(7520):843.3-844. https://doi.org/10.1136/bmj.331.7520.843-b .
Costello A, Zumla A. Moving to research partnerships in developing countries. BMJ. 2000;321(7264):827–9. https://doi.org/10.1136/bmj.321.7264.827 .
Article CAS PubMed PubMed Central Google Scholar
International Vaccines Task Force. Money and microbes: strengthening clinical research capacity to prevent epidemics. Washington, D.C.; 2018.
Bloomfield GS, Baldridge A, Agarwal A, Huffman MD, Colantonio LD, Bahiru E, et al. Disparities in cardiovascular research output and citations from 52 African countries: a time-trend, bibliometric analysis (1999–2008). J Am Heart Assoc. 2015. https://doi.org/10.1161/JAHA.114.001606 .
Ettarh R. Patterns of international collaboration in cardiovascular research in sub-Saharan Africa. Cardiovasc J Afr. 2016;27(3):194–200. https://doi.org/10.5830/CVJA-2015-082 .
Adedokun BO, Olopade CO, Olopade OI. Building local capacity for genomics research in Africa: recommendations from analysis of publications in Sub-Saharan Africa from 2004 to 2013. Glob Health Action. 2016;9:31026. https://doi.org/10.3402/gha.v9.31026 .
Hernandez-Villafuerte K, Li R, Hofman KJ. Bibliometric trends of health economic evaluation in Sub-Saharan Africa. Glob Health. 2016;12(1):50. https://doi.org/10.1186/s12992-016-0188-2 .
Adam T, Ahmad S, Bigdeli M, Ghaffar A, Røttingen J-A. Trends in health policy and systems research over the past decade: still too little capacity in low-income countries. PLoS ONE. 2011;6(11): e27263. https://doi.org/10.1371/journal.pone.0027263 .
Gilson L, Raphaely N. The terrain of health policy analysis in low and middle income countries: a review of published literature 1994–2007. Health Policy Plan. 2008;23(5):294–307. https://doi.org/10.1093/heapol/czn019 .
Uthman OA. Pattern and determinants of HIV research productivity in sub-Saharan Africa: bibliometric analysis of 1981 to 2009 PubMed papers. BMC Infect Dis. 2010;10(1):47. https://doi.org/10.1186/1471-2334-10-47 .
Breugelmans JG, Makanga MM, Cardoso ALV, Mathewson SB, Sheridan-Jones BR, Gurney KA, et al. Bibliometric assessment of European and Sub-Saharan African research output on poverty-related and neglected infectious diseases from 2003 to 2011. PLoS Negl Trop Dis. 2015;9(8): e0003997. https://doi.org/10.1371/journal.pntd.0003997 .
Chuang K-Y, Chuang Y-C, Ho M, Ho Y-S. Bibliometric analysis of public health research in Africa: the overall trend and regional comparisons. S Afr J Sci. 2011;107(5/6):54–9. https://doi.org/10.4102/sajs.v107i5/6.309 .
Rottingen JA, Regmi S, Eide M, Young AJ, Viergever RF, Ardal C, et al. Mapping of available health research and development data: what’s there, what’s missing, and what role is there for a global observatory? Lancet. 2013;382(9900):1286–307. https://www.thelancet.com/journals/lancet/article/PIIS0140-6736(13)61046-6/fulltext
Uthman OA, Uthman MB. Geography of Africa biomedical publications: an analysis of 1996–2005 PubMed papers. Int J Health Geogr. 2007;6(1):46. https://doi.org/10.1186/1476-072X-6-46 .
Uthman OA, Wiysonge CS, Ota MO, Nicol M, Hussey GD, Ndumbe PM, et al. Increasing the value of health research in the WHO African Region beyond 2015—reflecting on the past, celebrating the present and building the future: a bibliometric analysis. BMJ Open. 2015;5(3): e006340. https://doi.org/10.1136/bmjopen-2014-006340 .
AOSTI. Assessment of scientific production in the African Union, 2005–2010. Malabo, Equatorial Guinea; 2013.
Allard G. Science and technology capacity in Africa: a new index. J Afr Stud Dev. 2015;7(6):137–47. https://doi.org/10.5897/JASD2014.0322 .
Nwaka S, Ochem A, Besson D, Ramirez B, Fakorede F, Botros S, et al. Analysis of pan-African Centres of excellence in health innovation highlights opportunities and challenges for local innovation and financing in the continent. BMC Int Health Hum Rights. 2012;12(1):11. https://doi.org/10.1186/1472-698X-12-11 .
Schmalzbauer B, Visbeck M. The contribution of science in implementing the sustainable development goals. German Committee Future Earth. 2016. www.dkn-future-earth.org .
Allen RC. Explaining the British industrial revolution from the perspective of global wage and price history. Oxford: Oxford University; 2006. p. 1–30.
The Industrial Age—vaccine research leaps forward. Carrington College. 2015. https://carrington.edu/blog/the-industrial-age-vaccine-research-leaps-forward/ .
Bochove CJ van. The economic consequences of the Dutch: economic integration around the North Sea 1500–1850. Utrecht University; 2008.
Sumner A, Tribe M. International development studies: theories and methods in research and practice. London: SAGE Publications Ltd; 2008. http://sk.sagepub.com/books/international-development-studies
Georgalakis J. Is it time to stop talking about research uptake? Institute of Development Studies; 2017.
Kates RW, Clark WC, Corell R, Hall JM, Jaeger CC, Lowe I, et al. Sustainability science. Science (80-). 2001;292(5517):641–2. https://science.sciencemag.org/content/292/5517/641 .
UNDP. Making new technologies work for human development. Human Development Report 2001. New York: Oxford University Press; 2001. http://hdr.undp.org/en/content/human-development-report-2001 .
World Bank. World Development Report 1999/2000: Entering the 21st century. New York: Oxford University Press; 1999. http://hdl.handle.net/10986/5982 .
UN General Assembly. Transforming our world: the 2030 Agenda for sustainable development. 2015. https://www.un.org/ga/search/view_doc.asp?symbol=A/RES/70/1&Lang=E .
Molla T. Re-imagining Africa as a knowledge economy: premises and promises of recent higher education development initiatives. J Asian Afr Stud. 2018;53(2):250–68.
Obamba MO. Uncommon knowledge: World Bank policy and the unmaking of the knowledge economy in Africa. High Educ Policy. 2013;26(1):83–108.
World Bank. Measuring knowledge in the world’s economies: knowledge assessment methodology and the knowledge economy index. Washington, D.C.: The World Bank Institute; 2008.
Asongu SA, Tchamyou VS, Acha-Anyi PN. Who is who in knowledge economy in Africa? J Knowl Econ. 2018. https://doi.org/10.1007/s13132-018-0547-8 .
Oluwatobi S, Olurinola I, Alege P, Ogundipe A. Knowledge-driven economic growth: the case of Sub-Saharan Africa. Contemp Soc Sci. 2018. https://doi.org/10.1080/21582041.2018.1510135 .
Babatunde MA. Africa’s growth and development strategies: a critical review. Africa Dev/Afrique Développement. 2012;37(4):141–78. http://www.jstor.org/stable/afrdevafrdev.37.4.141 .
Nour SSOM. Regional systems of innovation and economic structure in the Arab Region. J Knowl Econ. 2014;5(3):481–520. https://doi.org/10.1007/s13132-014-0196-5 .
Lee K, Kim B-Y. Both institutions and policies matter but differently for different income groups of countries: determinants of long-run economic growth revisited. World Dev. 2009;37(3):533–49 http://www.sciencedirect.com/science/article/pii/S0305750X08002301 .
Chi-ang LB. A new vision of the knowledge economy. J Econ Surv. 2007;21(3):553–84. https://doi.org/10.1111/j.1467-6419.2007.00514.x .
Kaur M, Singh L. Knowledge in the economic growth of developing economies. Afr J Sci Technol Innov Dev. 2016;8(2):205–12. https://doi.org/10.1080/20421338.2016.1147207 .
Britz JJ, Lor PJ, Coetzee IEM, Bester BC. Africa as a knowledge society. Int Inf Libr Rev. 2006;38(1):25–40. https://doi.org/10.1080/10572317.2006.10762700 .
Kamara AB, Bousrih L, Nyende M. Growing a knowledge-based economy: evidence from public expenditure on education in Africa. Economic Research Working Paper Series. Tunis, Tunisia: African Development Bank; 2008.
Building knowledge economies: advanced strategies for development. WBI Development Studies. Washington, D.C.: The International Bank for Reconstruction and Development / The World Bank; 2007.
Nass SJ, Levit LA, Gostin LO, editors. The value, importance, and oversight of health research. In: Beyond the HIPAA privacy rule: enhancing privacy, improving health through research. Washington, DC: The National Academies Press; 2009. p. 111–52.
Hanney SR, Grant J, Wooding S, Buxton MJ. Proposed methods for reviewing the outcomes of health research: the impact of funding by the UK’s “Arthritis Research Campaign.” Health Res Policy Syst. 2004. https://doi.org/10.1186/1478-4505-2-4 .
Dobrow MJ, Goel V, Upshur REG. Evidence-based health policy: context and utilisation. Soc Sci Med. 2004;58(1):207–17.
Gilson L, editor. Health policy and systems research: a methodology reader. Geneva: Alliance for Health Policy and Systems Research, World Health Organization; 2012. 472 p. https://www.who.int/alliance-hpsr/resources/reader/en/ .
Weiss CH. The many meanings of research utilization. Public Adm Rev . 1979;39(5). https://sites.ualberta.ca/~dcl3/KT/PublicAdministration Review_Weiss_Themanymeaningsofresearch_1979.pdf.
UNESCO. Data for the sustainable development goals. 2019.
Stange K, Glasgow R. Considering and reporting important contextual factors in research on the patient-centered medical home. Rockville, MD; 2013. (PCMH Research Methods Series). Report No.: 13-0045-EF.
Kraemer-Mbula E, Scerri M. Southern Africa. In: UNESCO science report: towards 2030. Paris: UNESCO Publishing; 2015. p. 535–65.
Gaillard J. Le système national de recherche scientifique et technique à Madagascar. 2015.
Khelfaoui H. La science en Côte d’Ivoire. Waast R, Gaillard J, editors. Paris; 2000.
Kouici S. Les indicateurs de recherche entre référentiels internationaux et contexte national. Rev d’Information Sci Tech. 2018;21(2).
Ministère du Plan et du Développement. Plan National de Développement PND 2016-2020: Diagnostic stratégique de la Côte d’Ivoire sur la Trajectoire de l’Emergence. Abidjan; 2016.
Ministère de la Santé Publique République de Madagascar. Plan du Développement du Secteur Santé 2015–2019. Antananarivo; 2015.
Ministère de la Santé Publique République de Madagascar. Plan Directeur de Lutte Contre Les Maladies Tropicales Négligées (MTN) 2016–2020. Antananarivo; 2017.
OMS Bureau Régional de l’Afrique. Déclaration d’Alger sur la recherche pour la santé dans la région Africaine. 2008.
Essegbey G, Diaby N, Konte A. West Africa. In: UNESCO science report: towards 2030. UNESCO Publishing; 2015.
Ministère de l’Enseignement Supérieur et la Recherche Scientifique. La Stratégie Nationale de la Recherche. Antananarivo: République de Madagascar; 2013.
Ministère du Plan et du Développement. Plan National de Développement PND 2016–2020: Orientations Stratégiques. Abidjan: République de Côte d’Ivoire; 2016.
Ministère de la Santé Publique République de Madagascar. Politique nationale de recherche en santé Madagascar. Antananarivo; 2016.
Blankley WO, Booyens I. Building a knowledge economy in South Africa. S Afr J Sci. 2010. https://doi.org/10.4102/sajs.v106i11/12.373 .
Terry RF, Salm JF, Nannei C, Dye C. Creating a global observatory for health research and development. Science (80- ). 2014;345(6202):1302–4. http://science.sciencemag.org/content/sci/345/6202/1302.full.pdf .
