8 Tips for How to Thrive as a Nurse With ADHD

Attention deficit hyperactivity disorder (ADHD) affects both men and women but in different ways. Due to the differences, women are often underdiagnosed or diagnosed late in life, which can be a barrier to treatment, a sense of understanding, and the ability to find community.
An underdiagnosis of ADHD significantly affects careers where women make up the majority of the workforce, which includes nursing. In 2021, 82.5% of nurses were women.
While ADHD poses challenges, people with ADHD typically have other skills, including:
- High levels of empathy
- Spontaneity
- High levels of courage
- Being able to hyper-focus on a task
On this page, we share the experiences of one nurse with ADHD, how she tackled school, and how she thrives today as a nurse.
Molly Foss is a registered nurse at a level 1 trauma center. She was diagnosed with ADHD when she was 29.
Foss didn’t answer the call to be a nurse right out of high school. She felt intimidated by the work, so she pursued something else first.
“When I realized that wasn’t working, I was very intimidated to go back to school,” she says. “I finally realized that it’s all just a series of small steps.”

How to Thrive as a Nurse or Nursing Student With ADHD
Nursing students with ADHD must find strategies to help them study and absorb the material. Many of those same strategies can be used after graduation to stay up to date with research and nursing procedures. Before you can develop strategies, you must have a grasp of your own limitations and needs, which may be different than others with ADHD.
Self-awareness is the first step to creating tactics that help overcome your specific challenges. Foss has discovered that the medication prescribed to her is her No. 1 asset.
“Taking my medication is like putting on my glasses in the morning,” she says. “Everything goes from equally foggy and blurry to clear and obvious.”
While medication can help, lifestyle changes are what contribute to finding your groove with ADHD and maintaining it.
Foss also has created an assignment sheet. The sheet has tick boxes for most of the information she must track for patient care during her shift.
“More neurotypical people make their sheet on a blank piece of paper, I assume, because their brain is more organized,” she says. “My brain isn’t so organized, which is why I need my report sheet to be over-organized with a spot for everything.”
8 Tips for Nursing Students and Nurses With ADHD
Students and nurses with ADHD may help reduce the frustration and challenges accompanying the diagnosis by using tips and tricks others have discovered. These tips can be used independently or combined. They might also inspire another strategy that helps you in school, at work, or in your daily activities.
1. Use Flashcards
Students find consistent, repetitive exposure to information can help retention. Flashcards are a quick way to test yourself while involved in other activities. Movement and altering the environment can help to engage your brain in learning. Consider flashcards while eating, playing games, or when you’re out for a walk.
2. Change Your Environment
Students with attention deficit hyperactivity disorder find studying in the same environment for an extended period of time challenging. Consider moving your study space every hour or two. Don’t limit this space to the library or your home. Instead, include a coffee shop, park, restaurant, or a student lounge on campus.
Anywhere you can sit and comfortably study is fair game.
3. Ask for Help
Contact the school’s office for students with disabilities. You’ll need documentation of your diagnosis but this will give you access to accommodations that can help you succeed in school.
“One of the students in my class was allowed to take tests in a quiet room so they wouldn’t be distracted by everyone else,” Foss says.
4. Seek Out Resources
Students and working nurses need access to resources that help increase their level of success and to better understand ADHD, its origins, and its impacts. ADDitude magazine is one resource Foss recommends. Reading the articles helped her feel seen and not ignored by society. The magazine is full of resources, tips, and stories for adults with ADHD and parents with children who have ADHD.
Additionally, Dr. Gabor Maté, who has ADHD himself, authored “Scattered,” which helps readers understand their ADHD diagnosis, the origins of ADHD, and how to heal and reduce the impacts of ADHD.
5. Try the Pomodoro Technique
This strategy works with the short attention span that many people with ADHD experience. The Pomodoro Technique is a time management tool that sets a 25-minute limit on the amount of time you work on any assignment before taking a scheduled five-minute break. After the fourth break, you schedule a longer 15- to 30-minute break. Of course, you can alter the 25-minute work time to fit your personal needs without extending it past 30 minutes.
6. Practice Flexibility and Self-Compassion
No one is a robot. It’s important to recognize when you may be hyper-focused or highly productive. Take this time to work on projects that require more brainpower.
When you have trouble focussing, have self-compassion and use the time to relax or work on something that doesn’t require as much attention, such as creating flashcards. The trick is to be flexible with your schedule to work with your flow of attention and not against it.
4. Create Structure
New nursing students may enjoy the lack of structure and freedom they experience as a first-year college student. But for students with ADHD it can be a recipe for disaster. Instead, create your own structure for studying and develop an accountability system, so you aren’t on your own. Don’t forget to include downtime and recreational activities. They are important for your mental health.
