
100+ ICMR Research Topics: Unlocking Health Insights
The landscape of healthcare research in India has been significantly shaped by the endeavors of the Indian Council of Medical Research (ICMR). Established in 1911, the ICMR has played a pivotal role in advancing medical knowledge, informing health policies, and fostering collaborations to address pressing health challenges in the country.
In this blog, we embark on a journey through the corridors of ICMR research topics, shedding light on the council’s current and noteworthy research topics that are contributing to the nation’s health and well-being.
The Role of ICMR in Health Research
Table of Contents
The Indian Council of Medical Research operates as the apex body in India for the formulation, coordination, and promotion of biomedical research. With a mission to nurture and harness the potential of medical research for the benefit of society, ICMR has become a cornerstone in shaping health policies and practices.
By fostering collaborations with researchers and institutions across the nation, ICMR has emerged as a driving force in advancing healthcare knowledge and outcomes.
Understanding ICMR Research Methodology
The success of ICMR’s research lies not only in its expansive scope but also in its rigorous methodology and ethical considerations. ICMR has established guidelines that researchers must adhere to, ensuring that studies funded by the council are not only scientifically sound but also ethically conducted.
This commitment to ethical research practices has been a cornerstone in building public trust and confidence in the findings generated by ICMR-funded studies.
100+ ICMR Research Topics For All Level Students
- Infectious Diseases: Emerging pathogens and control strategies.
- Non-Communicable Diseases (NCDs): Diabetes, cardiovascular research.
- Maternal and Child Health: Strategies for mortality reduction.
- Biomedical Research: Molecular insights into diseases.
- Cancer Research: Innovative approaches for treatment.
- Epidemiology: Studying disease patterns and trends.
- Vaccination Strategies: Enhancing immunization programs.
- Public Health Interventions: Effective community health measures.
- Antibiotic Resistance: Combating microbial resistance.
- Genetic Studies: Understanding genetic contributions to diseases.
- Neurological Disorders: Research on neurological conditions.
- Mental Health: Addressing mental health challenges.
- Nutrition and Health: Studying dietary impacts on health.
- Health Systems Research: Improving healthcare delivery.
- Ayurveda Research: Integrating traditional medicine practices.
- Environmental Health: Impact of environment on health.
- Emerging Technologies: Utilizing tech for healthcare innovations.
- Pharmacological Research: Advancements in drug discovery.
- Global Health Collaborations: International health partnerships.
- Waterborne Diseases: Prevention and control strategies.
- Health Policy Research: Shaping evidence-based policies.
- Health Economics: Studying economic aspects of healthcare.
- Telemedicine: Harnessing technology for remote healthcare.
- Rare Diseases: Understanding and treating rare disorders.
- Community Health: Promoting health at the grassroots level.
- HIV/AIDS Research: Advancements in HIV prevention and treatment.
- Aging and Health: Research on geriatric health issues.
- Cardiovascular Health: Preventive measures and treatments.
- Respiratory Diseases: Understanding lung-related conditions.
- Zoonotic Diseases: Investigating diseases transmitted from animals.
- Stem Cell Research: Applications in regenerative medicine.
- Yoga and Health: Studying the health benefits of yoga.
- Gender and Health: Research on gender-specific health issues.
- Oral Health: Preventive measures and treatments for oral diseases.
- Health Informatics: Utilizing data for healthcare improvements.
- Health Education: Promoting awareness for better health.
- Drug Resistance: Research on antimicrobial resistance.
- Hepatitis Research: Prevention and treatment strategies.
- Telehealth: Remote healthcare services and accessibility.
- Diabetes Management: Strategies for diabetes prevention and control.
- Tuberculosis Research: Advancements in TB diagnosis and treatment.
- Fertility Research: Understanding reproductive health issues.
- Artificial Intelligence in Healthcare: Integrating AI for diagnostics.
- Health Disparities: Addressing inequalities in healthcare access.
- Mental Health Stigma: Research on reducing stigma.
- Mobile Health (mHealth): Applications for mobile-based healthcare.
- Vector-Borne Diseases: Prevention and control measures.
- Nanotechnology in Medicine: Applications in healthcare.
- Occupational Health: Research on workplace health issues.
- Biobanking: Storing and utilizing biological samples for research.
- Telepsychiatry: Providing mental health services remotely.
- Health Equity: Promoting fairness in healthcare delivery.
- Community-Based Participatory Research: Engaging communities in research.
- E-health: Electronic methods for healthcare delivery.
- Sleep Disorders: Understanding and treating sleep-related conditions.
- Health Communication: Effective communication in healthcare.
- Global Burden of Disease: Research on disease prevalence and impact.
- Traditional Medicine: Studying traditional healing practices.
- Nutraceuticals: Research on health-promoting food components.
- Health Data Security: Ensuring privacy and security of health data.
- Regenerative Medicine: Advancements in tissue engineering.
- Social Determinants of Health: Studying social factors affecting health.
- Pharmacovigilance: Monitoring and ensuring drug safety.
- Gerontology: Research on aging and the elderly.
- Mobile Apps in Healthcare: Applications for health monitoring.
- Genetic Counseling: Supporting individuals with genetic conditions.
- Community Health Workers: Role in improving healthcare access.
- Health Behavior Change: Strategies for promoting healthier habits.
- Palliative Care Research: Enhancing end-of-life care.
- Nanomedicine: Applications of nanotechnology in medicine.
- Climate Change and Health: Impact on public health.
- Health Literacy: Promoting understanding of health information.
- Antibody Therapeutics: Advancements in antibody-based treatments.
- Digital Health Records: Electronic health record systems.
- Microbiome Research: Understanding the role of microorganisms in health.
- Disaster Preparedness: Research on health response during disasters.
- Food Safety and Health: Ensuring safe food consumption.
- Artificial Organs: Advancements in organ transplantation.
- Telepharmacy: Remote pharmaceutical services.
- Environmental Epidemiology: Studying the link between environment and health.
- E-mental Health: Digital tools for mental health support.
- Precision Medicine: Tailoring treatments based on individual characteristics.
- Health Impact Assessment: Evaluating the consequences of policies on health.
- Genome Editing: Applications in modifying genetic material.
- Mobile Clinics: Bringing healthcare to underserved areas.
- Telecardiology: Remote cardiac care services.
- Health Robotics: Utilizing robots in healthcare settings.
- Precision Agriculture and Health: Linking agriculture practices to health outcomes.
- Community-Based Rehabilitation: Supporting rehabilitation at the community level.
- Nanotoxicology: Studying the toxicological effects of nanomaterials.
- Community Mental Health: Strategies for promoting mental well-being.
- Health Financing: Research on funding models for healthcare.
- Augmented Reality in Healthcare: Applications in medical training and diagnostics.
- One Health Approach: Integrating human, animal, and environmental health.
- Disaster Mental Health: Addressing mental health issues after disasters.
- Mobile Laboratory Units: Rapid response in disease outbreaks.
- Health Impact Investing: Investing for positive health outcomes.
- Rehabilitation Robotics: Assisting in physical therapy.
- Human Microbiota: Understanding the microorganisms living in and on the human body.
- 3D Printing in Medicine: Applications in medical device manufacturing.
Success Stories from ICMR-Funded Research
Highlighting the impact of ICMR-funded research is essential in appreciating the council’s contribution to healthcare in India. From breakthrough discoveries to successful interventions, ICMR-supported studies have led to tangible improvements in health outcomes.
Case studies showcasing the journey from ICMR research topics and findings to real-world applications serve as inspiring examples of how scientific knowledge can translate into positive societal impacts.
Challenges and Opportunities in ICMR Research
While ICMR has achieved remarkable success in advancing health research, it is not without its challenges. Researchers face obstacles in conducting studies, ranging from resource constraints to logistical issues.
Acknowledging these challenges is crucial in finding solutions and optimizing the impact of ICMR-funded research. Additionally, there are opportunities for collaboration, both nationally and internationally, that can further enrich the research landscape and accelerate progress in addressing health challenges.
The Future of Health Research in India: ICMR’s Vision
Looking ahead, ICMR envisions a future where health research continues to play a central role in shaping the well-being of the nation. Strategic goals include harnessing the power of technology and innovation to drive research advancements, fostering interdisciplinary collaborations, and addressing emerging health challenges.
The vision extends beyond the laboratory, emphasizing the translation of research findings into practical solutions that can positively impact the lives of individuals and communities across India.
In conclusion, the Indian Council of Medical Research stands as a beacon in the realm of healthcare research, tirelessly working towards advancements that contribute to the well-being of the nation.
By exploring ICMR research topics, understanding its methodology, and reflecting on success stories, we gain insight into the transformative power of scientific inquiry.
As ICMR continues to forge ahead, the future of health research in India looks promising, guided by a vision of innovation, collaboration, and a steadfast commitment to improving the health of all citizens.
Related Posts

Step by Step Guide on The Best Way to Finance Car

The Best Way on How to Get Fund For Business to Grow it Efficiently
- Open access
- Published: 24 August 2021
Psychological well-being and burnout amongst medical students in India: a report from a nationally accessible survey
- Sharad Philip ORCID: orcid.org/0000-0001-8028-3378 1 ,
- Andrew Molodynski 2 , 3 ,
- Lauren Barklie 2 ,
- Dinesh Bhugra 4 &
- Santosh K. Chaturvedi 1
Middle East Current Psychiatry volume 28 , Article number: 54 ( 2021 ) Cite this article
5408 Accesses
9 Citations
Metrics details
Medical students in India face multiple challenges and sources of stress during their training. No nationally representative survey has yet been undertaken. We undertook a cross-sectional national survey to assess substance use, psychological well-being, and burnout using CAGE, Oldenburg Burnout Inventory (OLBI), and the short General Health Questionnaire (GHQ-12). The survey was open to all medical students in India. Descriptive statistics along with chi square tests and Spearman’s correlation were performed.