Kirigia JM, Wambebe C. Status of national health research systems in ten countries of the WHO African Region. BMC Health Serv Res. 2006;6(1):135. https://doi.org/10.1186/s12961-015-0054-3 .
Kirigia JM, Ota MO, Motari M, Bataringaya JE, Mouhouelo P. National health research systems in the WHO African Region: current status and the way forward. Health Res Policy Syst. 2015;13(1):61. https://doi.org/10.1186/s12961-015-0054-3 .
Kirigia JM, Ota MO, Senkubuge F, Wiysonge CS, Mayosi BM. Developing the African national health research systems barometer. Health Res Policy Syst. 2016;14(1):53. https://doi.org/10.1186/s12961-016-0121-4 .
Mbondji PE, Kebede D, Zielinski C, Kouvividila W, Sanou I, Lusamba-Dikassa P-S. Overview of national health research systems in sub-Saharan Africa: results of a questionnaire-based survey. J R Soc Med. 2014;107(suppl_1):46–54. https://doi.org/10.1177/0141076814530600 .
Rusakaniko S, Makanga M, Ota MO, Bockarie M, Banda G, Okeibunor J, et al. Strengthening national health research systems in the WHO African Region—progress towards universal health coverage. Glob Health. 2019;15(1):50. https://doi.org/10.1186/s12992-019-0492-8 .
The World Bank. Open Data. 2018. https://data.worldbank.org .
UNESCO. UIS Statistics (category: science, technology, and innovation). 2018. http://data.uis.unesco.org .
Donabedian A. Evaluating the quality of medical care. Milbank Q. 2005;83:691–729.
Förster K. Universities Worldwide. 2018. https://univ.cc .
QS World University. Worldwide university rankings, guides and events. 2018.
Times Higher Education. Academic & University News. 2018. https://www.timeshighereducation.com .
Shanghai Ranking Consultancy. ARWU World University Rankings 2018. 2018. http://www.shanghairanking.com .
Council on Health Research for Development. Regulation and ethics review of research. 2018.
World Health Organization. WHO collaborating centres database and portal. 2018. https://www.who.int/collaboratingcentres/database/en/ .
World Health Organization. National Ethics Committees Database. 2018. https://apps.who.int/ethics/nationalcommittees/Default.aspx .
The International Associaton of National Public Health Institutes. Our Members - IANPHI . 2018. https://www.ianphi.org/about/member-countries.html .
Viergever RF, Hendriks TCC. The 10 largest public and philanthropic funders of health research in the world: what they fund and how they distribute their funds. Health Res Policy Syst. 2016;14(1):12. https://doi.org/10.1186/s12961-015-0074-z .
International Clinical Trials Registry Platform. Trial list by countries. 2018. https://www.who.int/ictrp/en/ .
U.S. National Library of Medicine. ClinicalTrials.gov. 2000. Clinicaltrials.gov.
U.S. Department of Health and Human Services. International Compilation of Human Research Standards. Washington, D.C.; 2018.
World Intellectual Property Organization. WIPO—International and National Patent Collections. 2019. https://patentscope.wipo.int/search/en/search.jsf . Accessed 4 Dec 2020.
Burnham JF. Scopus database: a review. Biomed Digit Libr. 2006;3(1):1. https://doi.org/10.1186/1742-5581-3-1 .
Simpkin V, Namubiru-Mwaura E, Clarke L, Mossialos E. Investing in health R&D: where we are, what limits us, and how to make progress in Africa. BMJ Glob Health. 2019;4(2): e001047. https://doi.org/10.1136/bmjgh-2018-001047 .
Mijumbi-Deve R, Parkhurst J, Jones CM, Juma PA, Sobngwi-Tambekou JL, Wenham C. Beyond the metrics of health research performance in African countries. BMJ Glob Heatlh. 2021;6: e006019.
Jones CM, Ankotche A, Canner E, Habboubi F, Hadis M, Hedquist A, et al. Strengthening national health research systems in Africa: lessons and insights from across the continent. London: LSE Health; 2021. https://doi.org/10.6084/m9.figshare.14039807
Chataway J, Dobson C, Daniels C, Byrne R, Hanlin R, Tigabu A. Science granting councils in Sub-Saharan Africa: trends and tensions. Sci Public Policy. 2019;46(4):620–31. https://doi.org/10.1093/scipol/scz007 .
Mouton J. Science-granting councils in Sub-Saharan Africa: a typology of diverse science funding configurations. In: Arvanitis R, O’Brien D, editors. The transformation of research in the south: policies and outcomes. Marseille: IRD Éditions; 2019. p. 13–23. https://books.openedition.org/irdeditions/32897 .
Gaillard J, Van Lill M, Mouton J. Functions of science granting councils in sub Sahara Africa. In: Cloete N, Maassen P, Bailey T, editors. Knowledge production and contradictory functions in African higher education. African Minds; 2015. p. 148–70.
Tigabu A, Khaemba W. Science Granting Councils in Africa: catalysts of innovation for sustainable development? In: Hanlin R, Tigabu AD, Sheikheldin G, editors. Building science systems in Africa. Nairobi: ACTS Press; 2020.
Gulland A. Plan to stimulate research in developing countries is put on hold. BMJ. 2012;344(may28.3):e3771–e3771. https://doi.org/10.1136/bmj.e3771 .
Annerstedt J, Liyanage S. Challenges when shaping capabilities for research: Swedish support to bilateral research cooperation with Sri Lanka and Vietnam, 1976–2006, and a look ahead. Sweden: Stockholm; 2008.
Kok MO, Rodrigues A, Silva AP, de Haan S. The emergence and current performance of a health research system: lessons from Guinea Bissau. Health Res Policy Syst. 2012;10(1):5. https://doi.org/10.1186/1478-4505-10-5 .
Sitthi-Amorn C, Somrongthong R. Strengthening health research capacity in developing countries: a critical element for achieving health equity. BMJ. 2000;321(7264):813–7. https://doi.org/10.1136/bmj.321.7264.813 .
Coloma J, Harris E. From construction workers to architects: developing scientific research capacity in low-income countries. PLoS Biol. 2009;7(7): e1000156. https://doi.org/10.1371/journal.pbio.1000156 .
Health TLG. Closing the door on parachutes and parasites. Lancet Glob Health. 2018;6(6): e593. https://doi.org/10.1016/S2214-109X(18)30239-0 .
Yozwiak NL, Happi CT, Grant DS, Schieffelin JS, Garry RF, Sabeti PC, et al. Roots, not parachutes: research collaborations combat outbreaks. Cell. 2016;166(1):5–8. https://doi.org/10.1016/j.cell.2016.06.029 .
Erondu NA, Aniebo I, Kyobutungi C, Midega J, Okiro E, Okumu F. Open letter to international funders of science and development in Africa. Nat Med. 2021;27(5):742–4. https://doi.org/10.1038/s41591-021-01307-8 .
Article CAS PubMed Google Scholar
Aksoy S. Solutions to neglected tropical diseases require vibrant local scientific communities. PLoS Negl Trop Dis. 2010;4(3): e662. https://doi.org/10.1371/journal.pntd.0000662 .
Download references
Acknowledgements
We thank Aaron Hedquist and Emily Canner for their research assistance with finalizing this manuscript.
Funding for this research was provided by Wellcome Trust under a commissioned project “Building the Case for Investment in Health Sciences Research in Africa”.
Author information
Authors and affiliations.
Department of Health Policy, LSE, Houghton Street, London, WC2A 2AE, United Kingdom
Clare Wenham, Olivier Wouters & Justin Parkhurst
LSE Health, LSE, Houghton Street, London, WC2A 2AE, United Kingdom
Catherine Jones, Pamela A. Juma, Rhona M. Mijumbi-Deve & Joëlle L. Sobngwi-Tambekou
The Center for Rapid Evidence Synthesis, College of Health Sciences, Makerere University, Kampala, Uganda
Rhona M. Mijumbi-Deve
Africa Center for Evidence, University of Johannesburg, Johannesburg, South Africa
RSD Institute (Recherche-Santé & Développement), Yaounde, Cameroon
Joëlle L. Sobngwi-Tambekou
You can also search for this author in PubMed Google Scholar
Contributions
CW and JP conceptualized and developed the research. CW drafted the manuscript. OW collected and analysed the data. CMJ, PAJ, RM and JST all contributed to the manuscript draft and conversations reflected in the analysis. All authors have read and approved the final manuscript.
Corresponding author
Correspondence to Clare Wenham .
Ethics declarations
Ethics approval and consent to participate.
Not applicable.
Consent for publication
Competing interests.
The authors declare that they have no competing interests.
Additional information
Publisher's note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1..
Search strategy and terms.
Additional file 2: Table S1.
Bibliometric data. Table S2. Clinical trial infrastructures and intellectual property rights. Table S3. R&D personnel. Table S4. R&D expenditure. Table S5. Regulatory capacities. Table S6. Funding. Table S7. Regression summary for gross domestic product and number of publications. Figure S1. The relationship between gross domestic product and publications. Figure S2. The relationship between gross domestic product per capita and publications per capita. Table S8. Regression summary for gross domestic product per capita and the number of publications per capita. Figure S3. The relationship between gross domestic product and patent applications. Table S9. Regression summary for gross domestic product and patent applications. Figure S4. The relationship between gross domestic product per capita and patent applications per capita. Table S10. Regression summary for gross domestic product per capita and patent applications per capita. Figure S5. The relationship between gross domestic product and GERD. Table S11. Regression summary for gross domestic product and GERD. Figure S6. The relationship between gross domestic product per capita and GERD per capita. Table S12. Regression summary for gross domestic product per capita and GERD per capita. Figure S7. The relationship between gross domestic product and universities. Table S13. Regression summary for gross domestic product and universities. Figure S8. The relationship between gross domestic product per capita and universities per capita. Table S14. Regression summary for gross domestic product per capita and universities per capita. Figure S9. The relationship between gross domestic product and clinical trials. Table S15. Regression summary for gross domestic product and clinical trials. Figure S10. The relationship between gross domestic product per capita and clinical trials per capita. Table S16. Regression summary for gross domestic product per capita and clinical trials per capita.
Additional file 3.
Description of Additional file 2 Tables S1–S6.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Wenham, C., Wouters, O., Jones, C. et al. Measuring health science research and development in Africa: mapping the available data. Health Res Policy Sys 19 , 142 (2021). https://doi.org/10.1186/s12961-021-00778-y
Download citation
Received : 11 March 2021
Accepted : 15 September 2021
Published : 11 December 2021
DOI : https://doi.org/10.1186/s12961-021-00778-y
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
Health Research Policy and Systems
ISSN: 1478-4505
- Submission enquiries: Access here and click Contact Us
- General enquiries: [email protected]
- Frontiers in Public Health
- Environmental health and Exposome
- Research Topics