5. Consider Treatment
Many with ADHD find that medication helps calm their mind and allows them to focus productively on tasks necessary for school and work. Many of the medications used are stimulants, yet they help people with attention deficit hyperactivity disorder function calmly and sleep better.
Additionally, cognitive behavioral therapy and environment modification can ease symptoms and help you cope better.
6. Prioritize Your Treatment
You can’t take care of your patients, family, or life if you aren’t taking care of yourself. Set an alarm to take your medication on time, create and stick with coping strategies that help you at school or work, and connect with others who have ADHD.
When you feel understood and appreciated for who you are, it can help raise your motivation to care for yourself so you can care for others.
7. Clear Your Mind
Frequently stopping what you’re doing to address an idea or thought that popped into your mind can mess up your day and impact patient care. Instead, carry a small notepad or your cell phone where you can write down the idea and address it later when you don’t have so much on your plate.
8. Take Things One Step at a Time
Just out of high school, Foss felt a calling to be a nurse. Terrified of the schooling and being able to work as a nurse, she chose to do something else. She soon realized the career wasn’t working but figured out that changing was really only a series of small steps.
“Right out of high school, I told people I wasn’t going to a university because I ‘didn’t have a four-year attention span.’ Now I have two two-year degrees and my BSN. Take the first step, even if it’s scary,” she says.
How ADHD Impacts Nurses and Nursing Students
The symptoms and manifestations of attention deficit hyperactivity disorder in adults can differ from those in children. Adults not diagnosed in childhood may not seek support at work or school. Yet, up to 5% of adults have ADHD, affecting their relationships and ability to function at work and home. This number is likely underreported.
How ADHD Shows Up
Without tools to cope with the impacts of ADHD, it can get overwhelming, and it may feel like the symptoms are getting harder to manage. The symptoms of ADHD can vary in each individual, but they aren’t all obstacles to life. Some symptoms of ADHD can enhance the lives of those diagnosed.
These symptoms are triggered by altered brain chemistry and neural activity:
- Lack of general focus
- Hyperfocused on details
- Poor impulse control or spontaneity
- Poor time management
- Inattention
- Increased empathy and exaggerated emotions
- Hyperactivity
- Executive dysfunction
There is no single test to determine if a person has ADHD. Additionally, there are three subtypes of ADHD. They are primarily hyperactive, primarily inattentive, or primarily combined types.
There are nine symptoms of ADHD that are primarily inattentive or primarily hyperactive. Adults must exhibit at least five of the symptoms in multiple settings to be diagnosed with ADHD.
How to Treat ADHD
The best treatments for ADHD are combinations of several approaches that work together. The ideal combination may be different for each individual.
They can include some or all of the following:
- Behavioral therapy
- Supplements
- Stress reduction
Adults with attention deficit hyperactivity disorder can develop strategies that help focus attention to successfully complete their activities at home and at work.
This is how Foss successfully completed nursing school and has thrived in her position in a fast-paced healthcare environment.
Seeking a Diagnosis
Foss was prompted to see her doctor after a classmate with many of the same challenges she had was diagnosed with ADHD. Finally having a diagnosis took a weight off her shoulders.
Foss has found that her symptoms can vary from day to day.
“Sometimes I can multitask like a pro; other times I constantly forget to bring a patient the warm blanket I promised them,” she says.
Self-acceptance and reparenting are two big ways to cope with the neurodivergence of ADHD while having compassion for its impacts. Foss recognizes that her brain is not as organized as her coworkers, and she has found approaches that help her work around the impacts of ADHD and successfully function as a nurse.
With medication, education, and established strategies, Foss stays organized by writing down everything. These strategies help her complete her tasks and pass important details to the next shift.
Foss has also identified certain benefits to her ADHD that help her at work. For example, she believes that she is more comfortable deviating from a set list of activities than some of her coworkers.
“I’m the one other nurses come to with the unusual questions about finding a workaround when we’re out of supplies,” she says.
Her management recognizes these qualities in Foss too. The education department specifically schedules Foss to cover other staff when three rounds of education are planned in a shift.
“I can go with the flow and rotate between three different assignments better than others can,” she says.
Finding what works for you is the first step in thriving as a nurse with ADHD. Seeking a community of people similarly impacted by ADHD can increase your sense of belonging, your support network, and your ability to meet your unique needs as a nurse or nursing student with ADHD.