Burnout was reported by 86% of respondents for disengagement and 80% for exhaustion. Seventy percent had a score of more than 2 on the GHQ-12, indicating caseness.
Conclusions
This study reveals that medical students are going through exceptional stress when compared to their age-matched peers. More nationally representative studies must be conducted on a large scale to quantify the problem and to help design new interventions.
The rigours of medical education are well-known internationally, and medical students’ mental health morbidity is higher than that of their aged-matched peers [ 1 ]. Medical students are prone to anxiety, depressive disorders, and high levels of psychological distress [ 2 , 3 , 4 , 5 , 6 , 7 ]. Such issues may progress to negatively impact academic performance, predispose to substance use, and/or encourage other maladaptive coping strategies [ 4 , 8 , 9 ]. Increased distress can also increase academic dishonesty [ 10 ].
‘Burnout’ was first outlined by Freudenberger in 1974 [ 11 ], and ‘International Classification of Diseases-11 (ICD-11)’ recognises it as an occupational phenomenon in all workplace environments. Initially described as including reduced personal accomplishment, depersonalization, and emotional exhaustion, it is considered to be a health issue arising in the context of poorly managed workplace stress. It is comprised of three dimensions—energy depletion, reduced professional efficacy, and feelings of negativism or cynicism towards one’s job [ 12 ]. Burnout is directly related to increased psychological distress and unmitigated mental health issues in an apathetic environment. It has been shown to impact up to 40% of practicing doctors [ 13 , 14 ].
In 2019, 1.41 million students attempted the Indian medical school entrance exam; 797,000 passed and only 75,000 were selected. The course lasts over 5 years and is academically and personally demanding. Many undertake medical studies due to parental pressure rather than personal interest [ 15 ], potentially causing disillusionment and limiting help seeking.
India is home to the world’s largest population of people aged 10–24 years, and suicide is their leading cause of death [ 16 , 17 ]. ‘Academic trauma’ has been documented as a contributor to student suicide in a news report of nearly 10,000 students committing suicide in 1 year [ 18 ]. Separate data for medical students is however unavailable.
Several cross-sectional studies have examined the stress and overall well-being of Indian medical students by using various questionnaires. One study [ 19 ] using the Oldenburg Burnout Inventory and GHQ 12 reported high levels of burnout (88% and 81% for disengagement and exhaustion respectively) and high levels of mental health problems (62% with GHQ score >2). Two studies [ 20 , 21 ] using the Oldenburg Burnout Inventory have reported mean scores in Indian medical students, disengagement scores of 2.43 [ 20 ] and 18.16 [ 21 ], and exhaustion scores of 2.32 [ 20 ] and 13.89 [ 21 ] respectively. A different study [ 22 ] used the Maslach Burnout Inventory and reported 71% of the students showed moderate to high levels of burnout. Bute et al. [ 23 ] reported high levels of caseness indicating need for evaluation (66% with scores more than 4) amongst Indian medical students using the GHQ 28. Another study [ 24 ] using the same scale reported a mean score of above 7. Many other studies have examined the psychological well-being and mental health of Indian medical students [ 25 , 26 , 27 , 28 , 29 ]. The variety of instruments and scales used and methodological variations have resulted in a wide range of results. All studies were limited to students within a few medical colleges. There have yet been no nationally representative robust studies. Our study reports a nationally accessible large-scale survey on the well-being of medical students in India.
We conducted an online survey amongst medical student communities in India as part of a larger international effort to understand the stresses of medical student life. Matching surveys have been undertaken in countries such as Brazil [ 30 ], Morocco [ 31 ], and Jordan [ 32 ]. A similar study was also undertaken in four medical colleges of eastern and southern India [ 19 ].
This cross-sectional survey was conducted over the ‘Type Form’ platform, which presents survey questions sequentially and records respondent data. These data are collected and displayed graphically for each question. The survey link was disseminated to multiple medical student groups. A message accompanied the link to introduce the survey and its’ aims and to assure confidentiality and anonymity. Participant consent was sought in the beginning of the survey. The link was launched along with the message over multiple medical student groups across many colleges, predominantly by reaching out to student leadership and WhatsApp chat groups. The survey was open from 09/02/20 until 31/08/20. Fortnightly reminders were sent. As the circulation increased, a medical student magazine ‘Lexicon’ picked up the survey link and promoted it.
Survey questions included basic demographic details such as year of study, level of parental education, hours of work outside of student activities, current and past mental health difficulties, prescribed medications, and basic details of substance use. The short version of the ‘General Health Questionnaire’ (GHQ-12) [ 33 , 34 ] was included to screen for minor psychiatric disorders, with a score of 2 or more indicating caseness. The GHQ-12 has been used previously in Indian populations [ 35 ]. The CAGE questionnaire [ 36 ] was included to measure alcohol use with a score of more than 2, considered as ‘CAGE positive’. Lastly, the Oldenberg Burden Inventory [ 37 ] was included to identify burnout with threshold scores of 2.10 for disengagement and 2.25 for exhaustion [ 38 ].
Three hundred and forty-four respondents completed the survey. Of these respondents, three were removed as they were not medical students. There were respondents from New Delhi, Pondicherry, Vellore, Ludhiana, Bellary, and Bangalore amongst other sites.
Responses were spread across the training years as follows: 15% in the first year, 22% from the second year, 20% from year three, 12% from year four, 10% from year five, and 19% from year six. Two percent did not specify year of training.
Sixty percent of respondents identified as female, 39% identified as male, and one respondent identified as other gender.
Parental education levels for 46% were post-graduation; 35% were undergraduate degrees, while 13% were up to high school education.
Fifteen percent of respondents reported working for more than 20 h weekly. The majority of respondents (79%) did not work. Details of the sociodemographic details are presented in Tables 1 , 2 , 3 , 4 , and 5 .
Mental health
Before commencing their medical education, 27 respondents (8%) consulted a mental health professional, and five (2%) were given a mental health diagnosis. Diagnoses included mood disorder, anxiety disorder, adjustment disorder, and obsessive-compulsive disorder. Four respondents reported attention deficit hyperactive disorders. Seventeen (5%) students were on psychotropics. Twelve did not provide details, four (1%) were prescribed antidepressants, and one (0.3%) was prescribed benzodiazepines.
Thirty-six (11%) students reported that they were seeing a mental health professional at the time of the survey. Conditions reported included mood disorder, anxiety disorder, stress-related disorder, and obsessive-compulsive disorder. Twenty-four (7%) respondents reported being on prescription medications for their mental health. Nineteen (5%) were on antidepressants, three (1%) were on mood stabilisers, four (1%) were on sedatives, two (1%) were on antipsychotics, and one (0.3%) was on beta blocker. Twelve (4%) reported being prescribed stimulants for ADHD/ADD.
Two hundred and thirty-nine respondents (70%) reported academic work as a source of stress. One hundred and eighty (52%) respondents reported stress from relationships; eighty-eight (26%) reported stress due to financial reasons. Most respondents reported multiple stressors.
CAGE and substance use
Forty-nine (14%) respondents were CAGE positive. Thirty-three (10%) reported using a nonprescription substance to modify their mood to feel better. These nonprescription medications included sedatives, 13 respondents (4%); stimulants, six respondents (2%); antidepressants, five respondents (1%); and over the counter medications, three respondents (1%).
Forty (12%) students reported using cannabis, and five (1%) reported using hallucinogens. Nineteen (6%) of the respondents had used substances to enhance academic performance.
Fifteen (4%) respondents reported that someone close to them was worried about their substance use, and twenty-four (7%) reported being concerned about their own substance use.
GHQ-12 and OLBI score
The mean score of our sample was 5.26, and two hundred and thirty-nine (70%) respondents scored more than 2 in GHQ-12. The mean score for the group on the OLBI scale was 2.6. Two hundred and ninety-four (86%) of the respondents met the disengagement criteria for the OLBI scale while two hundred and seventy-five (80%) met criteria for exhaustion.
Comparisons before training and during training
Twenty-six (8%) respondents reported having had consultations with general practitioners and mental health professionals during the training. Eighteen (5%) of those who responded had only consulted before training and did not do so during their training.
Thirty-seven (11%) respondents reported being diagnosed with a mental health condition after the commencement of their medical training while only two (0.6%) reported being diagnosed in the past but not currently diagnosed. Four (1%) respondents were diagnosed in the past and continued with the diagnosis.
Association of sociodemographic factors with GHQ and OLBI scores
GHQ scores indicating ‘caseness’ were significantly associated with the first and sixth year of medical training. Higher GHQ scores were also reported for higher parental education levels ( p <0.05). We found an association between GHQ scores greater than two and a higher number of reported stressors ( p <0.05) (Ref. Table 1 ).
Disengagement and exhaustion were significantly associated ( p <0.05) with increasing number of stressors (Ref. Table 5 ).
Correlation of GHQ, OLBI, and CAGE scores
GHQ scores were positively correlated with the disengagement domain (correlation coefficient 0.511) and the exhaustion domain (correlation coefficient 0.521) of the OLBI scores. CAGE scores also positively correlated with the GHQ scores (correlation coefficient 0.136).