Public Health in Africa: Role of Nutrition and Environment
Total Downloads
Total Views and Downloads
About this Research Topic
Many African countries are struggling to improve and protect the health of their population, which is a major challenge to the social and economic development of the continent. Countries are still grappling with major public health challenges such as access to safe drinking water, access to basic sanitation, ...
Keywords : Africa, nutrition, environment
Important Note : All contributions to this Research Topic must be within the scope of the section and journal to which they are submitted, as defined in their mission statements. Frontiers reserves the right to guide an out-of-scope manuscript to a more suitable section or journal at any stage of peer review.
Topic Editors
Topic coordinators, recent articles, submission deadlines, participating journals.
Manuscripts can be submitted to this Research Topic via the following journals:
total views
- Demographics
No records found
total views article views downloads topic views
Top countries
Top referring sites, about frontiers research topics.
With their unique mixes of varied contributions from Original Research to Review Articles, Research Topics unify the most influential researchers, the latest key findings and historical advances in a hot research area! Find out more on how to host your own Frontiers Research Topic or contribute to one as an author.

CGIAR RESEARCH INITIATIVES
Ilri is actively engaged in several cgiar initiatives and platforms..
- Climate adaptation and mitigation
- Environmental health and biodiversity
- Gender, equality, youth and social inclusion
- Nutrition, health and food security
- Poverty reduction, livelihoods and jobs
- Research compliance
- Communication and knowledge management
- Intellectual property and legal unit
- Data and research methods
- Animal and human health
- Feed and forage development
- Livestock genetics
- Policies, institutions and livelihoods
- Sustainable livestock systems
- Impact at scale
- CGIAR research initiatives
- Capacity development
- Centre for tropical livestock genetics and health
- ILRI Genebank
- Kapiti research station
- Mazingira centre
- One health centre
- Poultry facility
- The CGIAR AMR hub
- Bioscience facility
- Genomics platform

International Land Coalition Rangelands Initiative: Making rangelands secure

ACTIVE Feb 2028
Emerging public health threats in africa’s drylands.
- Burkina Faso
- Explore our work in the countries
- ILRI in the media

Policies and Design Processes to Enable Transformation
- Pereira, Laura
- Vrettos, Chris
- Cramer, Laura K.
- Drimie, Scott
- Muiderman, Karlijn
- Schapendonk, Frans
- Stringer, Lindsay C.
- Veeger, Marieke
- Vervoort, Joost M.
- Wamukoya, George

Opportunities to quantify resilience of dairy cattle to environmental stressors in Sub-Saharan Africa
- Oloo, Richard Dooso
- Ekine-Dzivenu, Chinyere C.
- Ojango, Julie M.K.
- Gebreyohanes, Gebregziabher
- Mrode, Raphael A.
- Okeyo Mwai, Ally
- Chagunda, Mizeck G.G.
- Publications
- Journal articles
- Presentations
- Infographics
- Browse archive

Goal The goal of the project is to mitigate threats of vector-borne diseases in Mandera, Marsabit, Samburu and Turkana counties of northern Kenya. Overview Pastoralism is an important livelihood activity in the arid lands of northern Kenya. These lands also provide a natural habitat for a variety of wildlife species and rivers provide water resources upon which wildlife, livestock and people depend.
Zoonotic pathogens also circulate in this habitat, with biting vectors such as mosquitoes and ticks spreading infection from wildlife to livestock and people. As a result, pastoral communities are at high risk from emerging infectious diseases.
This project aims to understand how ecological, epidemiological and socio-demographic factors in northern Kenya converge for people and animals to be at risk of emerging pathogens.
The project also aims to develop capacity to prevent and respond to vector-borne disease threats through improved surveillance, detection and control measures. The project uses a multi-layered approach to study and develop tools to address the vector-borne pathogens that cause Rift Valley fever, Crimean-Congo haemorrhagic fever and tularaemia.
Through co-funding, the project will support up to 10 PhD students. Expected outcomes
- A dataset to identify and communicate measures that can be taken to reduce people’s risk of exposure to zoonotic pathogens.
- Modelling tools that will allow public health officials to make accurate, real-time forecasts of disease threats.
Partners George Mason University Georgetown University Kenya Medical Research Institute Smithsonian Institution Turkana Basin Institute University of Liverpool University of Milan University of Nairobi US Army Medical Research Institute of Infectious Diseases Walter Reed Biosystematics Unit Zoological Society of London Zoonotic Disease Unit, Kenya
- animal diseases
- animal health
- disease control
- human health
- pastoralism
- zoonotic diseases
You may also like

Building resilience: Community-led response to Rift Valley fever in Isiolo County, Kenya

Unlocking the power of the genome: A leap towards enhanced food nutrition security and species conservation

Tony Barbet, ILRAD, University of Florida tickborne disease molecular biologist, dies

New science
A vaccine solution for african swine fever is within reach.