Meet Our Contributor

Molly Foss, RN
Molly Foss is a registered nurse at a level 1 trauma center, but before that she was a mechanical drafter. After five years she realized that she wasn’t cut out to be sitting at a desk all day. At age 27, she went back to school to become a nurse. After two years, she was diagnosed with ADHD during her first year of nursing school. She has been a nurse for 11 years and has been in trauma and specialty care for the last eight.
You might be interested in

Time Management Tips for Nursing Students
Many nursing students have out-of-control schedules and a vanishing social life. These time management strategies can help you achieve your goals and still get some sleep.

Study Tips for Online Nursing Students
To help learners improve their study skills, we have gathered 10 tips for online success.

How to Manage Stress as a Nurse
Have you learned how to manage stress as a nurse? These 15 strategies can help reduce stress and protect your physical and mental health.

- Don’t leave your email app open as it is a huge distraction to hear that ‘incoming mail’ message. Make a rule that you only check your email at set times of day and only after your work is done.
- Use reminder alarms so you can “set it and forget it.” Knowing your alarm will go off when it’s time to leave to pick up the kids means your brain has a lot less “stuff” swirling around in it, making it much easier to focus on the task at hand.
- Slow down when taking tests and read things aloud if you can. This greatly minimizes the risk you’ll skip over potentially important words or phrases.
- When attending in-person lectures, sit in the front row so there are no distractions in front of you.
- If electronics are difficult distractions for you to resist, try taking notes on paper so you aren’t tempted to shop or do other things that pull you away from your work.
- Utilize earplugs or noise-canceling headphones during exams and work sessions if sounds are a source of distraction for you.
- Reward yourself for completing focus sessions. Maybe it’s making a cup of tea, playing with the dog or spending ten minutes doing an activity you enjoy. You’ve worked hard….you’ve earned it!
- Minimize visual distractions by keeping only the things you need to for that specific task/assignment on your desk. Put other books, notes or in-progress projects out of sight.
- If you tend to procrastinate with non-essential activities (especially when stressed), write a note to yourself and put it somewhere you can see it. Maybe it says, “I’ll organize my closet tomorrow. Today I’m studying for an exam.”
- If a thought or future task keeps popping into your head while you’re studying, jot it down on a dedicated list of things to tackle later. I call this my “Later List.”
Create an ADHD-friendly study space
Tackling nursing school with ADHD means setting up a workspace designed to maximize your success.
- Make sure you have everything you need at your desk area so you can get to work and minimize disruptions. This may include a water bottle, a snack, pens/pencils/highlighters, a comfortable chair, headphones, fidgets, reference books and study materials.
- Consider a computer riser so you can sit, stand, sit, stand, sit, stand, etc…
- Use a bookcase cabinet with doors versus open shelving so you can put things away when you’re not using them, leading to less distractions.
- Designate a study-only area in your home. This sends a message to your brain that when you’re in this space, it’s time to work.
- Some students benefit from alternate forms of seating and switch from a desk to a table to the couch to a lap desk, etc… Experiment to find what works for you!
Maximize your learning style
If you’re going to nursing school with ADHD, studying effectively means knowing and maximizing your learning style.
- Utilize interactive learning to stay as engaged as possible. A great resource for this is through the online access codes that come with textbooks. These often include many interactive activities that can help the student with ADHD stay engaged while learning and studying.
- Write your notes in different color pens or pencils. For visual and creative learners this can “trick” your brain into thinking it’s art and not just a bunch of words.
- Learn the material by teaching someone else. This is an excellent way to stay engaged and take on a very active role in your learning. Plus, it’s a great way to develop positive relationships in nursing school!
- Incorporate physical activity while reading. I’ve heard of students using fidget tools, incorporating color-coded highlighting and even knitting.
- Use a fidget tool to remind yourself to slow down during tests.
- If your brain is drawn to art and creativity, doing things like color-coding your notes, drawing out concepts, and even, using different handwriting styles can all engage your brain in an effective way.
- If you tend to zone out or lose interest during lecture, try to familiarize yourself with the concepts prior to class. One student reported that it was very helpful to do a quick skim of the reading and then try to fill out a LATTE template before class. Then, during lecture, she would stay engaged by filling in the gaps.
- If your school allows audio recordings of lecture, take advantage of this so you can listen to the lessons more than once. If you get bored with people who speak slowly, increase the playback speed.
- Utilize captions while watching videos. This gives your brain additional sensory input which can help you stay focused and engaged. You may need to request closed-captioning from your school or ask your professor to turn on captioning when using Zoom.
- Find what helps you remember things, even if it seems silly. Some students use goofy stories to remember medication side effects or disease signs/symptoms. Other effective techniques are mnemonic devices or even songs. Hey, whatever works!