This was the first nationally accessible survey of medical student well-being in India. A previous study [ 19 ] used the same methods but was conducted in selected medical colleges. We used innovative approaches to recruit respondents. Our survey found that medical students were at greater risk of developing mental ill health than their age-matched peers. Further, it appears that medical training increases mental health morbidity. Only 2% of the respondents had a diagnosis prior to commencing their training while 12% reported being diagnosed after entering medical college. This is a sizeable increase meriting further research to identify aggravating and protective factors. An identical survey carried out a year ago reported that 10% of respondents had received a mental ill health diagnosis prior to entering medical school and that 15% did during medical school [ 19 ]. Rates in the overall literature vary, and this will at least in part be due to sampling and the use of different measures.
From the survey on types and number of stressors, analysis was done looking for associations between the scale measures and stressors. Statistically significant results were obtained regarding increased mental health disturbances and the number of stressors.
There appears to be an association between duration of medical training and mental health issues. It can be understood that many stressors are likely to have greater impacts during the first year and the last year of medical training. The former period is one of great change and uncertainty while the latter period is one of exam pressure and expectations. These periods should be the focus of support systems and measures.
This study demonstrates the need to optimise well-being and to decrease burnout in medical students, which is now known beyond doubt to be increasing amongst physicians throughout their careers [ 39 ]. We need to urgently develop initiatives to minimise morbidity and maximise an individual’s well-being and medical career. Some suggestions are listed below:
Emphasising the importance of well-being both in and away from the workplace
Increasing the amount of targeted support around mental health from medicaleducators/institutions
Stigma reduction and attitude changes that will allow a positive platform on which well-being and mental health optimization and/or treatment can be accessed
Based on the findings from Singh et al. [ 22 ], we endorse co-curricular activities to promote cohesion and development of secondary and tertiary support systems in the colleges. Yoga and meditation activities conducted in group formats may also be beneficial [ 40 ]. Emphasis on physical activity and sleep hygiene should be retained. Online social networks can complement existing more traditional ones. Robust peer mentoring systems and the training of faculty members may aid in surveillance and early detection of mental health issues. This may subsequently reduce morbidity for those affected and reduce dropout rates. Mental health promotion activities should also be a focus of student welfare activities.
Limitations
This study is a cross-sectional survey of a convenience sample available only in English. However, English is the medium of instruction during medical training in India. The questions used were easily understood English.
Implications
Findings from this study highlight high levels of burnout and psychological distress being experience by medical students in India. Mental health morbidity appears to increase in medical training. Further research is warranted to assess mental health morbidity and its’ contributing and mitigating factors amongst students pursuing professional and non-professional disciplines in India.
Medical students in India report high levels of psychological distress and burnout. Urgent attention and interventions are required from peers, teachers, and policy makers.
Availability of data and materials
Abbreviations.
Attention deficit hyperactive disorders/attention deficit disorder
General Health Questionnaire
International Classification of Diseases-11
Oldenburg Burnout Inventory
Moir F et al (2018) Depression in medical students: current insights. Adv Med Education Pract 9:323–333
Article Google Scholar
Sherina MS, Rampal L, Kaneson N (2004) Psychological stress among undergraduate medical students. Med J Malays 59(2):2017–2011
Google Scholar
Supe AN (1998) A study of stress in medical students at Seth G.S. Medical College. J Postgrad Med 44(1):1
CAS PubMed Google Scholar
Stewart SM et al (1999) A prospective analysis of stress and academic performance in the first two years of medical school. Med Educ 33(4):243–250
Article CAS PubMed Google Scholar
Saipanish R (2003) Stress among medical students in a Thai medical school. Med Teach 25(5):502–506
Article PubMed Google Scholar
Dyrbye LN, Thomas MR, Shanafelt TD (2006) Systematic review of depression, anxiety, and other indicators of psychological distress among U.S. and Canadian medical students. Acad Med:354–373
Dyrbye LN et al (2008) Burnout and suicidal ideation among U.S. medical students. Ann Intern Med 149(5):334–341. https://doi.org/10.7326/0003-4819-149-5-200809020-00008
Ashton CH, Kamali F (1995) Personality, lifestyles, alcohol and drug consumption in a sample of British medical students. Med Educ 29(3):187–192
Newbury-Birch D, Walshaw D, Kamali F (2001) Drink and drugs: from medical students to doctors. Drug Alcohol Depend 64(3):265–270
Rennie SC, Rudland JR (2003) Differences in medical students’ attitudes to academic misconduct and reported behaviour across the years - a questionnaire study. J Med Ethics 29(2):97–102. https://doi.org/10.1136/jme.29.2.97
Article CAS PubMed PubMed Central Google Scholar
Freudenberger HJ (1974) Staff burn-out. J Soc Issues 30(1):159–165
World Health Organisation. Burn-out an “occupational phenomenon.”: International Classification of Diseases. International Classification of Disease. 2019.
Henderson G (1984) Physician burnout. Hospital Physician 20(10):8–9
Langade D et al (2016) Burnout syndrome among medical practitioners across India: a questionnaire-based survey. Cureus 8:9
Jothula KY et al (2018) Study to find out reasons for opting medical profession and regret after joining MBBS course among first year students of a medical college in Telangana. Int J Community Med Public Health 5(4):1392–1396
UNFPA India | Young people (no date). (). Available at: https://india.unfpa.org/en/topics/young-people-12 .
Dandona R et al (2018) Gender differentials and state variations in suicide deaths in India: the Global Burden of Disease Study 1990–2016. Lancet Public Health 3(10):e478–e489
Student suicides rising, 28 lives lost every day - the Hindu (no date). (Accessed: 12 Nov 2020). Available at: https://www.thehindu.com/news/national/student-suicides-rising-28-lives-lost-every-day/article30685085.ece
Farrell SM et al (2019) Wellbeing and burnout in medical students in India; a large scale survey. Int Rev Psychiatry 31(7–8):555–562
Shad R, Thawani R, Goel A (2015) Burnout and sleep quality: a cross-sectional questionnaire-based study of medical and non-medical students in India. 7(10):e361
Goel A et al (2016) Longitudinal assessment of depression, stress, and burnout in medical students. J Neurosciences Rural Practice 7(4):493–498
Singh S et al (2016) A cross-sectional assessment of stress, coping, and burnout in the final-year medical undergraduate students. Ind Psychiatry J 25(2):179
Article PubMed PubMed Central Google Scholar
Bute J et al (2016) A cross-sectional study of mental well-being among undergraduate students in a Medical College, in Central India. Int J Med Science Public Health 5(9):1775
Nandi M et al (2012) Stress and its risk factors in medical students: an observational study from a medical college in India. Indian J Med Sci 66(1–2):1–12
Jena S, Tiwari C (2015) Stress and mental health problems in 1st year medical students: a survey of two medical colleges in Kanpur, India. Int J Res Med Sci 3(1):130–134
Venkatarao E, Iqbal S, Gupta S (2015) Stress, anxiety; depression among medical undergraduate students; their socio-demographic correlates. Indian J Med Res 141(3):354
Yuvaraj BY, Poornima S, Rashmi S (2016) Screening for overall mental health status using mental health inventory amongst medical students of a government medical college in North Karnataka, India. Int J Community Med Public Health 3(12):3308–3312
Anuradha R et al (2017) Stress and stressors among medical undergraduate students: a cross-sectional study in a private medical college in Tamil Nadu. Indian J Community Med 42(4):222
Garg K, Agarwal M, Dalal PK (2017) Stress among medical students: a cross-sectional study from a North Indian Medical University. Indian J Psychiatry 59(4):502–504
PubMed PubMed Central Google Scholar
Castaldelli-Maia JM et al (2019) Stressors, psychological distress, and mental health problems amongst Brazilian medical students. Int Rev Psychiatry 31(7–8):603–607
Lemtiri Chelieh M et al (2019) Mental health and wellbeing among Moroccan medical students: a descriptive study. Int Rev Psychiatry 31(7–8):608–612
Molodynski A et al (2020) Cultural variations in wellbeing, burnout and substance use amongst medical students in twelve countries. Int Rev Psychiatry
Goldberg DP, Blackwell B (1970) Psychiatric illness in general practice: a detailed study using a new method of case identification. Br Med J 2(5707):439–443
Article PubMed Central Google Scholar
Goldberg DP et al (1997) The validity of two versions of the GHQ in the WHO study of mental illness in general health care. Psychol Med 27(1):191–197
Chaturvedi SK et al (1994) Detection of psychiatric morbidity in gynecology patients by two brief screening methods. J Psychosom Obstet Gynaecol 15(1):53–58
Ewing JA (1984) Detecting alcoholism: the CAGE questionnaire. J Am Med Assoc 252(14):1905–1907
Article CAS Google Scholar
Demerouti E, Bakker AB (2007) Measurement of Burnout (and engagement) measurement of burnout and engagement. the Oldenburg Burnout Inventory: a good alternative to measure burnout (and Engagement)
Westwood S et al (2017) Predictors of emotional exhaustion, disengagement and burnout among improving access to psychological therapies (IAPT) practitioners. J Ment Health 26(2):172–179
Shanafelt TD, Dyrbye LN, West CP (2017) Addressing physician burnout the way forward. J Am Med Assoc:901–902
Ganpat T, Nagendra H (2012) Integrated yoga therapy for improving mental health in managers. Ind Psychiatry J 20(1):45
Download references
Acknowledgements
We would like to thank all the people who helped and the many students who took part.
No funding was required for this study.
Author information
Authors and affiliations.