ILRI joins new EU-funded research consortium to develop African swine fever vaccine

ILRI champions One Health on World Neglected Tropical Diseases Day
The United States Department of Agriculture joins the global race to control contagious bovine pleuropneumonia
Related publications.

Current and potential use of animal disease data by stakeholders in the global south and north
- Grace, Delia
- Amenu, Kebede
- Daborn, C.J.
- Knight-Jones, Theodore J.D.
- Huntington, B.
- Poole, Elizabeth J.
- Rushton, J.

Cross-sectional serosurvey of Leptospira species among slaughter pigs, goats, and sheep in Uganda
- Alinaitwe, Lordrick
- Aturinda, C.J.
- Kivali, Velma
- Bugeza, James
- Wainaina, M.
- Richter, M.H.
- Hoona, J.J.
- Roesel, Kristina
- Mayer-Scholl, A.
- Cook, Elizabeth A.J.

Determinants of animal disease and nontherapeutic antibiotic use on smallholder livestock farms
- Kagambèga, A.
- Dione, Michel M.
African swine fever management planning: A practical approach
- Deka, Ram Pratim

Serological evidence and factors associated with Crimean–Congo haemorrhagic fever in sheep in Burkina Faso
- Dahourou, L.D.
- Savadogo, M.
- Yougbaré, B.
- Ouoba, L.B.
- Tapsoba, A.S.R.
- Zerbo, L.H.
- Ilboudo, Abdoul K.
- Alambédji, R.B.

Rationalising development of classification systems describing livestock production systems for disease burden analysis within the Global Burden of Animal Diseases programme
- McIntyre, K. Marie
- Rasmussen, Philip
- Gilbert, William
- Chaters, Gemma
- Raymond, Kassy
- Jemberu, Wudu T.
- Larkins, Andrew
- Patterson, Grace T.
- Kwok, Stephen
- Kappes, Alexander James
- Mayberry Dianne
- Schrobback, Peggy
- Herrero Acosta, Mario
- Stacey, Deborah A.
- Huntington, Benjamin
- Bruce, Mieghan
- Rushton, Jonathan
Related Projects

ACTIVE Dec 2027
New technologies for african swine fever (vax4asf).

ACTIVE Dec 2024
Analysis of the cross-protective response induced by african swine fever virus recombinant vaccine asfv-g-δi177l.

Adoption and scaling up of improved livestock production systems in Zimbabwe (LIPS-Zim)
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- J Urban Health
- v.93(4); 2016 Aug

Urban Health Research in Africa: Themes and Priority Research Questions
1 Division of Public Health Medicine, School of Public Health and Family Medicine, University of Cape Town, Cape Town, South Africa
Warren Smit
2 African Centre for Cities, University of Cape Town, Cape Town, South Africa
Richard Matzopoulos
3 Burden of Disease Research Unit, South African Medical Research Council, Cape Town, South Africa
Jo Hunter Adams
4 Health Economics unit, School of Public Health and Family Medicine, University of Cape Town, Cape Town, South Africa
Michelle Pentecost
5 Department of Anthropology, University of Cape Town, Cape Town, South Africa
6 Institute of Social and Cultural Anthropology, University of Oxford, Oxford, UK
Hanna-Andrea Rother
7 Division of Environmental Health and Centre for Environmental and Occupational Health Research, School of Public Health and Family Medicine, University of Cape Town, Cape Town, South Africa
Zulfah Albertyn
8 Children’s Institute, Department of Paediatrics, University of Cape Town, Cape Town, South Africa
Farzaneh Behroozi
9 Primary Health Care Directorate, University of Cape Town, Cape Town, South Africa
Olufunke Alaba
Mamadou kaba.
10 Division of Health Economics, School of Public Health and Family Medicine, University of Cape Town, Cape Town, South Africa
11 Division of Medical Microbiology, Department of Clinical Laboratory Sciences, University of Cape Town, Cape Town, South Africa
Claire van der Westhuizen
12 Alan J Flisher Centre for Public Mental Health, Department of Psychiatry and Mental Health, University of Cape Town, Cape Town, South Africa
Maylene Shung King
13 Division of Health Policy and Systems, School of Public Health and Family Medicine, University of Cape Town, Cape Town, South Africa
Naomi S. Levitt
14 Chronic Disease Initiative for Africa and Division of Diabetic Medicine and Endocrinology, Department of Medicine, University of Cape Town, Cape Town, South Africa
Susan Parnell
Estelle v. lambert.
15 Division of Exercise Science and Sports Medicine, Department of Human Biology, University of Cape Town, Cape Town, South Africa
Introduction
In Africa, urbanization and urban growth are dramatically restructuring the nature of cities. The growing majority of urban dwellers now live in informal conditions that, without access to basic services or public amenities, expose residents to greater health risk, and health-care systems are unable to provide affordable or comprehensive cover. The differential exposure to these urban conditions is compounded by social and economic vulnerability, resulting in health inequities. Yet despite pressing needs driven by Africa’s considerable and complex burden of disease and high levels of health inequity, urban health and urban health equity have not yet emerged as major research and policy priorities in Africa, and as such South Africa, like many other African countries, lags behind in addressing these issues.
This commentary presents a conceptual framework, using a public health approach, for interdisciplinary research aimed at contributing to the understanding and mitigation of urban health issues and challenges in Africa (Fig. 1 ). This approach identifies downstream and upstream factors, based on published literature, associated with key determinants in each theme. In other words, in addition to the individual level risk factors, the figure summarizes factors associated with each theme at the community, experiential, environmental, and structural policy levels. It represents a collective effort by interdisciplinary academics from public health; anthropology; civil engineering; architecture, planning and geomatics; human biology; psychiatry and mental health; medicine; pathology; and paediatrics, from the Research Initiative for Cities and Health ( RICHE ), University of Cape Town (UCT), to generate African perspectives on urban health and urban health equity. A workshop to tackle the urban health research agenda in August 2015 was attended by 40 RICHE members with extensive global and local urban health experience. In line with the co-production philosophy advocated for African urban contexts 1 , additional contributions came from representatives from the Western Cape Department of Health. The process of identifying themes and gaps was as follows: First existing urban health research in Africa was presented. The workshop participants, who have a wide range of experience in urban health in Africa presented what work was ongoing or planned. Through this iterative process, the key components of research questions identified were then thematically classified into six distinct focus areas. Using a public health, socio-ecological model, these themes were then classified into different levels from the individual to policy levels. Gaps in research were then identified qualitatively by the same iterative process from which unanswered priority research questions were identified. Three cross-cutting principles for African urban health research were also identified in the process, based on methodological and technical requirements for the successful conduct of the proposed research themes (Table (Table1 1 ).