- As you learn a concept, try to guess what the test questions will be about. Write these out as you go and not only have you stayed engaged, you’ve also created a study guide for the exam. That’s a win-win!
- Record yourself reading your notes or talking through concepts. Listen to these recordings as you do a physical activity such as walking to class or doing chores around the house.
- When reading out loud, try using an exaggerated voice. It sounds silly but it can help you stay engaged AND help you remember.
- Many students learn optimally by having the material read TO them. If you’re utilizing e-books, check to see if they have a “read aloud” option.
Apps and equipment
Having the tools you need to thrive can make going to nursing school with ADHD a lot less stressful. Note that some of these links earn this site a commission, these are always designated by #ad.
- Fidgets, like this Infinity Cube (#ad) , can help ease anxiety, focus your mind and serve as a reminder to stay engaged.
- iPad with Apple pencil and the Notability app. This app allows you to record lectures and take notes within the same document. This is a great way to review the material if you lost attention during class.
- Habitica – app that helps you form and follow habit routines with fun gamification built in.
- Freedom and Self Control – apps that block distracting apps and websites at times you designate.
- Focus Keeper – app that utilizes the Pomodoro technique.
- A white noise machine (#ad) can drown out unwanted sounds that cause distractions.
- Noise-canceling headphones(#ad) create a sound-free environment, or a superb auditory experience…you choose!
- An adjustable computer riser (#ad) enables you to transition from sitting to standing with ease.
Utilize your resources
If you’re heading into nursing school with ADHD, take the time to familiarize yourself with the resources available at your school.
- Utilize every resource that is available at your school. These include the disability center, writing center, tutoring services and counseling. Plan ahead because some of these may require appointments and documentation, especially when getting accommodations for things like exams.
- The “ How to ADHD ” YouTube channel has some wonderful suggestions and tools.
- If your school or division of Nursing has tutoring, make an appointment even if you don’t necessarily need the tutoring. Having structured study time is worth its weight in gold.
Be a clinical rockstar
Nursing school clinicals can be especially challenging for students with ADHD, but with these tips you will soar!
- In clinical, lists and routines will be your BFFs. Many students report having several things they need to do and then forgetting what they are by the time they get to the patient’s room. That’s because hospitals (and patients) are absolutely brimming with distractions. Make lists, even if it’s just a list of things to do next time you go in the patient’s room. Over time, you’ll probably find you rely on these lists less and less as the environment becomes more familiar.
- Routines help ensure you don’t forget to do important tasks. Develop a “start-of-shift” routine a “first-assessment” routine and an “end-of-shift” routine. I talk about all these routines in my book, Nursing School Thrive Guide (#ad).
- Use a run sheet. Run sheets are your general plan for the day, so you know when meds and specific interventions will be done. Download the Clinical Success Pack and get a run sheet you can use over and over again.
- Keep a small notepad (#ad) with you at all times. Jot down vital signs, patient requests, instructions from the RN and anything else you need to remember. There’s no shame in writing things down, especially when those tasks are new.
Stick with your medication regimen
- This is not the time to experiment with your medication regimen without your physician’s input. Up to 50% of college students under-use or stop using their ADHD medication. Always discuss your medication regimen with your healthcare provider.
- If you move away from home, have a plan for refills and regular check-ins with your doctor. This may include finding a new primary care provider, so plan ahead.
Be kind to yourself
Attending nursing school is rough enough, attending nursing school with ADHD can be especially challenging. You owe it to yourself to celebrate how amazing you are and to reward yourself for a job well done!
- More than anything else, it’s important that you give yourself some grace. Things that seem easy for other students may be challenging for you, but you actually have a lot of advantages. People with ADHD are creative problem solvers and that is HUGE in nursing…so give yourself a pat on the back!
- Exercise has been shown to be highly beneficial for students with ADHD, so make the time even if it’s just 30 minutes a day.
- Incorporate self care into your routine, and this includes down time to do things that simply bring you joy. Remember that replenishing your emotional reserves will actually make you MORE productive in the long run.
____________________________________________________________
The information, including but not limited to, audio, video, text, and graphics contained on this website are for educational purposes only. No content on this website is intended to guide nursing practice and does not supersede any individual healthcare provider’s scope of practice or any nursing school curriculum. Additionally, no content on this website is intended to be a substitute for professional medical advice, diagnosis or treatment.
20 Secrets of Successful Nursing Students
Being a successful nursing student is more than just study tips and test strategies. It’s a way of life.
you may also like...
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- Thieme Open Access

ADHD: Current Concepts and Treatments in Children and Adolescents
Renate drechsler.