Department of Psychiatry, NIMHANS, Bangalore, Karnataka, India
Sharad Philip & Santosh K. Chaturvedi
Oxford Health NHS Foundation Trust, Oxford, UK
Andrew Molodynski & Lauren Barklie
Oxford University, Oxford, UK
Andrew Molodynski
King’s College, London, UK
Dinesh Bhugra
You can also search for this author in PubMed Google Scholar
Contributions
SP contributed in planning the study, preparing the methodology and questionnaire, analysing the results, preparing the tables, writing the introduction and discussions, and reviewing, revising, and approving the final manuscript. AM contributed in planning the study, preparing the methodology and questionnaire, interpreting the results, writing the introduction and discussions, and reviewing, revising, and approving the final manuscript. LB contributed in preparing the methodology and questionnaire, writing the discussions, and reviewing, revising, and approving the final manuscript. DB contributed in planning the study, preparing the methodology and questionnaire, writing the discussions, and reviewing, revising, and approving the final manuscript. SKC contributed in planning the study, preparing the methodology and questionnaire, analysing the results, preparing the tables, writing the introduction and discussions, and reviewing, revising, and approving the final manuscript. The authors read and approved the final manuscript.
Corresponding author
Correspondence to Sharad Philip .
Ethics declarations
Ethics approval and consent to participate.
As per the Indian Council of Medical Research guidelines for online surveys, only participant consent is required. There is no requirement for ethics committee permissions. No ethical approval was deemed necessary by the national algorithm in the UK as this was an online population survey of consenting medical students irrespective of their health status. Only consenting subjects were included. Participant consent was sought in the beginning of the survey.
Consent for publication
The authors have consented to publication.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ .
Reprints and permissions
About this article
Cite this article.
Philip, S., Molodynski, A., Barklie, L. et al. Psychological well-being and burnout amongst medical students in India: a report from a nationally accessible survey. Middle East Curr Psychiatry 28 , 54 (2021). https://doi.org/10.1186/s43045-021-00129-1
Download citation
Received : 12 July 2021
Accepted : 18 July 2021
Published : 24 August 2021
DOI : https://doi.org/10.1186/s43045-021-00129-1

Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Medical students
Advertisement
Lack of research amongst undergraduate medical students in India: It’s time to act and act now
- Perspective
- Published: 29 March 2017
- Volume 54 , pages 357–360, ( 2017 )
Cite this article
- Rajesh Garg 1 , 3 ,
- Shobha Goyal 2 &
- Kamaljit Singh 1
104 Accesses
12 Citations
7 Altmetric
Explore all metrics
Participation in research is important in producing doctors with an understanding of evidence-based medicine. Though a mandatory part in post-graduate medical course, research has largely been invisible from the under graduation medical course in India. Very few research opportunities are available at under graduate level. The reason behind this is lack of encouragement, lack of basic infrastructure, facilities and structured mentorship programs, no extra incentives to researchers and the long journey to get academic acclaim. Another additional aspect is of lack of writing skills for biomedical publication. Additional incentives to students as well faculty members are required to foster the research environment in India.
This is a preview of subscription content, log in via an institution to check access.
Access this article
Price includes VAT (Russian Federation)
Instant access to the full article PDF.
Rent this article via DeepDyve
Institutional subscriptions
Similar content being viewed by others
Carrying out research in Nepal: perceptions of scholars about research environment and challenges
Prakash Kumar Paudel & Basant Giri

Ethical oversight of student data in learning analytics: a typology derived from a cross-continental, cross-institutional perspective
James E. Willis III, Sharon Slade & Paul Prinsloo

Understanding the role of the paramedic in primary care: a realist review
Georgette Eaton, Geoff Wong, … Kamal R. Mahtani
Wickramasinghe DP, Perera CS, Senarathna S, Samarasekera DN. Patterns and trends of medical student research. BMC Med Educ. 2013;13:175.
Article PubMed PubMed Central Google Scholar
Stringer MD, Ahmadi O. Famous discoveries by medical students. ANZ J Surg. 2009;79:901–8.
Article PubMed Google Scholar
Carter JB, Luckhardt AB. Discoveries by medical students. JAMA. 1956;160:504.
Google Scholar
Ohry A. Outstanding discoveries made by medical students. Prog Health Sci. 2012;2:162–70.
Dangayach NS, Kulkarni UP, Panchabhai TS. Mentoring medical student research through studentships and fellowships: Reflections from India. J Postgrad Med. 2009;55:152–3.
Article CAS PubMed Google Scholar
United Nations Educational, Scientific and Cultural Organization. Institute for Statistics. Country profiles: India. Human Resources in Research and Experimental Development (RandD). Available from: http://www.uis.unesco.org/DataCentre/Pages/countryprofile.aspx?region code=40535andcode=IND . Accessed May 26, 2016.
Gupta BM, Bala A. Scientometric analysis of Indian research output in medicine during 1999–2008. J Nat Sci Biol Med. 2011;2:87–100.
Article CAS PubMed PubMed Central Google Scholar
Lal S. Scenario of Postgraduate Medical Education in Community Medicine in India. Indian J Community Med. 2004; 29:56–61.
Garg R, Gupta S. Are we really producing public health experts in India?: Need for a paradigm shift in postgraduate Teaching in Community Medicine. Indian J Community Med. 2011;36:93–7.
National Health Research Policy 2011. Department of Health Research. Ministry of Health and Family Welfare, Government of India. New Delhi. Available from: http://www.dhr.gov.in/annual_report/2011-12/national_health.pdf . Accessed May 26, 2016.
Ray S, Shah I, Nundy S. The research output from Indian medical institutions between 2005 and 2014. Curr Med Res Pract. 2016;6:49–58.
Article Google Scholar
Shankar PR, Chandrasekhar TS, Mishra P, Subish P. Initiating and strengthening medical student research: Time to take up the gauntlet. Kathmandu University Med J. 2006;4:135–8.
CAS Google Scholar
Remes V, Hellineus I, Sinisaari I. Research and medical students. Med Teach. 2000;22:164–7.
Abraham D, Swamy RS. Perspectives in Mentorship and Mentoring Programs in Post-graduate Medical Education and Beyond: An Indian viewpoint. J Educational Res Med Teacher. 2015;3:1–4.
Aggarwal R, Gogtay N, Kumar R, Sahni P, Indian Association of Medical Journal Editors. The revised guidelines of the medical council of India for academic promotions: Need for a rethink. Indian Pediatr. 2016;53:23–6.
Chaturvedi S, Aggarwal OP. Training interns in populationbased research: learners’ feedback from 13 consecutive batches from a medical school in India. Med Educ. 2001;35:585–9.
Harsha HN, Jayaram S, Kumar GS, Vinita J, Rohit S, Satish M, et al . Perception, practices towards research and predictors of research career among UG medical students from coastal South India: A cross-sectional study. Indian J Community Med. 2009;34:306–9.
Datta SS, Boratne AV, Singh Z. Attitude, perception and demand for research among medical undergraduates in a teaching medical institution in South India. Indian J Publ Health Res Develop. 2012;3:139–43.
Houlden RL, Raja JB, Collier CP, Clark AF, Waugh JM. Medical students’ perceptions of an undergraduate research elective. Med Teach. 2004;26:659–61.
Ogunyemi D, Bazargan M, Norris K, Jones-Quaidoo S, Wolf K, Edelstein R, et al . The development of a mandatory medical thesis in an urban medical school. Teach Learn Med. 2005;17:363–69.
Kasulkar AA, Gupta M, Chari S, Kanade HT. Assessment of medical students’ interest in research in central India. J Evolution Medi Dent Sci. 2013;2:5375–81.
Ratnayake GM, Jayasena GM, Weeratunga PN, et al . Medical student research output in a developing country: Where has all the research gone? Med Teach. 2012;34:998.
PubMed Google Scholar
The Indian Council of Medical Research. Grant Schemes. Short Term Studentship. Available from: http://www.icmr.nic.in/Grants/Grants.html . Accessed May 26, 2016.
Kishore Vaigyanik Protsahan Yojana (KVPY). Government of India. Available from: http://kvpy.iisc.ernet.in/main/eligibility.htm . Accessed May 18, 2016.
National Defence Fund. Salient Features of “PM’s Scholarship Scheme” being implemented out of National Defence Fund. PMINDIA. Available from: http://pmindia. gov.in/en/national-defence-fund/ . Accessed May 26, 2016.
Indian Oil for Society. Indian Oil Educational Scholarship Scheme 2014. Available from: https://iocl.com/aboutus/scholarships.aspx . Accessed May 26, 2016.
Deo MG. Undergraduate medical students’ research in India. J Postgrad Med. 2008;54:176–9.
The Forum for Medical Students’ Research. INFORMER-Observation beyond Vision. Available from: http://www.informer.org.in/about-us/vision . Accessed May 26, 2016.
Download references
Author information
Authors and affiliations.
Department of Community Medicine, MM Medical College, Solan, Himachal Pradesh, India
Rajesh Garg & Kamaljit Singh
Department of Dentistry, MM Medical College, Solan, Himachal Pradesh, India
Shobha Goyal
H No 1000, Sector 19, Part - 2, HUDA Colony, Kaithal, Haryana, 136 027, India
Rajesh Garg
You can also search for this author in PubMed Google Scholar
Corresponding author
Correspondence to Rajesh Garg .
Rights and permissions
Reprints and permissions
About this article
Garg, R., Goyal, S. & Singh, K. Lack of research amongst undergraduate medical students in India: It’s time to act and act now. Indian Pediatr 54 , 357–360 (2017). https://doi.org/10.1007/s13312-017-1104-4
Download citation
Published : 29 March 2017
Issue Date : May 2017
DOI : https://doi.org/10.1007/s13312-017-1104-4
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Publication
- Scholarship
- Find a journal
- Publish with us
- Track your research
Call for papers - Medical education in India
Guest Editors: Anne D. Souza: Manipal Academy of Higher Education, India Olwyn Westwood: King’s College London, UK
Submission Status: Open | Submission Deadline: 7 August 2024

Articles will undergo the journal’s standard peer-review process and are subject to all of the journal’s standard policies . Articles will be added to the Collection as they are published.