Conceptual framework of public health approach to urban health research themes in Africa.
Urban health research focus areas and priority research questions
Six Focus Area Themes
Urban context as a tool for health promotion and disease prevention.
The health and well-being of urban residents is intricately linked to the natural, built, and institutional elements of the urban context. As such, all dimensions of urbanization and urban living, including socio-environmental determinants of health need to be considered 2 . The Commission on the Social Determinants of Health 3 and the Hidden Cities 4 reports identify addressing urban health as a key priority in the global South. Thus, investigation of the interaction between health and the urban determinants of health (social and policy environments, health services, the built, physical housing and recreational environments, food systems, crime/security, access to potable water, air quality, transport, vector and pest management, community resilience, psycho-social support structures) is essential 5 . Understanding these interactions could facilitate developing, implementing, and evaluating interventions that aim to harness these aspects of the urban context as tools for health promotion and prevention of infectious and vector-borne diseases, non-communicable diseases, and injuries, which in South African cities account for 20 % more mortality than in rural areas 6 . This understanding could be gained via research paired with “natural experiments” and randomized evaluations, such as urban upgrades, housing developments, and integrated transport system routes, to assess the impact on health behaviors and health outcomes.
Obesity and Food Insecurity Nexus
As in South Africa, the most urbanized African country, many low- and middle-income countries, urban populations on average have better access to health services and are associated with better health indicators overall 7 , 8 . However, urban areas are characterized by significant spatial and environmental deprivation and discrimination, the co-existence of chronic communicable and non-communicable diseases along with a high prevalence of obesity in predominantly food insecure communities 9 , 10 . As urbanization has a direct effect on food systems and therefore nutrition, knowledge of local urban food systems and food ways, including the informal and formal sectors, is needed to address the dual burden of obesity and food security. In particular, given the higher prevalence of obesity in women in many African countries, the importance of pre-conception and peri-partum nutrition on fetal health and the subsequent health of the child into adulthood, research in this area should utilize a life-course approach to more effectively target nutritional interventions for health promotion and disease prevention.
Urban Health Governance and Policy
There is a growing recognition of the importance of social determinants of health and the need for a multisectoral effort to effectively address these determinants to improve health equity. Yet a coherent strategy has not been implemented in many African countries, resulting in a lack of understanding of the processes in place in different sectors, an absence of a shared learning space, and a paucity of data on the health impact of intersectoral policies and programs. While a number of government departments in South Africa have begun to include health objectives in their strategic and developmental planning 11 , the process and impact of this change has not been evaluated. This evaluation and an investigation into the barriers and facilitators to such policy reform are urgently needed. One approach that may guide research in this area is the Health in All Policies (HiAP) approach. This approach recognizes the important roles that structural, environmental, and socio-economic factors play in population health and highlights the need for intersectoral approaches to foster healthy communities and environments. Incorporating the context of informal housing into urban health governance research is required as housing policies of some African countries focus on upgrading, not eliminating, informal settlements. Key elements of this approach 12 include stakeholder (community, private sector, funders, policy makers) engagement, creation of co-benefits for multiple partners and efficiencies across agencies and sectors, and the creation of structural and procedural change to institutionalize HiAP within government processes and initiatives. These elements will support deep and sustainable intersectoral collaboration and promote health and equity in all government policies and programs.
Community Strengthening for Healthy Inclusive Cities
A healthy city has been defined as one that is “continually creating and improving those physical and social environments and strengthening those community resources which enable people to mutually support each other in performing all the functions of life and achieving their maximum potential” 13 . In a major step forward, the new global sustainable development goals recognize the need to make cities inclusive, safe, resilient, and sustainable 14 . This goal is especially pertinent for vulnerable population groups (impoverished, low educational attainment, elderly, disabled, young) who are least equipped to compensate for the conditions that epidemiological, nutritional, climate, and urban transitions generate 15 , 16 . This “inverse care law” 17 results in social patterning, not only for access to health care but also “deprivation amplification” with a differential uptake and appropriation of messages promoting health. There is, therefore, a need to understand community well-being and how it affects individual health and to explore resources and positive attributes within communities, as well as health system competencies that can be strengthened and harnessed to improve urban community well-being and inclusivity.
Health Systems in an Urbanizing Context
Health systems are complex and require consideration of multiple components, factors, actors, and the interrelationships between these in order to adequately address health needs. In the context of urbanization and epidemiological transition in Africa 18 , a deeper understanding of how health systems may need to transform in order to muster an appropriate and sustainable response is required. In particular, account must be taken of the co-existence of chronic infectious disease (ID) epidemics such as HIV, emerging chronic non-communicable disease (NCD) epidemics, including mental disorders, and an increasing burden of violence and injuries 19 , 20 . While the South African health system is moving towards a decentralized, integrated approach to primary healthcare, many gaps in implementation exist 21 . Furthermore there is a lack of understanding of the needs of dynamic communities and very little community involvement in health-care organization and access planning 22 , 23 . The formal health systems also need to take into consideration the informality that characterizes many African urban settings in order to evaluate how best to reach those most in need. There is therefore a need for context-specific, integrated systems research to enable the health system to be responsive to population health transitions. In addition, it is important to recognise that the health system is part of a broader social system, and the interrelationship between the health and other social systems in mitigating the health needs is of paramount importance.
Migration, Urbanization, and Health: the Pathways and Mechanisms through Which Exposures to the Urbanizing Environment Influences Health, Health Risk, and Health Outcomes
Relatively high levels of impermanence and mobility characterize the urban population in many African countries 24 , particularly in informal areas where circular rural-urban and urban-urban movement is common. However, there is little quantification and appreciation of the nature of these population dynamics over space and time. Consequently, given the often-stark differences in environmental exposures, including pathogens, air, chemicals, and food, between rural and urban communities, a better understanding of urban population dynamics would facilitate investigation of the mechanisms through which these environmental exposures over the life course influence the biopsychosocial health of urban residents. For healthy migration, there is a need to better understand patterns of circular migration and differential health exposures in each stage of migration, as well as the ways in which health, economic, and social policies and systems best respond to mobility.
Three Cross-Cutting Principles
Cross-cutting principles necessary for these issues to be addressed underpin these themes.
Integration of Urban Intelligence and Surveillance
Upstream determinants of health (including social protection, employment (formal and informal), education, forensic pathology) need to be monitored by integrating routine datasets across sectors and a coordinated analysis of intersectoral data to inform research and policy priorities and interventions. In South Africa, there are three rural but no urban health and demographic surveillance sites. Indeed, there are currently only two urban surveillance sites in Africa (Nairobi, Kenya and Ouagadougou, Burkina Faso). Integration and coordination of urban intelligence through a surveillance system would contribute vital information that supports the conduct of implementation research and the assessment of natural experiments, to address key societal challenges in South Africa and the African continent. The extent and nature of the urban health indicators surveyed should be based on known health equity gaps and in particular, those that are mutable and that will be responsive to policy and program solutions 25 .
Systems Approach to Monitoring, Impact, and Policy Evaluation
The support, tracking, and evaluation of diverse health and health-related policy and system changes should use a variety of analytical frameworks and approaches, including economic analyses. Context is the key, as current conditions are created by politics and systemic inequalities in society. 26
Communication, Dissemination, and Meaningful Translation
For research to improve health disparities for the urban poor, there is a need to promote engaged scholarship and an engaged society with key stakeholder (governmental departments and communities) collaboration to identify research priorities and programs. Innovative knowledge creation, dissemination in public media, and meaningful engagement with broader society are also required to promote health and well-being through embracing principles of citizen science and the adoption of an inclusive, all-of-society, approach.
Priority Research Questions
Guided by these themes, an urban health research gap analysis was conducted, identifying key gaps in research. Based on these research gaps, we proposed urban health research questions that should be prioritized in Africa (Table (Table1 1 ).
The themes and cross-cutting principles presented overlap and interact with each other. As such, a complex systems approach is required to investigate and improve understanding of health and well-being in a changing urban context with a view to developing sustainable and cost-effective interventions. This approach:
- Acknowledges the different dimensions of determinants that influence health;
- Understands the importance of addressing gaps in data and access to information from across these dimensions;
- Identifies the need to address inequity in health and health determinants;
- Recognizes the need to contextualize the dimensions of the urban environment and engage all relevant stakeholders across sectors to effectively prioritize intersectoral interventions to improve health; and
- Emphasizes that action to address health determinants should not be solely undertaken by the health sector but requires an interdisciplinary approach and the involvement of key sectors including economic and social development, housing, and planning.
RICHE researchers are optimistic that the funding environment will support the need for a public health approach to urban health research themes addressing the African context so as to reduce urban health disparities and promote evidence-based policy making.
Acknowledgments
T.O. received a WHO TDR training grant (ID number: 184732).
Needs and opportunities for addressing the nexus of climate change and public health in Africa
Subscribe to africa in focus, tedros adhanom-ghebreyesus ta tedros adhanom-ghebreyesus director general - world health organization @drtedros.
May 9, 2024
This viewpoint is part of Foresight Africa 2024 .
Climate change is having increasingly disastrous effects on human health and well-being, especially in Africa, and protecting and promoting health is a powerful argument for climate action. Ultimately, the climate crisis is a health crisis.
More than half of the public health events reported in Africa during the first two decades of the 21st century are identified as climate-related health emergencies, according to a recent analysis by the WHO. This already worrying trend is accelerating. There were 25% more climate-related events recorded between 2011 and 2021 when compared with the previous decade. 1
The population of Africa is projected to almost double to 2.5 billion by 2050, and along with increasing urbanization, that will mean more people living in areas exposed to hazards such as extreme heat waves and floods. Unless adaptation measures are implemented, the toll of deaths, injuries, and illness due to climate disasters will continue to increase rapidly.
Under the umbrella of the historic 2008 Libreville Declaration on health and environment , the WHO supports countries to cope with the impacts of climate and environmental change on health systems, while networks such as Clim-Health Africa support multisectoral work and capacity building for climate-related health emergencies in Africa.
Following COP26 in Glasgow in 2021, with support from the U.K., Egypt, and the United Arab Emirates, the WHO launched the Alliance for Transformative Action on Climate and Health (ATACH). So far, 75 countries have committed to ATACH, 29 of them from Africa —allowing them to learn quickly from each other and from partners and to accelerate assessments, planning, and implementation to build climate-resilient and sustainable low-carbon health systems.
In many respects, African countries are ahead of the curve in climate adaptation. For example, the WHO is supporting Mozambique to connect climate information to health surveillance and planning to guide a faster and more effective early warning and response system to health risks from cyclones to malaria transmission. We are also working with Somalia to power essential health equipment in rural health clinics with cheap, clean, and reliable electricity from solar panels—leapfrogging the need for connection to an electrical grid. These interventions save lives now, provide resilience from climate change, and offer a vision of a greener and healthier continent.
The WHO welcomes the leadership of the United Arab Emirates in dedicating an entire day of COP28 to health. This is a critical opportunity for driving system transformation, strengthening support on adaptation and resilience, and financing climate and health, specifically for the African continent, which is one of the most-affected regions while a minimal contributor of greenhouse gas emissions.
To promote the human right to health and a healthy environment, the global health community is calling for health to be explicitly integrated into United Nations Framework Convention on Climate Change negotiation texts and outcomes. Climate change is having increasingly disastrous effects on human health and well-being, especially in Africa, and protecting and promoting health is a powerful argument for climate action. Ultimately, the climate crisis is a health crisis.
Related Content
Ede Ijjasz-Vasquez, Jamal Saghir, Morgan Richmond
February 22, 2024
Kerllen Costa
March 28, 2024
Angela R. Pashayan
February 29, 2024
- WHO Africa. 2022. “Africa faces rising climate-linked health emergencies.”
Climate Action & Justice Climate Adaptation & Resilience Climate Change
Global Economy and Development
Africa Growth Initiative
Nasrin Siddiqa, Atenea Rosado-Viurques
April 23, 2024
Homi Kharas, Charlotte Rivard
April 16, 2024
Pedro Conceição
April 3, 2024