1 Department of Child and Adolescent Psychiatry and Psychotherapy, University Hospital of Psychiatry, University of Zurich, Zurich, Switzerland
Silvia Brem
2 Neuroscience Center Zurich, Swiss Federal Institute of Technology and University of Zurich, Zurich, Switzerland
Daniel Brandeis
3 Department of Child and Adolescent Psychiatry and Psychotherapy, Central Institute of Mental Health, Medical Faculty Mannheim/Heidelberg University, Mannheim, Germany
4 Zurich Center for Integrative Human Physiology, University of Zurich, Zurich, Switzerland
Edna Grünblatt
Gregor berger, susanne walitza.
Attention deficit hyperactivity disorder (ADHD) is among the most frequent disorders within child and adolescent psychiatry, with a prevalence of over 5%. Nosological systems, such as the Diagnostic and Statistical Manual of Mental Disorders, 5th edition (DSM-5) and the International Classification of Diseases, editions 10 and 11 (ICD-10/11) continue to define ADHD according to behavioral criteria, based on observation and on informant reports. Despite an overwhelming body of research on ADHD over the last 10 to 20 years, valid neurobiological markers or other objective criteria that may lead to unequivocal diagnostic classification are still lacking. On the contrary, the concept of ADHD seems to have become broader and more heterogeneous. Thus, the diagnosis and treatment of ADHD are still challenging for clinicians, necessitating increased reliance on their expertise and experience. The first part of this review presents an overview of the current definitions of the disorder (DSM-5, ICD-10/11). Furthermore, it discusses more controversial aspects of the construct of ADHD, including the dimensional versus categorical approach, alternative ADHD constructs, and aspects pertaining to epidemiology and prevalence. The second part focuses on comorbidities, on the difficulty of distinguishing between “primary” and “secondary” ADHD for purposes of differential diagnosis, and on clinical diagnostic procedures. In the third and most prominent part, an overview of current neurobiological concepts of ADHD is given, including neuropsychological and neurophysiological researches and summaries of current neuroimaging and genetic studies. Finally, treatment options are reviewed, including a discussion of multimodal, pharmacological, and nonpharmacological interventions and their evidence base.
Introduction
With a prevalence of over 5%, attention deficit hyperactivity disorder (ADHD) is one of the most frequent disorders within child and adolescent psychiatry. Despite an overwhelming body of research, approximately 20,000 publications have been referenced in PubMed during the past 10 years, assessment and treatment continue to present a challenge for clinicians. ADHD is characterized by the heterogeneity of presentations, which may take opposite forms, by frequent and variable comorbidities and an overlap with other disorders, and by the context-dependency of symptoms, which may or may not become apparent during clinical examination. While the neurobiological and genetic underpinnings of the disorder are beyond dispute, biomarkers or other objective criteria, which could lead to an automatic algorithm for the reliable identification of ADHD in an individual within clinical practice, are still lacking. In contrast to what one might expect after years of intense research, ADHD criteria defined by nosological systems, such as the Diagnostic and Statistical Manual of Mental Disorders, 5th edition (DSM-5) and the International Classification of Diseases, editions 10 and 11 (ICD-10/11) have not become narrower and more specific. Rather, they have become broader, for example, encompassing wider age ranges, thus placing more emphasis on the specialist's expertise and experience. 1 2 3
Definitions and Phenomenology
Adhd according to the dsm-5 and icd-10/11.
ADHD is defined as a neurodevelopmental disorder. Its diagnostic classification is based on the observation of behavioral symptoms. ADHD according to the DSM-5 continues to be a diagnosis of exclusion and should not be diagnosed if the behavioral symptoms can be better explained by other mental disorders (e.g., psychotic disorder, mood or anxiety disorder, personality disorder, substance intoxication, or withdrawal). 1 However, comorbidity with other mental disorders is common.