The Editors have no competing interests with the submissions which they handle through the peer review process. The peer review of any submissions for which the Editors have competing interests is handled by another Editorial Board Member who has no competing interests.

- Member Types & Privileges
- Registration
- INFORMER Logo
- Office Bearers
- Our history
- Vision Mission & Values
- Blog@Third I
Quick Links
Subscribe to our Mailing List
- Request new password
Error message
- Deprecated function : Return type of DatabaseStatementBase::execute($args = [], $options = []) should either be compatible with PDOStatement::execute(?array $params = null): bool, or the #[\ReturnTypeWillChange] attribute should be used to temporarily suppress the notice in require_once() (line 2244 of /home2/inforyjm/public_html/includes/database/database.inc ).
- Deprecated function : Return type of DatabaseStatementEmpty::current() should either be compatible with Iterator::current(): mixed, or the #[\ReturnTypeWillChange] attribute should be used to temporarily suppress the notice in require_once() (line 2346 of /home2/inforyjm/public_html/includes/database/database.inc ).
- Deprecated function : Return type of DatabaseStatementEmpty::next() should either be compatible with Iterator::next(): void, or the #[\ReturnTypeWillChange] attribute should be used to temporarily suppress the notice in require_once() (line 2346 of /home2/inforyjm/public_html/includes/database/database.inc ).
- Deprecated function : Return type of DatabaseStatementEmpty::key() should either be compatible with Iterator::key(): mixed, or the #[\ReturnTypeWillChange] attribute should be used to temporarily suppress the notice in require_once() (line 2346 of /home2/inforyjm/public_html/includes/database/database.inc ).
- Deprecated function : Return type of DatabaseStatementEmpty::valid() should either be compatible with Iterator::valid(): bool, or the #[\ReturnTypeWillChange] attribute should be used to temporarily suppress the notice in require_once() (line 2346 of /home2/inforyjm/public_html/includes/database/database.inc ).
- Deprecated function : Return type of DatabaseStatementEmpty::rewind() should either be compatible with Iterator::rewind(): void, or the #[\ReturnTypeWillChange] attribute should be used to temporarily suppress the notice in require_once() (line 2346 of /home2/inforyjm/public_html/includes/database/database.inc ).
WHO ARE WE?
India is a country which contains hundreds of medical colleges and thousands of medical students graduating each year. A fair number of students actively involve themselves in research at a local or national or even international level. INFORMER, The Forum for Medical Students' Research, India is a step towards bringing those interested in research to a common platform.

INFORMER is an all India medical students' body aimed at advocacy and promotion of research amongst undergraduate medical students and to encourage them to present their research work at a national level by means of the annual conference organized by the forum. It is an institution comprising of a group of medical students who attempt to keep the spirit of research alive among the student community. INFORMER was formed in 2009 in response to there being a lack of an advocate for undergraduate medical students in the country. Over the past 3 years, we have diversified base of activities which now include our annual flagship conference (Medicon), an online journal club,collaborative research projects, a research project mentoring forum, workshops which promote evidence-based medicine,medical quizzes, case presentation conferences etc.
Recent Updates
Topic: Medical Research in India Past and Future
We are as young as our faith and old as our doubts. APJ Abdul Kalam
Write an essay on the topic in less than 1500 words and win cash prizes. 1st Prize- Rs.10000/-, 2nd Prize- Rs.7000/-, 3rd Prize-Rs.5000/-
Instructions:
-BMJ India has teamed up with Fortis C-DOC Center of Excellence for Diabetes, Metabolic Diseases & Endocrinology, New Delhi to provide educational support for health professionals to improve care for people with diabetes in India. Learn more about their course and how to sign up.-
Greetings from the 50th year council of Chengalpattu Medical college, Chengalpattu, Tamil Nadu. www. www.chemfest.in/charm.html
We, the students of this famed institution take immense pleasure in introducing to you our annual academic extravaganza – the 3rd CHARM-CHengalpattu Academic and Research Meet, to be conducted at our college premises, in September 2015
Abstract submission deadlines for Medicon 2015 have been extended to 30 June 2015. This is owing to certain colleges having examinations around the previous deadline. Hope you will be able to complete abstract submission within that time.
The wait is over ... Call for ICMR STS 2015 is out
Read all updates
Undergraduate medical students' research in India
- PMID: 18626161
- DOI: 10.4103/0022-3859.41796
Publication types
- Biomedical Research / education*
- Biomedical Research / organization & administration
- Education, Medical, Undergraduate / organization & administration*
- Students, Medical*
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- v.14(5); 2022 May

Medical Education and Research in India: A Teacher’s Perspective
Venkataramana kandi.
1 Clinical Microbiology, Prathima Institute of Medical Sciences, Karimnagar, IND
Medical education is a systematic process wherein interested and eligible individuals are trained to become physicians/surgeons. It is assumed that a person who completes the Bachelor of Science and Bachelor of Medicine (MBBS) degree will be competent enough to perform the duties of a physician of first contact. However, it is not the case with graduates from India. Most MBBS graduates prefer to pursue a postgraduate degree and become unavailable to people or governments. The doctor-to-patient ratio in India (1:1,655) does not currently satisfy the World Health Organization’s prescribed ratio (1:1,000). The Government of India, therefore, has been taking initiatives to increase the number of MBBS graduates. Moreover, there are several doubts over the quality of medical education and the competency of medical students. In addition, the National Medical Commission, the epic body that regulates the medical education and practice in India, has recently been conducting medical education technology workshops to improve teachers and has devised a new curriculum to elevate the standards of medical education in India. This editorial attempts to provide readers with the current status of medical education and research in India.
The Indian medical education system has recently seen a makeover in the form of a change in the curriculum. This change may have become inevitable due to growing concerns, both within the country and globally, over the low standards and quality of MBBS graduates. It has been widely accepted that medical students graduating from Indian institutions are not competent enough to practice. This is evident by the requirement for medical graduates from India to clear the United States Medical Licensing Examination (USMLE) to practice in the United States. Therefore, the National Medical Commission (NMC), previously known as the Medical Council of India (MCI), has come forward with a vision to revamp medical education in India. The main motto of this initiative by the NMC is to ensure that Indian medical graduates (IMG) are competent enough to function as community physicians of first contact [ 1 ]. This decision by the Government of India (GOI) was taken after considering the high disease burden among people, as well as the huge disparities in the status of medical institutions/establishments/facilities/services within different geographical regions of the country. Moreover, the NMC has made it mandatory for all medical teachers to undergo a training program on medical education technology (MET). The NMC regularly conducts basic and advanced workshops/courses for all medical teachers in the country. However, the NMC appears to have ignored the most significant aspect that could potentially contribute to the success of a teacher/learner in medical education. The attitudes of both the teachers and learners significantly influence the learning outcomes, thereby affecting the competency of medical graduates. Carefully designed faculty development programs may contribute to medical teachers’ professionalism, management, and leadership abilities that further enable students to become competent physicians [ 2 ].
The current scenario
Most medical teachers, especially those who participate in the teaching of students in their I MBBS and II MBBS may be considered accidental teachers. Although this is not usually considered a topic for discussion, it must be noted that the first two years of the MBBS course function as a foundation for students. During this period, students learn basic subjects, including anatomy, physiology, biochemistry, pathology, microbiology, and pharmacology. Basic and comprehensive knowledge of these subjects is considered extremely useful to understand the clinical subjects that the students pursue from the third year of the MBBS course. However, in practice, disinterested teachers are misguiding students to learn the subjects from an examination point of view rather than emphasizing the importance of the role played by pre and para-clinical subjects for the rest of their future in the medical profession (clinical relevance and integrated approach). The scenario may be the same with teachers who opt for less familiar clinical degrees after having compromised on their specialization of interest. Unfortunately, specializations gain familiarity based on the expected earnings they can get during the practice and not particularly about the interest/skills they have concerning the subject/specialization.
The NMC and GOI’s decision to improve the doctor-to-patient ratio has indirectly affected the teacher-to-student ratio. With increased numbers of medical institutions being permitted and more in the pipeline, there is a continuous movement of faculty resulting in transient deficiencies of faculty that directly affects the quality of curriculum delivery despite the improvement/change in the curriculum, as envisaged by the NMC recently. Further, the NMC and the GOI must consider the numbers of MBBS and MD (Doctor of Medicine) graduates who move out of the country for livelihood and other reasons. Interestingly, not many medical graduates were available who volunteered during the initial days of the coronavirus disease 2019 (COVID-19) pandemic. Therefore, public and private healthcare facilities were forced to work with medical students (house surgeons/interns/final MBBS students) and fresh MBBS graduates. The main reason is that MD graduates belonging to the pre and para-clinical subjects, sparing a few, lose their connectivity to medicine and lack the confidence to examine patients. This aspect needs serious consideration by the GOI, NMC, local governments, as well as the doctors themselves, who should make efforts to provide their services by running evening community clinics.
Admission for entry into the MBBS course is currently carried out based on reservations following the caste system that is prevalent in India. A significant percentage of seats are filled based on the student’s capability to pay fees, and some are accommodated to the non-resident Indian (NRI) category. Similarly, the admission of students is based on a competitive multiple-choice-based examination that does not evaluate students’ interests and attitudes and merely evaluates their theoretical knowledge. These are the main reasons for the deteriorating quality of medical graduates in India. Conversely, the deterioration in quality comes from the fact that the concepts that were described in the medical education workshops are not pursued by the majority of faculty members across medical colleges in India. Compared to the olden days, currently, teachers are not spending enough time with students and patients, especially in the clinical departments.