National Public Health Institutes and Research

Strengthened public health science and improved public health decision-making and practice to achieve positive health outcomes.
Strategic Objectives
- Establish Africa CDC public health research agenda with goals and objectives that address priority health issues, which may include certain suitable capacities.
- Strengthen public health research capacity within public institutions, in partnership with academic institutions in Member States.
- Promote collaboration and coordination among existing networks for conducting research on priority public health research issues.
- Re-characterize the known burden of “disease” and other health concerns from a continental and/or regional perspective (core epi, clinical descriptive).
- Assess the effectiveness of existing public health interventions on health conditions that have been prioritized by the health policy instruments of the African Union.
- Support research on surveillance methodologies: quality interventions and innovative technologies.
- Apply multi-sectoral/cross-cutting One Health strategies to the Africa CDC public health research agenda.

Revolutionizing Public Health in Africa: Launch of the African Public Health Institutes Collaborative (APHIC)

Africa CDC – UNICEF Consultation Workshop to Support Country Plan Development

Africa speaks with one voice on the Pandemic Agreement

Statement by H.E Dr. Jean Kaseya, Director General of Africa CDC, on the African Vaccination Week
Communiqué from the african high–level ministerial consultation for intergovernmental negotiating body on the draft pandemic prevention, preparedness and response agreement.

Africa CDC and EU partner in new genomic surveillance and data-sharing projects

African researchers propose Mpox research group

Africa CDC launches initiatives to advance molecular diagnostics and genomic surveillance in Africa

Création d’un centre régional de connaissances en Afrique centrale : la plateforme présentée aux experts de la région
Subscribe for alerts.
Numbers, Facts and Trends Shaping Your World
Read our research on:
Full Topic List
Regions & Countries
- Publications
- Our Methods
- Short Reads
- Tools & Resources
Read Our Research On:
Public Health a Major Priority in African Nations
Improving hospitals, dealing with hiv/aids are top issues, survey report.
Concerns about public health are widespread in sub-Saharan Africa, and there is considerable support in the region for making public health challenges a top national priority. In particular, people want their governments to improve the quality of hospitals and other health care facilities and deal with the problem of HIV/AIDS.
A Pew Research Center survey, conducted March 6, 2013 to April 12, 2013 in six African nations, also finds broad support for government efforts to address access to drinking water, access to prenatal care, hunger, infectious diseases, and child immunization.
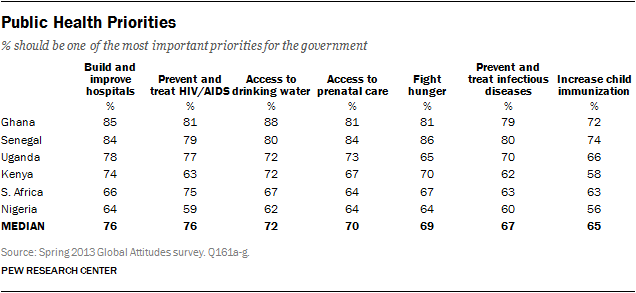
A median of 76% across six countries surveyed say building and improving hospitals and other health care facilities should be one of the most important priorities for their national government. The percentage of the public who holds this view ranges from 85% in Ghana to 64% in Nigeria.
Similarly, a median of 76% believe preventing and treating HIV/AIDS should be one of government’s most important priorities, ranging from 81% in Ghana to 59% in Nigeria.
A median of at least 65% also say the other issues included on the poll — ranging from access to drinking water to increased child immunization — should be among the most important priorities. In fact, majorities hold this view about all seven issues in all six nations.
Overall, there has been little change in public health priorities in Uganda or Kenya since these questions were last asked in 2007, although in the latter nation the percentage of people saying HIV/AIDS should be one of the most important priorities for government has declined from 80% to 63%. Meanwhile, Ghanaians today are more likely to say that six of the seven tested health issues should be a central concern for government. For instance, 85% of Ghanaians say this about building and improving hospitals, compared with 62% in 2007. 1

In a follow up question, respondents were asked which of these challenges they believe should be the most important public health priority for their government. On this question, responses are somewhat diffuse within each nation, and differ by country.
However, hospital and health care facility improvement is at or near the top of the list in several nations, including Uganda where roughly one-in-three (34%) consider this the number one public health concern.
Many also say HIV/AIDS should be the top priority for government, especially in South Africa and Uganda, which have the highest HIV prevalence rates among the six countries surveyed. 2 Meanwhile, fighting hunger and malnutrition is the highest priority in Senegal, and is tied for the top spot in Kenya.
- For more on the 2007 findings, see A Global Look At Public Perceptions of Health Problems, Priorities, and Donors: The Kaiser/Pew Global Health Survey . The 2007 survey was conducted in partnership with the Kaiser Family Foundation. Nigeria, Senegal and South Africa were also surveyed in 2007, but those trends are not shown because the 2007 samples in those countries were less representative than the 2013 samples, which are nationally representative. ↩
- 2012 estimates: 17.9% HIV prevalence rate in South Africa and 7.2% in Uganda. Data from AIDSinfo.org http://www.unaids.org/en/dataanalysis/datatools/aidsinfo/ ↩
Sign up for our weekly newsletter
Fresh data delivery Saturday mornings
Sign up for The Briefing
Weekly updates on the world of news & information
- Coronavirus (COVID-19)
- Health Policy
- Medicine & Health
How Americans View the Coronavirus, COVID-19 Vaccines Amid Declining Levels of Concern
Online religious services appeal to many americans, but going in person remains more popular, about a third of u.s. workers who can work from home now do so all the time, how the pandemic has affected attendance at u.s. religious services, mental health and the pandemic: what u.s. surveys have found, most popular, report materials.
- Spring 2013 Survey Data
1615 L St. NW, Suite 800 Washington, DC 20036 USA (+1) 202-419-4300 | Main (+1) 202-857-8562 | Fax (+1) 202-419-4372 | Media Inquiries
Research Topics
- Age & Generations
- Economy & Work
- Family & Relationships
- Gender & LGBTQ
- Immigration & Migration
- International Affairs
- Internet & Technology
- Methodological Research
- News Habits & Media
- Non-U.S. Governments
- Other Topics
- Politics & Policy
- Race & Ethnicity
- Email Newsletters
ABOUT PEW RESEARCH CENTER Pew Research Center is a nonpartisan fact tank that informs the public about the issues, attitudes and trends shaping the world. It conducts public opinion polling, demographic research, media content analysis and other empirical social science research. Pew Research Center does not take policy positions. It is a subsidiary of The Pew Charitable Trusts .
Copyright 2024 Pew Research Center
Bibliographic analysis of scientific research on selected topics in public health nutrition in West Africa: Review of articles published from 1998 to 2008
Affiliation.
- 1 Department of Nutrition, University of California Davis, USA.
- PMID: 21113830
- DOI: 10.1080/17441692.2010.526128
Few countries in West Africa have the capacity for carrying out advanced training in nutrition and public health. To provide additional information on current regional applied nutrition research capacity and productivity, we analysed peer-reviewed articles on key public health nutrition topics that were published from 1998 to 2008. Using MEDLINE/PubMed, the following terms were searched: 'breast feeding', 'infant nutrition physiology' (comprising complementary feeding and weaning), 'protein energy malnutrition', 'nutrition and infection', 'vitamin A', 'iodine', 'zinc' and 'overweight', each linked with the term 'Western Africa'. In total, 412 unique articles (37±6 articles per year) were identified. Most research focused on infant and young child feeding practices, selected micronutrient deficiencies, and the emerging problem of overweight and obesity. The primary author of nearly half (46%) the publications was located in an institution outside of West Africa. Most articles were published in English (90%), and nearly half of all articles (41%) were cross-sectional studies. Our findings indicate that few peer-reviewed research studies are being published on key public health topics in the West African region, considering the magnitude of nutrition problems in this region. New approaches are needed to encourage and support research capacity and output in West Africa.
Publication types
- Research Support, Non-U.S. Gov't
- Africa, Western / epidemiology
- Bibliometrics
- Malnutrition / epidemiology
- Nutrition Assessment
- Nutritional Sciences*
- Peer Review, Research
- Public Health*
- Research* / statistics & numerical data