In the DSM-5, the defining symptoms of ADHD are divided into symptoms of inattention (11 symptoms) and hyperactivity/impulsivity (9 symptoms). 1 The former differentiation between subtypes in the DSM-IV proved to be unstable and to depend on the situational context, on informants, or on maturation, and was therefore replaced by “presentations.” 4 Thus, the DSM-5 distinguishes between different presentations of ADHD: predominantly inattentive (6 or more out of 11 symptoms present), predominantly hyperactive/impulsive (6 or more out of 9 symptoms present), and combined presentation (both criteria fulfilled), as well as a partial remission category. Symptoms have to be present in two or more settings before the age of 12 years for at least 6 months and have to reduce or impair social, academic, or occupational functioning. In adolescents over 17 years and in adults, five symptoms per dimension need to be present for diagnosis. 1 In adults, the use of validated instruments like the Wender Utah rating scale is recommended. 5
In contrast, the ICD-10 classification distinguishes between hyperkinetic disorder of childhood (with at least six symptoms of inattention and six symptoms of hyperactivity/impulsivity, present before the age of 6 years) and hyperkinetic conduct disorder, a combination of ADHD symptoms and symptoms of oppositional defiant and conduct disorders (CD). 3 In the ICD-11 (online release from June 2018, printed release expected 2022), the latter category has been dropped, as has the precise age limit (“onset during the developmental period, typically early to mid-childhood”). Moreover, the ICD-11 distinguishes five ADHD subcategories, which match those of the DSM-5: ADHD combined presentation, ADHD predominantly inattentive presentation, ADHD predominantly hyperactive/impulsive presentation and two residual categories, ADHD other specified and ADHD nonspecified presentation. For diagnosis, behavioral symptoms need to be outside the limits of normal variation expected for the individual's age and level of intellectual functioning. 2
Overlapping Constructs: Sluggish Cognitive Tempo and Emotional Dysregulation
Sluggish cognitive tempo (SCT) is a clinical construct characterized by low energy, sleepiness, and absent-mindedness, and is estimated to occur in 39 to 59% of (adult) individuals with ADHD. 6 7 The question of whether SCT might constitute a feature of ADHD or a separate construct that overlaps with ADHD inattention symptoms is unresolved. 8 While current studies indicate that SCT might be distinct and independent from hyperactivity/impulsivity, as well as from inattention dimensions, it remains uncertain whether it should be considered as a separate disorder. 8 9 Twin studies have revealed a certain overlap between SCT and ADHD, especially with regard to inattention symptoms, but SCT seems to be more strongly related to nonshared environmental factors. 10
Emotion dysregulation is another associated feature that has been discussed as a possible core component of childhood ADHD, although it is not included in the DSM-5 criteria. Deficient emotion regulation is more typically part of the symptom definition of other psychopathological disorders, such as oppositional defiant disorder (ODD), CD, or disruptive mood dysregulation disorder (DSM-5; for children up to 8 years). 11 However, an estimated 50 to 75% of children with ADHD also present symptoms of emotion dysregulation, for example, anger, irritability, low tolerance for frustration, and outbursts, or sometimes express inappropriate positive emotions. The presence of these symptoms increases the risk for further comorbidities, such as ODD and also for anxiety disorders. 12 13 For adult ADHD, emotional irritability is a defining symptom according to the Wender Utah criteria, and has been confirmed as a primary ADHD symptom by several studies (e.g., Hirsch et al). 5 14 15
Whether emotion dysregulation is inherent to ADHD, applies to a subgroup with combined symptoms and a singular neurobiological pathway, or is comorbid with but independent of ADHD, is still a matter of debate (for a description of these three models; Shaw et al 13 ). Faraone et al 12 distinguished three ADHD prototypes with regard to deficient emotion regulation: ADHD prototype 1 with high-emotional impulsivity and deficient self-regulation, prototype 2 with low-emotional impulsivity and deficient self-regulation, and prototype 3 with high-emotional impulsivity and effective self-regulation. All three prototypes are characterized by an inappropriate intensity of emotional response. While prototypes 1 and 3 build up their responses very quickly, prototype 2 is slower to respond but experiences higher subjective emotional upheaval than is overtly shown in the behavior. Prototypes 1 and 2 both need more time to calm down compared with prototype 3 in which emotional self-regulation capacities are intact.