Medical teachers
Teachers appointed in medical institutes are required to have an MD degree in the respective subjects. However, the NMC has allowed the appointment of non-medical teachers (teachers without an MBBS degree) for up to 30% (50% in biochemistry) in both pre and para-clinical subjects excluding the department of pathology [ 3 ]. This was mainly due to the lack of qualified MD teachers available for the job. Recently, the change in the medical education curriculum with more emphasis on competency and competency-based medical education (CBME) has forced the NMC to reconsider the appointment of non-medical teachers. Therefore, NMC has decided to reduce the number of non-medical teachers in the anatomy, physiology, and biochemistry departments, and stop the recruitment of such teachers to the microbiology and pharmacology departments. The decision of the NMC regarding non-medical teachers was long pending with complaints about such teachers emerging over the years both from students as well as teachers with MD degrees. The major reason for the NMC’s decision to minimize and remove non-medical teachers is because the GOI and the NMC have already given a green signal/approval for admission into several MD courses in these departments. On the contrary, many MBBS graduates who fail to pursue a clinical MD/MS degree have been opting for non-clinical (pre and para-clinical) MD subject specialization courses. However, this decision by the NMC had some drawbacks. The major one is the lack of interest among MBBS graduates admitted in the concerned subject of specialization. After joining the courses, these students face difficulties in completing the course at the designated time. Moreover, the mandatory dissertation required for them to complete the course is not done with the required/desired technical and ethical standards.
In contrast to a Ph.D. degree, wherein the pursuant does research work for at least three years to become eligible for the award of the degree, MD graduates work as part-time teachers (tutor/junior resident/senior resident) and are able to complete the course within three years. All universities in India come under the aegis of the Union Grants Commission (UGC). However, medical institutions and medical universities function under the umbrella of the NMC. The UGC mandates that Ph.D. students publish at least two original research articles in reputed journals and present at least one abstract in a national/international conference to become eligible to be awarded the degree. This is in complete contrast to the MD degree, wherein the students only undertake research work for a maximum period of one year, and it is not mandatory to publish/present papers in journals/conferences. Moreover, the period during the MD study is considered a teaching experience in the position of resident/tutor/demonstrator. Therefore, MD degree holders become eligible for appointments as assistant professors after the study period. This points to the fact that an MD degree must not necessarily be considered a research degree. The UGC has a mechanism wherein the Ph.D. thesis and postgraduate dissertations submitted by the students are deposited in a repository (Shodhganga) and are carefully screened for plagiarism before they are approved/accepted. The Information and Library Network Centre (INFLIBNET) is an autonomous interuniversity center of the UGC [ 4 ]. However, even today, this practice is not followed by medical universities. Therefore, MD dissertations are generally not as standard as Ph.D. theses. Medical Universities, in the future, should consider screening all MD dissertation submissions for potential plagiarism and make the dissertations available in the public domain (similar repository as the INFLIBNET). Several institutions do not support the financial aspects of the MD dissertation, and this limitation could be the reason why the students are unable to pursue real research and finally end up writing dissertations without even working on the topic. This situation can be improved by active vigilance by the NMC and at the institutional level regarding the MD dissertations and their standards. Given the above observations, the matter of equivalence of an MD degree with a Ph.D. degree appears to be questionable. However, medical universities in India and autonomous research institutes funded by the GOI are accepting/recognizing MD degree holders as Ph.D. guides. Such practices should be re-evaluated by higher education bodies/councils because it affects the standards of Ph.D. holders and their future in research activities.
Medical research
Medical teachers who were not properly trained in research end up being not interested in pursuing research after obtaining their degrees. This probably was the main reason why the NMC was particular about the research publications requirement for promotions. However, medical teachers find it difficult to do even these mandatory research publications. This is majorly attributed to the lack of financial and logistic support from the public and private administrations. The lack of proper research orientation among medical teachers appears to have significantly impacted the research inclination of students. Moreover, medical institutions have not been supportive of the research activities of both the faculty and students. The GOI, under the Indian Council for Medical Research, has been implementing limited numbers of short-term studentship (STS) research fellowships (two-month duration) for medical students [ 5 ]. Despite this initiative, many more interested students will remain unbenefited. This issue may be addressed by the institution by devising a mechanism wherein research-oriented faculty may be roped into a group (research wing) that mainly functions to facilitate interested students to pursue research work under able faculty members. Because research work involves financial implications, medical institutions must create a fund (crowdfunding, donations, corpus, others) that potentially serves this purpose.
The criteria for promotion that requires a medical teacher to have published at least two papers in an indexed journal also appear to be responsible for the deterioration of research standards among medical teachers and institutions. This decision by the NMC was instrumental in the emergence of several predatory journals that claim to have been indexed by the agencies recognized/prescribed by the NMC. However, the NMC realized and changed its decision and excluded the Index Copernicus as the desired indexing agency that was responsible for the emergence of pay-to-publish journals. Interestingly, the NMC recently added the Indian Citation Index to the list of desired indexing agencies along with others that are already present, including PubMed, Scopus, DOAJ, and EMBASE, among others. Given unethical research and publication practices, the NMC may choose to accept literature reviews as an acceptable type of article in consideration for promotions. This will enable faculty members to pursue research and get increasingly acquainted with current trends with extremely limited resources and encourage within-country and foreign collaborations.
Other concerns
Despite several positive changes by the NMC, medical institutions are further plagued by the problems of ghost faculty, ghostwriters, and other malpractices related to examinations, research, dissertation work, and publications. The factors that potentially affect medical education and research in a medical institution are depicted in Figure Figure1 1 .

Ghostwriter
Ghostwriters are anonymous persons who write manuscripts (that in this case are represented by research publications) for teachers who require them for promotions. A ghostwritten research article is used by a teacher to his/her credit by implanting his/her name on it and without mentioning the person who has written it. Moreover, ghostwritten articles are not necessarily written based on authentic data collected after conducting bench work. These amount to malicious practices under the recommendations by the Committee of Publication Ethics (COPE). Ghostwriters have been in full function helping several medical teachers to acquire research publications required for promotions. The problem with ghostwriting is that authors claim a work neither by doing nor by writing. Such literature that is written without actually working and available as published content in the public domain will adversely influence the scientific community and public health.
Ghost faculty
It has been a frequent occurrence in the past decade, wherein medical teachers representing more than one medical college appear before the NMC during inspections. However, NMC did identify this problem and punished several such medical faculties. There was also a problem of duplicate faculty wherein the certificates of a medical person were used to wrongly represent the faculty. Despite strict vigilance by the NMC, the newest trend is the ghost faculty. Medical colleges call upon qualified medical graduates during the inspection and show them as resident faculty members to the NMC. It is an open secret that is followed ubiquitously by several institutions throughout India. Interestingly, the faculty list shown by the institutes could range between 15 and 20 in each department during the inspection days. However, once the NMC inspection is completed, the actual faculty that works on the ground is considerably low in numbers (hardly 10). This significantly affects the faculty-to-student ratio. Assuming a college has 200 students, and the college shows 15 staff during the inspection, the actual number of teachers working on the ground will be less than 10. This results in overcrowding during practical demonstrations, and, for this reason, many students do not follow/understand the practical aspects. Moreover, with a smaller number of faculty members, teachers do not function in the manner that allows them to train each student adequately. Several practicing doctors and academically uninterested graduates are approached by the institutions. Due to the financial favors offered by institutions, medical graduates agree to be on the rolls of the college.
The ghost faculty who regularly present themselves to the NMC during the inspection do not even take a single theory/practical class. However, institutes promote them regularly based on the number of years of experience, despite the fact that the person has never attended the college in person, nor has he/she taken a single class. The ghost faculty issue emerges because there is a frequent increase in the number of medical colleges.
Admission requirements for entry into the MBBS course also require serious considerations. More than half of the admissions currently are carried out based on reservations based on the caste system that is prevalent in India. Although the remaining seats are considered open, a significant percentage are filled based on the student’s capability to pay fees, and some are accommodated as NRIs. This implies that the merit of students is grossly ignored, and admissions, therefore, in the current situation do not guarantee the entry of qualified students who are willing and motivated to pursue the course.
Currently, India has the highest number (>600) of medical colleges in country-wise statistics. However, the medical education quality and standards of medical graduates have been under the scrutiny of the GOI and the NMC. A mere change in the curriculum and faculty training does not necessarily guarantee standards. Increased vigilance, uniform salaries, peer evaluation of research publications used for promotions, support and encouragement for faculty pursuing research, continuing medical education in the form of workshops/seminars/symposiums/conferences, and extensive student feedback are mandatory to further strengthen the quality of medical education and improve the standards of medical graduates in India. Recently, the UGC has decided to appoint non-Ph.D. teachers in universities for utilizing their vast experience and expertise. It is, therefore, imperative that subject expertise matters much more than the degree a person holds.
Teachers are role models for students, and to nurture future generations in the right direction, it is more than essential to improve the attitudes and quality of teachers. Further, it is the institutes that teach the society and the country as a whole regarding how systematically one should function to achieve desirable results. Therefore, institutes must take responsibility for establishing the best educational environment.
In conclusion, it should be noted that addressing the deteriorating standards and quality of medical education requires a multifaceted approach. The implementation of the new curriculum for undergraduates and medical education technology workshops for faculty members does not guarantee an improvement in the quality. Dedication from admitted students, faculty, and institution administration is equally important.
The content published in Cureus is the result of clinical experience and/or research by independent individuals or organizations. Cureus is not responsible for the scientific accuracy or reliability of data or conclusions published herein. All content published within Cureus is intended only for educational, research and reference purposes. Additionally, articles published within Cureus should not be deemed a suitable substitute for the advice of a qualified health care professional. Do not disregard or avoid professional medical advice due to content published within Cureus.