- About UNAIDS
- Global AIDS Strategy 2021-2026
- United Nations declarations and goals
- UNAIDS governance
- UNAIDS Programme Coordinating Board
- Results and transparency portal
- UNAIDS Cosponsors
- UNAIDS ambassadors and global advocates
- UNAIDS leadership
- UNAIDS evaluation office
- UNAIDS ethics office
- UNAIDS transformation
- Community pandemic response
- Education Plus Initiative
- Global alliance to end AIDS in children
- Equal access to cutting edge HIV technologies
- Save lives: Decriminalize
- Global council on inequality, AIDS and pandemics
- Resources and financing
- War in Ukraine
- Global HIV Prevention Coalition
- Global Partnership to Eliminate Stigma and Discrimination
- COVID-19 and HIV
- 2025 AIDS targets
- AIDS and SDGs
- Community mobilization
- Fast-Track cities
- H6 partnership
- HIV prevention
- HIV treatment
- Human rights
- Key populations
- Private sector and the AIDS response
- Security and humanitarian affairs
- Social protection
- Universal health coverage
- Young people
Press centre
- Publications
- Infographics
- FAQ on HIV and AIDS
- World AIDS Day
- Zero Discrimination Day
- Latest data on HIV
- Data on key populations
- Laws and policies
- HIV financial resources
- Technical Support Mechanism
- Learn about HIV and AIDS
- Take action
- Become a donor
- Investment Book
Press Statement

Press statement
Unaids calls for the protection of human rights on the international day to end homophobia, biphobia, and transphobia (idahobit).
GENEVA, 15 May 2024— Ahead of IDAHOBIT, commemorated worldwide on 17 May, UNAIDS is calling on governments everywhere to protect the human rights of LGBTQ+ people. Protecting the human rights of every person, UNAIDS research shows, is essential for protecting public health, because it enables inclusive and equitable access to health services without discrimination.
The movement for human rights for all has made important progress. For example, whereas, at the start of the AIDS pandemic, most countries criminalized LGBTQ+ people , now two thirds of countries do not.
However, more than 60 countries still do while another 20 countries criminalize gender expression and identity.
“Stigma, discrimination and criminalization can be lethal,” said Winnie Byanyima, Executive Director of UNAIDS. “In the response to HIV, we have learned that a human rights-based approach is critical in responding to a health crisis and leaving no-one behind. Countries must remove these discriminatory criminal laws and introduce legislation which protects rights if we are to end AIDS as a public health threat for everyone.”
Discrimination, violence and criminalization force many LGBTQ+ people underground and away from health services; as a result, gay men and other men who have sex with men, and transgender people, are more affected by HIV. Globally, in 2022, men who have sex with men were 23 times more likely to acquire HIV, and transgender women 20 times more likely to acquire HIV than other adults aged 15–49.
Criminalization of LGBTQ+ people in particular causes significant harm to health. In sub-Saharan Africa, men who have sex with men in countries where they are criminalized, are five times more likely to be living with HIV than in countries that do not criminalize same-sex sexual behavior.
As a recent IAS - Lancet report demonstrated, violations of human rights have multiple damaging impacts on public health. Treating people as criminals drives people away from vital services for fear of arrest and discrimination, resulting in them not accessing HIV prevention, treatment and care. In addition, strict anti-LGBTQ+ laws have been associated with a lack of knowledge about HIV testing and HIV status.
“For far too many people in our LGBTQ+ communities and beyond, the most basic things are still too far from reach, because of the discrimination, stigma, and violence they face every day,” said the international lesbian, gay, bisexual, trans and intersex association, ILGA World , co-Secretaries General Luz Elena Aranda and Tuisina Ymania Brown. “This is why they are rallying behind an urgent cry: ‘No one left behind: equality, freedom and justice for all,’ reminding us of the importance of rejecting discriminatory laws, policies, and attitudes.”
Criminal laws that discriminate on the basis of sexual orientation and gender identity are a breach of the right to privacy and non-discrimination and impede the HIV response. UNAIDS calls on all states to repeal such laws and to introduce legal protections against discrimination on the basis of sexual orientation.
UNAIDS, the World Health Organization, the United Nations Development Programme, and the Global Commission on HIV and the Law have made the same recommendations, as have the Office of the United Nations High Commissioner for Human Rights and several other United Nations agencies.
UNAIDS stands with LGBTQ+ people everywhere who are facing hate, discrimination and marginalization, and calls for an end to their criminalization.
The Joint United Nations Programme on HIV/AIDS (UNAIDS) leads and inspires the world to achieve its shared vision of zero new HIV infections, zero discrimination and zero AIDS-related deaths. UNAIDS unites the efforts of 11 UN organizations—UNHCR, UNICEF, WFP, UNDP, UNFPA, UNODC, UN Women, ILO, UNESCO, WHO and the World Bank—and works closely with global and national partners towards ending the AIDS epidemic by 2030 as part of the Sustainable Development Goals. Learn more at unaids.org and connect with us on Facebook , Twitter , Instagram and YouTube .
A .gov website belongs to an official government organization in the United States.
A lock ( ) or https:// means you've safely connected to the .gov website. Share sensitive information only on official, secure websites.
- When to Seek Medical Care for Rabies
- Suspected Human Rabies
About Rabies
- Rabies is a viral disease that is deadly in people if medical care is not received before symptoms start.
- Rabies is spread to humans and pets primarily through bites or scratches from an infected animal.
- Rabies control measures in the United States have significantly reduced rabies as a public health threat.
- Each year 60,000 Americans receive medical care following a potential rabies exposure.

What you need to know
Rabies is a fatal but preventable viral disease. It can be spread to people and pets through the bites and scratches of an infected animal. Rabies primarily affects the central nervous system, leading to severe brain disease and death if medical care is not received before symptoms start.
Immediate medical attention following suspected rabies exposure is critical. Medical care following a rabies exposure is called post-exposure prophylaxis or PEP. PEP includes wound care, a dose of human rabies immune globulin (HRIG), and a series of four or five rabies vaccines, which must be administered as soon as possible after exposure. This care is vital to prevent the disease from developing. It is nearly 100% effective if administered promptly. Each year, 60,000 Americans receive PEP after a potential rabies exposure.
The disease is rare in humans in the United States, with only 1 to 3 cases reported each year. Still, rabies poses a serious public health threat, because of its high death rate in people. It is also present in many wildlife species, nearly 3 in 4 Americans live in a community where raccoons, skunks, or foxes carry rabies.
Animals and rabies
In the United States, more than 90% of reported cases of rabies in animals occur in wildlife. Contact with infected bats is the leading cause of human rabies deaths in this country; at least 7 out of 10 Americans who die from rabies in the US were infected by bats. The animals most often found with rabies in the U.S. include:
While rabid dogs in the US are uncommon, around the world, domestic dogs are responsible for more than 95% of the estimated 70,000 human deaths that occur each year.
People at risk
People who are at increased risk for rabies exposures may want to consider pre-exposure vaccination for increased protection.
People who travel
Since 1990, over 80 people have died from rabies after an exposure during travel. Rabies is prevalent globally except in Antarctica. In Africa, Asia, and specific areas of Central and South America, rabies in dogs is still a major problem. Additionally, access to PEP may be hard to get in those places. As a result, tens of thousands of people die of the disease each year.
When traveling, it is important to keep your distance from wild and unfamiliar animals, including dogs and cats.
Before traveling abroad, consult your doctor, a travel clinic , or your local or state health department about your risk of exposure to rabies.
People who participate in certain leisure activities
People who enjoy outdoor certain outdoor activities that may lead to contact with wildlife, such as spelunking, camping, and hunting are at higher risk of being exposed to rabies, because they may encounter wildlife while participating in these activities.
People who have jobs with animals
People with jobs that involve frequent animal contact, such as veterinary professionals (including technicians), animal control workers, wildlife researchers, wildlife rehabilitation workers, and certain agricultural workers, are at increased risk of a rabies exposure. People who work with or are exposed to wild animals could encounter a wild animal with rabies. People who work with pets may be exposed if a pet is not vaccinated for rabies and/or has encountered a wild animal with rabies.
Rabies prevention efforts by veterinary, wildlife management, and public health professionals mean that human cases of rabies in the U.S. are rare. Veterinarians vaccinate over 40 million cats and dogs each year, and these vaccinations significantly reduce the risk of you or your pets getting rabies. Each year, wildlife management professionals distribute oral vaccines to wildlife, through baits, to control rabies at its source, especially in areas where rabies in wild animals is common.
The best way you can prevent rabies is by:
- Making sure your pets are up-to-date on their rabies vaccines;
- Keeping wildlife wild - stay away from wildlife for both human and animal safety;
- Calling animal control to remove stray animals from your neighborhood;
- Washing bites or scratches immediately with soap and water; and
- Seeking medical care shortly after potential exposures.
Around the world, large-scale dog vaccination programs are the most effective way to prevent rabies. However, in many countries, there aren't enough resources to reach all the dogs that need it. CDC works with public and private partners to improve vaccine access for people and animals, making travel safer and improving global health.
- International Rabies Taskforce
Rabies is a preventable viral disease of mammals usually transmitted through the bite of an infected animal.
For Everyone
Health care providers.