Dimensional versus Categorical Nature of ADHD
Recent research on subthreshold ADHD argues in favor of a dimensional rather than categorical understanding of the ADHD construct, as its core symptoms and comorbid features are dimensionally distributed in the population. 16 17 18 Subthreshold ADHD is common in the population, with an estimated prevalence of approximately 10%. 19 According to Biederman and colleagues, clinically referred children with subthreshold ADHD symptoms show a similar amount of functional deficits and comorbid symptoms to those with full ADHD, but tend to come from higher social-class families with fewer family conflicts, to have fewer perinatal complications, and to be older and female (for the latter two, a confound with DSM-IV criteria cannot be excluded). 20
Temperament and Personality Approaches to ADHD
Another approach which is in accordance with a dimensional concept is to analyze ADHD and categorize subtypes according to temperament/personality traits (for a review and the different concepts of temperament see Gomez and Corr 21 ). Temperament/personality traits are usually defined as neurobiologically based constitutional tendencies, which determine how the individual searches for or reacts to external stimulation and regulates emotion and activity. While temperament traits per se are not pathological, extreme variations or specific combinations of traits may lead to pathological behavior. This approach has been investigated in several studies by Martel and colleagues and Nigg, 22 23 24 who employed a temperament model comprising three empirically derived domains 25 26 : (1) negative affect, such as tendencies to react with anger, frustration, or fear; (2) positive affect or surgency which includes overall activity, expression of happiness, and interest in novelty; and (3) effortful control which is related to self-regulation and the control of action. The latter domain shows a strong overlap with the concept of executive function. 27 In a community sample, early temperamental traits, especially effortful control and activity level, were found to potentially predict later ADHD. 28 Karalunas et al 29 30 distinguished three temperament profiles in a sample of children with ADHD: one with normal emotional functioning; one with high surgency, characterized by high levels of positive approach-motivated behaviors and a high–activity level; and one with high negative (“irritable”) affect, with the latter showing the strongest, albeit only moderate stability over 2 years. Irritability was not reducible to comorbidity with ODD or CD and was interpreted as an ADHD subgroup characteristic with predictive validity for an unfavorable outcome. These ADHD temperament types were distinguished by resting-state and peripheral physiological characteristics as measured by functional magnetic resonance imaging (fMRI). 29
Epidemiology and Prevalence
While ADHD seems to be a phenomenon that is encountered worldwide, 31 prevalence rates and reported changes in prevalence are highly variable, depending on country and regions, method, and sample. 32 A meta-analysis by Polanczyk et al 32 yielded a worldwide prevalence rate of 5.8% in children and adolescents. 33 In an update published 6 years later, the authors did not find evidence for an increase in prevalence over a time span of 30 years. Other meta-analyses reported slightly higher (e.g., 7.2%) 34 or lower prevalence rates, which seems to be attributable to the different criteria adopted for defining ADHD. Prevalence rates in children and adolescents represent averaged values across the full age range, but peak prevalence may be much higher in certain age groups, for example, 13% in 9-year-old boys. 35 Universal ADHD prevalence in adults is estimated to lie at 2.8%, with higher rates in high-income (3.6%) than in low-income (1.4%) countries. 36 True prevalence rates (also called community prevalence, e.g., Sayal et al 37 ) should be based on population-based representative health surveys, that is, the actual base rate of ADHD in the population, in contrast to the administrative base rate, which is related to clinical data collection (Taylor 38 ). Recent reports on the increase in ADHD rates usually refer to administrative rates, drawn from health insurance companies, from the number of clinical referrals for ADHD, 39 clinical case identification estimates, or from the percentage of children taking stimulant medication (prescription data). Changes in these rates may be influenced by increased awareness, destigmatization, modifications in the defining criteria of ADHD, or altered medical practice. According to a recent U.S. health survey on children and adolescents (4–17 years), in which parents had to indicate whether their child had ever been diagnosed with ADHD, the percentage of diagnoses increased from 6.1% in 1997 to 10.2% in 2016. 40 A representative Danish survey based on health registry, data collected from 1995 to 2010 reported that ADHD incidence rates increased by a factor of approximately 12 (for individuals aged 4–65 years) during this period. Moreover, the gender ratio decreased from 7.5:1 to 3:1 at early school age and from 8.1:1 to 1.6:1 in adolescents in the same time frame, 41 42 probably indicating an improved awareness of ADHD symptoms in girls. In other countries, it is assumed that girls are still underdiagnosed. 38
Population register data show that the use of stimulants for ADHD has increased considerably worldwide. 43 In most countries, an increase in stimulant medication use has been observed in children since the 1990s (e.g., United Kingdom from 0.15% in 1992 to 5.1% in 2012/2013), 44 45 but in some European countries, stimulant prescription rates for children and adolescents have remained stable or decreased over the last 5 to 10 years (e.g., Germany). 35 In the United States, the prescription of methylphenidate peaked in 2012 and has since been slightly decreasing, while the use of amphetamines continues to rise. 46
Comorbidity, Differential Diagnosis, and Clinical Assessment
Comorbidity.