The authors have declared that no competing interests exist.
- Help & FAQ
Future specialization interests among medical students in southern india
- Department of Data Science, Manipal
- Department of Community Medicine, Kasturba Medical College, Mangalore
Research output : Contribution to journal › Article › peer-review
Background. A consideration of the future specialization interests of undergraduate medical students might help to understand the needs of higher medical education and future manpower availability for healthcare. Methods. A cross-sectional study was conducted among 373 undergraduate students of a medical college in southern India using a self-administered questionnaire. Results. Of the 373 students, 188 (50.4%) were men. Almost all of them (370 [99.2%]) wanted to pursue postgraduation. Of these, 267 (72.4%) wanted to pursue postgraduation in India. Overall, the first choice subject was surgery (120 [32.2%]) followed by internal medicine (85 [22.8%]) and paediatrics (43 [11.5%]). The third preference for men and women differed, with men choosing orthopaedics and women choosing obstetrics and gynaecology. The factors that influenced the choice of specialization were interest in the speciality (Likert scale score 4.7), job satisfaction (4.6), employment opportunities (4.0), job security (4) and high income potential (3.9). Conclusion. It was evident from the proportion of students desiring to do postgraduation and their choice of specialties that most of them will end up working at hospitals instead of at primary healthcare centres. The deficiencies of certain specialists such as ophthalmologists are likely to persist. This is a cause for concern as the majority of our population lives in rural areas and there is already a maldistribution of doctors.
All Science Journal Classification (ASJC) codes
- General Medicine
Other files and links
- Link to publication in Scopus
- Link to citation list in Scopus
Fingerprint
- Students Social Sciences 100%
- Medical Student Social Sciences 100%
- Interest Social Sciences 100%
- Men Social Sciences 100%
- India Social Sciences 100%
- Man Medicine and Dentistry 100%
- Student Medicine and Dentistry 100%
- india INIS 100%
T1 - Future specialization interests among medical students in southern india
AU - Subba, S. H.
AU - Binu, V. S.
AU - Kotian, M. S.
AU - Joseph, N.
AU - Mahamood, A. B.
AU - Dixit, N.
AU - George, A.
AU - Kumar, P.
AU - Acharya, S.
AU - Reddy, P.
PY - 2012/7/1
Y1 - 2012/7/1
N2 - Background. A consideration of the future specialization interests of undergraduate medical students might help to understand the needs of higher medical education and future manpower availability for healthcare. Methods. A cross-sectional study was conducted among 373 undergraduate students of a medical college in southern India using a self-administered questionnaire. Results. Of the 373 students, 188 (50.4%) were men. Almost all of them (370 [99.2%]) wanted to pursue postgraduation. Of these, 267 (72.4%) wanted to pursue postgraduation in India. Overall, the first choice subject was surgery (120 [32.2%]) followed by internal medicine (85 [22.8%]) and paediatrics (43 [11.5%]). The third preference for men and women differed, with men choosing orthopaedics and women choosing obstetrics and gynaecology. The factors that influenced the choice of specialization were interest in the speciality (Likert scale score 4.7), job satisfaction (4.6), employment opportunities (4.0), job security (4) and high income potential (3.9). Conclusion. It was evident from the proportion of students desiring to do postgraduation and their choice of specialties that most of them will end up working at hospitals instead of at primary healthcare centres. The deficiencies of certain specialists such as ophthalmologists are likely to persist. This is a cause for concern as the majority of our population lives in rural areas and there is already a maldistribution of doctors.
AB - Background. A consideration of the future specialization interests of undergraduate medical students might help to understand the needs of higher medical education and future manpower availability for healthcare. Methods. A cross-sectional study was conducted among 373 undergraduate students of a medical college in southern India using a self-administered questionnaire. Results. Of the 373 students, 188 (50.4%) were men. Almost all of them (370 [99.2%]) wanted to pursue postgraduation. Of these, 267 (72.4%) wanted to pursue postgraduation in India. Overall, the first choice subject was surgery (120 [32.2%]) followed by internal medicine (85 [22.8%]) and paediatrics (43 [11.5%]). The third preference for men and women differed, with men choosing orthopaedics and women choosing obstetrics and gynaecology. The factors that influenced the choice of specialization were interest in the speciality (Likert scale score 4.7), job satisfaction (4.6), employment opportunities (4.0), job security (4) and high income potential (3.9). Conclusion. It was evident from the proportion of students desiring to do postgraduation and their choice of specialties that most of them will end up working at hospitals instead of at primary healthcare centres. The deficiencies of certain specialists such as ophthalmologists are likely to persist. This is a cause for concern as the majority of our population lives in rural areas and there is already a maldistribution of doctors.
UR - http://www.scopus.com/inward/record.url?scp=84872005629&partnerID=8YFLogxK
UR - http://www.scopus.com/inward/citedby.url?scp=84872005629&partnerID=8YFLogxK
M3 - Article
C2 - 23278783
AN - SCOPUS:84872005629
SN - 0970-258X
JO - National Medical Journal of India
JF - National Medical Journal of India
Get verified solutions to all your doubts
35 lakh questions, verified answers.
- MyU : For Students, Faculty, and Staff
Undergraduate student project explores potential light-based therapy for Raynaud’s phenomenon

April 17, 2024 — A pioneering group of undergraduate students and faculty member Steven Saliterman have developed a novel, non-pharmacologic therapy device that might someday help people with Raynaud’s phenomenon and disease, a blood-flow disorder.
The device shows so much promise for treating the condition that findings were recently published in Annals of Biomedical Engineering and clinical studies are planned to test the therapy’s efficacy.
The project started with a request from a physician for an effective, non-medicinal therapy that would treat his wife’s Raynaud’s phenomenon. The phenomenon reduces blood flow to areas of the body through blood vessel spasms in affected areas, often the fingers and toes. Symptoms can be triggered by cold temperatures, stress, and upsetting emotions.
With the goal of treating these symptoms, Prof. Saliterman; two undergraduate students, Jennifer Chmura and Brett Levac; and Jerry Molitor, an Associate Professor in the Division of Rheumatic and Autoimmune Diseases at the University of Minnesota Medical School, developed a low-energy blue light phototherapy device. They also worked with Vaughn Schmid, UMN Technology Commercialization, to identify and secure intellectual property on behalf of the University of Minnesota.
Biomedical engineering undergraduate students James Kerber and Kushal Sehgal, along with Levac, continued the development effort in Prof. Saliterman’s Medical Device Practicum course (BMEN 3151), with the intent of developing a suitable study instrument. Emily Wegner, a UMN undergraduate student studying physiology, also joined the team as they progressed to writing a study protocol and submitting their work for publication.
Previous studies in animal models had suggested that low-energy blue light stimulates the vasodilation of blood vessels through cellular signaling mechanisms. The team hypothesized that a similar blue-light therapy may mitigate the vessel spasms responsible for troublesome Raynaud’s symptoms.
The project team created four different iterations of the phototherapy device over many years, starting with simple foam-board mockups and progressing to full-scale subassemblies. The electronic circuitry was designed by the team and hand-wired to create various prototypes. One of the primary challenges for the research group was designing a low-level light source that produced the specific wavelength of blue light known to stimulate vasodilation.
Once the phototherapy device was complete, the project team received approval from the University of Minnesota Institutional Review Board (IRB) for their clinical study protocol.
During the Covid-19 pandemic, the team received special permission to complete over 20 trial runs of their clinical protocol as both healthy volunteers and research assistants, allowing the team to further refine the phototherapy instrument and study design.
On January 9, the team received a utility patent (U.S. 11,865,357) for light-based treatment devices and methods. Independent clinical studies will soon be conducted to determine the effectiveness of the blue-light phototherapy device in patients with Raynaud’s phenomenon.
Remarkably, the phototherapy device project began in 2017 and remains active, composed of an interdisciplinary team in the fields of biomedical and electrical engineering, intellectual property law, public health, rheumatology and internal medicine.
“It’s extraordinary that an undergraduate team of students has continued to work together for so long and achieve so much on such an important topic,” says Prof. Saliterman.
The team plans to continue refining the phototherapy technology, with the hopes that it can be used to develop marketable devices, such as a stationary treatment unit or wearable glove, that can help people with Raynaud’s phenomenon.