IMAGES
VIDEO
COMMENTS
The Journal of Public Health in Africa (JPHiA) is a peer-reviewed, academic journal that focuses on health issues in the African continent. The journal editors seek high quality original articles on public health related issues, reviews, comments and more. The aim of the journal is to move public health discourse from the background to the forefront.
Quarraisha Abdool Karim. Notable for: Developing HIV prevention solutions for women. Led South Africa's first community-based HIV prevalence study in 1990, discovering disproportionately high rates of infection among adolescent girls. Helped establish and is associate scientific director of the Centre for the AIDS Programme of Research in ...
ISSN: 3006-4090 EISSN: 3006-4104. Health Research in Afr ica (HRA) is an open access, peer reviewed medical journal that is affiliated to Health Sciences and Disease. HRA values high quality research with impact on clinical care in order to improve human health in Africa. HRA covers all aspects of medicine, pharmacy, biomedical and health ...
Since 2000, Africa has made historic progress in improving health metrics across all age groups 4. The WHO estimates that the region successfully reduced the number of malaria-, HIV-1-, and ...
We aim to promote high-quality research that advances our understanding of health issues in Africa, and advocates for better healthcare on the continent in line with the United Nations 2030 Agenda ...
research in Africa" conducted by LSE investigated barriers and facilitators to improving health sciences research (HSR) in a set of African countries across all sub-regions (with HSR taken to include a range of activities from basic and clinical science to public health research or applied health policy and systems research) (Jones et al ...
I am convinced that a new way of doing public health in Africa is within reach. Nature 621, 9 (2023 ... Consider joining the Center for Cancer Research (CCR) at the National Cancer Institute. ...
The Journal of Public Health in Africa is a peer-reviewed, academic journal that focuses on health issues in the African continent. The journal editors seek high quality original articles on public health-related issues, reviews, comments and more. ... We will continue to provide a platform for groundbreaking research and foster an environment ...
The continent of Africa is home to 17% of the global population that carries 25% of the global disease burden. Yet globally, it accounts for less than 2% of genomic data1 used in medical innovation and less than 3% of clinical trials.2 Clinical research remains concentrated in high-income countries.3 Here, we highlight the importance of diversity in clinical research and propose solutions to ...
Africa's New Approach to Public Health. Published November 29, 2022. COVID-19. Health Policy. ... Research Gaps Around Type 1 Diabetes. April 19, 2024 ... A South African Soup Kitchen Is Bringing Relief to Caregivers . April 18, 2024. Johns Hopkins Bloomberg School of Public Health 615 N. Wolfe Street, Baltimore, MD 21205. Footer social ...
Health sciences research (HSciR) has been defined to include basic, clinical and applied science on human health and well-being, as well as the determinants, prevention, detection, treatment and management of disease [1,2,3].To date, the majority of HSciR has taken place in the Global North [4,5,6].As of 2018, less than 1% of scientific articles published worldwide each year include at least ...
The recent Ebola outbreak in West Africa has foregrounded questions about how to strengthen public health systems and drawn attention to notions of 'resilience', and the relationship between health system resilience and relations of trust between citizens and the state (Bloom, MacGregor, Mackenzie, & Sokpo, 2015; Wilkinson & Leach, 2014 ).
The journal found out, for example, that from 1991 to 2010, epidemiologic research as a part of public health research in the WHO/AFRO region increased from 172 to 1086. At first glance, the increased number seems impressive but it amounts to only 50 articles per year for the whole continent during a period of 19 years.
Three global health partners launched a pioneering peer-to-peer learning initiative, the African Public Health Institutes Collaborative (APHIC), at an inaugural meeting in Addis Ababa this week, highlighting the importance of strengthening collaborations across core public health functions to have greater impact by working together. The new initiative is a collaboration between the Africa ...
The goal of this Research Topic is to receive and catalogue original research manuscripts and reviews that assesses the relationship between environmental and nutritional exposures of pressing concern in Africa, and the health outcomes increasing in prevalence on the continent. ... Topics may include, but are by no means limited to public ...
Emerging public health threats in Africa's drylands. Active. FromMarch 2023 toFebruary 2028. Goal. The goal of the project is to mitigate threats of vector-borne diseases in Mandera, Marsabit, Samburu and Turkana counties of northern Kenya. Overview. Pastoralism is an important livelihood activity in the arid lands of northern Kenya.
In Africa, urbanization and urban growth are dramatically restructuring the nature of cities. The growing majority of urban dwellers now live in informal conditions that, without access to basic services or public amenities, expose residents to greater health risk, and health-care systems are unable to provide affordable or comprehensive cover.
More than half of the public health events reported in Africa during the first two decades of the 21st century are identified as climate-related health emergencies, according to a recent analysis ...
Goal Strengthened public health science and improved public health decision-making and practice to achieve positive health outcomes. Strategic Objectives Establish Africa CDC public health research agenda with goals and objectives that address priority health issues, which may include certain suitable capacities. Strengthen public health research capacity within public institutions, in ...
Lead Stories: WHO Prequalifies Second Dengue Vaccine, Expanding Global Access. May 17, 2024: The World Health Organization WHO has prequalified Takeda Pharmaceuticals' TAK-003 making it the second dengue vaccine to receive this recognition Learn more [Read more] South Africa's National Health Insurance at a Glance. May 17, 2024:
By Topic. Faculty, students, researchers and visiting scholars at UC Berkeley engage in a wide range of research on Africa. Politics, public health, conflict, human rights, environment, conservation, climate change, technology, religion and languages are just some of the areas covered. Over time, we will add various ways to explore the research ...
A Pew Research Center survey, conducted March 6, 2013 to April 12, 2013 in six African nations, also finds broad support for government efforts to address access to drinking water, access to prenatal care, hunger, infectious diseases, and child immunization. A median of 76% across six countries surveyed say building and improving hospitals and ...
Few countries in West Africa have the capacity for carrying out advanced training in nutrition and public health. To provide additional information on current regional applied nutrition research capacity and productivity, we analysed peer-reviewed articles on key public health nutrition topics that were published from 1998 to 2008.
Discrete choice experiments in medical education : the role of management, health economics and research. Turner, Astrid Chrisilda (University of Pretoria, 2023-12-15) In this thesis, Discrete choice experiments in medical education: the role of management, health economics and research, the candidate utilised the stated preference technique ...
GENEVA, 15 May 2024—Ahead of IDAHOBIT, commemorated worldwide on 17 May, UNAIDS is calling on governments everywhere to protect the human rights of LGBTQ+ people.Protecting the human rights of every person, UNAIDS research shows, is essential for protecting public health, because it enables inclusive and equitable access to health services without discrimination.
The disease is rare in humans in the United States, with only 1 to 3 cases reported each year. Still, rabies poses a serious public health threat, because of its high death rate in people. It is also present in many wildlife species, nearly 3 in 4 Americans live in a community where raccoons, skunks, or foxes carry rabies. Animals and rabies
By Liam Connolly. (SACRAMENTO) Two UC Davis Health physicians from the Department of Emergency Medicine received national awards for their contributions to the field from the Society for Academic Emergency Medicine (SAEM). Nathan Kuppermann, the Bo Tomas Brofeldt endowed chair of emergency medicine, was the recipient of the John Marx Leadership ...