Read the paper and learn more about the project
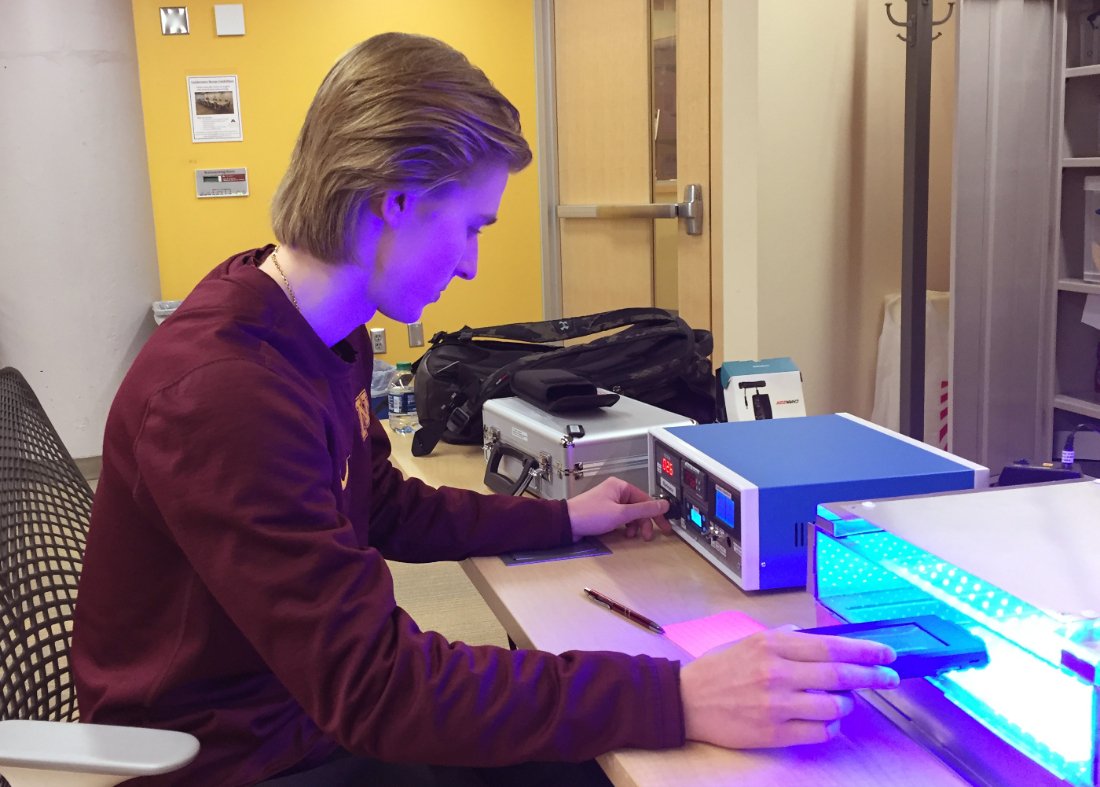
- Future undergraduate students
- Future transfer students
- Future graduate students
- Future international students
- Diversity and Inclusion Opportunities
- Learn abroad
- Living Learning Communities
- Mentor programs
- Programs for women
- Student groups
- Visit, Apply & Next Steps
- Information for current students
- Departments and majors overview
- Departments
- Undergraduate majors
- Graduate programs
- Integrated Degree Programs
- Additional degree-granting programs
- Online learning
- Academic Advising overview
- Academic Advising FAQ
- Academic Advising Blog
- Appointments and drop-ins
- Academic support
- Commencement
- Four-year plans
- Honors advising
- Policies, procedures, and forms
- Career Services overview
- Resumes and cover letters
- Jobs and internships
- Interviews and job offers
- CSE Career Fair
- Major and career exploration
- Graduate school
- Collegiate Life overview
- Scholarships
- Diversity & Inclusivity Alliance
- Anderson Student Innovation Labs
- Information for alumni
- Get engaged with CSE
- Upcoming events
- CSE Alumni Society Board
- Alumni volunteer interest form
- Golden Medallion Society Reunion
- 50-Year Reunion
- Alumni honors and awards
- Outstanding Achievement
- Alumni Service
- Distinguished Leadership
- Honorary Doctorate Degrees
- Nobel Laureates
- Alumni resources
- Alumni career resources
- Alumni news outlets
- CSE branded clothing
- International alumni resources
- Inventing Tomorrow magazine
- Update your info
- CSE giving overview
- Why give to CSE?
- College priorities
- Give online now
- External relations
- Giving priorities
- Donor stories
- Impact of giving
- Ways to give to CSE
- Matching gifts
- CSE directories
- Invest in your company and the future
- Recruit our students
- Connect with researchers
- K-12 initiatives
- Diversity initiatives
- Research news
- Give to CSE
- CSE priorities
- Corporate relations
- Information for faculty and staff
- Administrative offices overview
- Office of the Dean
- Academic affairs
- Finance and Operations
- Communications
- Human resources
- Undergraduate programs and student services
- CSE Committees
- CSE policies overview
- Academic policies
- Faculty hiring and tenure policies
- Finance policies and information
- Graduate education policies
- Human resources policies
- Research policies
- Research overview
- Research centers and facilities
- Research proposal submission process
- Research safety
- Award-winning CSE faculty
- National academies
- University awards
- Honorary professorships
- Collegiate awards
- Other CSE honors and awards
- Staff awards
- Performance Management Process
- Work. With Flexibility in CSE
- K-12 outreach overview
- Summer camps
- Outreach events
- Enrichment programs
- Field trips and tours
- CSE K-12 Virtual Classroom Resources
- Educator development
- Sponsor an event

IMAGES
VIDEO
COMMENTS
Objective of the study was to assess the knowledge, attitude and practice towards scientific research among undergraduate students of a medical college in Delhi, India.Methods: A cross sectional ...
The inclusion criteria were 1) Cross-sectional study design, 2) The study population was undergraduate medical students from India, 3) Assessing the prevalence of depression using a standardized instrument, and 4) The study period was from January 2019 to April 2022. ... services to undergraduate medical students. Research with large sample ...
100+ ICMR Research Topics: Unlocking Health Insights. General / By Stat Analytica / 20th November 2023. The landscape of healthcare research in India has been significantly shaped by the endeavors of the Indian Council of Medical Research (ICMR). Established in 1911, the ICMR has played a pivotal role in advancing medical knowledge, informing ...
M ATERIALS AND M ETHODS. Our institution started formal training of UGs in research as a part of the community medicine curriculum in 2002. The MBBS students undergo training in community medicine during their 1 st-year MBBS (1 st and 2 nd semesters), 2 nd-year MBBS (3 rd and 4 th semesters), and 3 rd-year MBBS (6 th and 7 th semesters). The students undergo the mandatory research methodology ...
A novel innovation in medical education was initiated by the Medical Council of India after 21 years. Competency-based medical education (CBME) is an effective outcome-based strategy, which requires integration of knowledge, attitude, skills, values, and responsiveness. The aim was to assess the students' perspectives on competency-based ...
The curriculum formulated by the Medical Council of India (MCI) exposed medical students to the basics of biostatistics and epidemiology during their training in community medicine at the Indian Medical School. ... The faculty briefs the students on topics ranging from the selection of journals and peer review process to plagiarism and ...
In India, students preparing to be medical doctors study Anatomy, Physiology and Biochemistry in the first year of their five and a half years coursework. 10 During the first year, in addition to lectures, students visit the dissection hall almost on a daily basis where they learn about the human anatomy. Dissection hall sessions help them in building an understanding of how the intricate ...
T1 - Fostering research skills in undergraduate medical students through mentored student projects. T2 - Example from an Indian medical school. AU - Devi, V. AU - Abraham, R. R. AU - Adiga, A. AU - Ramnarayan, K. AU - Kamath, A. PY - 2010. Y1 - 2010
Medical school can nurture the skill of research right from the under graduation. Research forms an integral part of the medical curriculum in western countries. We attempted the same in our medical school in India. We developed a structured research methodology program, which was implemented in the undergraduate (UG) curriculum in two phases.
Abstract. Background Medical educators in India made rapid adjustments to maintain continuity and integrity of medical education in the midst of disruption caused by the Covid-19 pandemic. However, there are concerns regarding achievement of competence by undergraduate medical students due to inadequate clinical exposure.
The rigours of medical education are well-known internationally, and medical students' mental health morbidity is higher than that of their aged-matched peers [].Medical students are prone to anxiety, depressive disorders, and high levels of psychological distress [2,3,4,5,6,7].Such issues may progress to negatively impact academic performance, predispose to substance use, and/or encourage ...
Participation in research is important in producing doctors with an understanding of evidence-based medicine. Though a mandatory part in post-graduate medical course, research has largely been invisible from the under graduation medical course in India. Very few research opportunities are available at under graduate level. The reason behind this is lack of encouragement, lack of basic ...
BMC Medical Education is now welcoming new submissions to a Collection on the ever-evolving field of medical education in India, seeking to highlight novel approaches, best practices, and cutting-edge research in this country. Medical education in India stands at a pivotal juncture, with the landscape witnessing rapid transformations driven by advancements in medical science, technology, and ...
INFORMER is an all India medical students' body aimed at advocacy and promotion of research amongst undergraduate medical students and to encourage them to present their research work at a national level by means of the annual conference organized by the forum. It is an institution comprising of a group of medical students who attempt to keep ...
A bird's eye view of the current status of undergraduate medical research in India is given and the steps that need to be taken to promote research at the grass root level are discussed. 176 J Postgrad Med July 2008 Vol 54 Issue 3 In India, medical education has remained more or less static, and research is in a very poor state. Against this backdrop, the idea of promoting research culture ...
Undergraduate medical students' research in India. Undergraduate medical students' research in India. Undergraduate medical students' research in India J Postgrad Med. 2008 Jul-Sep;54(3):176-9. doi: 10.4103/0022-3859.41796. Author M G Deo. PMID: 18626161 DOI: 10.4103 ...
Abstract. Medical education is a systematic process wherein interested and eligible individuals are trained to become physicians/surgeons. It is assumed that a person who completes the Bachelor of Science and Bachelor of Medicine (MBBS) degree will be competent enough to perform the duties of a physician of first contact.
Methods. A cross-sectional study was conducted among 373 undergraduate students of a medical college in southern India using a self-administered questionnaire. Results. Of the 373 students, 188 (50.4%) were men. Almost all of them (370 [99.2%]) wanted to pursue postgraduation. Of these, 267 (72.4%) wanted to pursue postgraduation in India.
In India, undergraduate medical research is far from satisfactory and is worsened with the mushrooming of a large number of ill-equipped medical colleges. This fact is proved by a study, which reports that the 70% of medical students expressed the unawareness about research. In our country, medical education has remained more or less static ...
April 17, 2024 — A pioneering group of undergraduate students and faculty member Steven Saliterman have developed a novel, non-pharmacologic therapy device that might someday help people with Raynaud's phenomenon and disease, a blood-flow disorder.The device shows so much promise for treating the condition that findings were recently published in Annals of Biomedical Engineering and ...