ADHD is characterized by frequent comorbidity and overlap with other neurodevelopmental and mental disorders of childhood and adolescence. The most frequent comorbidities are learning disorders (reading disorders: 15–50%, 4 dyscalculia: 5–30%, 47 autism spectrum disorder, which since the DSM-5 is no longer viewed as an exclusion criterion for ADHD diagnosis: 70–85%, 48 49 tic/Tourette's disorder and obsessive compulsive disorder: 20%, and 5%, 50 developmental coordination disorder: 30–50%, 51 depression and anxiety disorders: 0–45%, 52 53 and ODD and CD: 27–55% 54 ). ADHD increases the risk of substance misuse disorders 1.5-fold (2.4-fold for smoking) and problematic media use 9.3-fold in adolescence 55 56 and increases the risk of becoming obese 1.23-fold for adolescent girls. 57 58 59 It is also associated with different forms of dysregulated eating in children and adolescents. Enuresis occurs in approximately 17% of children with ADHD, 60 and sleep disorders in 25 to 70%. 61 Frequent neurological comorbidities of ADHD include migraine (about thrice more frequent in ADHD than in typically developing [TD] children) 62 63 64 and epilepsy (2.3 to thrice more frequent in ADHD than in TD children). 65 66 The risk of coexisting ADHD being seen as a comorbid condition and not the primary diagnosis is considerably enhanced in many childhood disorders of different origins. For example, the rate of comorbid ADHD is estimated at 15 to 40% 67 68 in children with reading disorders and at 26 to 41% 69 70 in children with mild intellectual dysfunction. While comorbidity in neurodevelopmental disorders may arise from a certain genetic overlap (see details under genetic associations), ADHD symptoms are also present in several disorders with well-known and circumscribed genetic defects, normally not related to ADHD (e.g., neurofibromatosis, Turner's syndrome, and Noonan's syndrome) 71 or disorders with nongenetic causes, such as traumatic brain injuries, pre-, peri- or postnatal stroke, or syndromes due to toxic agents, such as fetal alcohol syndrome. Comorbid ADHD is estimated in 20 to 50% of children with epilepsy, 72 73 in 43% of children with fetal alcohol syndrome, 74 and in 40% of children with neurofibromatosis I. 75 ADHD is three times more frequent in preterm-born children than in children born at term and four times more frequent in extremely preterm-born children. 76
Differential Diagnosis, Primary and Secondary ADHD
A range of medical and psychiatric conditions show symptoms that are also present in primary ADHD. The most important medical conditions which are known to “mimic” ADHD and need to be excluded during the diagnostic process are epilepsy (especially absence epilepsy and rolandic epilepsy), thyroid disorders, sleep disorder, drug interaction, anemia, and leukodystrophy. 77 78 The most important psychiatric conditions to be excluded are learning disorder, anxiety disorders, and affective disorders, while an adverse home environment also needs to be excluded.
However, the picture is complex, as many differential diagnoses may also occur as comorbidities. For instance, bipolar disorder, which is frequently diagnosed in children and adolescents in the United States but not in Europe, is considered as a differential diagnosis to ADHD, but ADHD has also been found to be a comorbidity of bipolar disorder in 21 to 98% of cases. 79 Similarly, absence epilepsy is a differential diagnosis of ADHD but is also considered to be a frequent comorbidity, occurring in 30 to 60% of children with absence epilepsy. 80 The prevalence of the ADHD phenotype in benign childhood epilepsy with centrotemporal spikes (rolandic epilepsy) lies at 64 to 65%, 81 and is possibly related to the occurrence of febrile convulsions. 82 The literature often does not draw a clear distinction between an ADHD phenotype, which includes all types of etiologies and causes, and a yet to be specified developmental ADHD “genotype.” Some authors use terms, such as “idiopathic” ADHD, 83 “primary,” or “genotypic” ADHD, 84 in contrast to ADHD of circumscribed origin other than developmental, the latter being referred to as ADHD “phenotype,” or “phenocopy,” 85 or “ADHD-like.” 86 “Secondary ADHD” usually refers to newly acquired ADHD symptoms arising after a known event or incident, for example, a head trauma or stroke. After early childhood stroke, the ADHD phenotype occurs in 13 to 20% of cases, and after pediatric traumatic brain injury, ADHD symptoms are observed in 15 to 20% of children. 87 Having ADHD considerably increases the risk of suffering a traumatic brain injury, 88 89 90 and most studies on secondary ADHD after traumatic brain injury control for or compare with premorbid ADHD (e.g., Ornstein et al 91 ). Whether and to what extent “phenotypic” and “genotypic” ADHD need to be distinguished on a phenomenological level is not clear. It is possible that shared neurobiological mechanisms will prevail and that genetic vulnerability and epigenetic factors may play a role in both types. For example, James et al 86 compared neurophysiological markers in two groups of adolescents with ADHD, one born very preterm and the other born at term. While the authors found very similar ADHD-specific markers in the two groups, some additional deficits only emerged in the preterm group, indicating more severe impairment. Other examples are rare genetic diseases with known genetic defects, which are often comorbid with ADHD. One may ask whether, for example, ADHD in Turner's syndrome should be considered as a rare genetic ADHD variant and count as genotypic ADHD, or whether it results from a different genetic etiology, with the status of an ADHD phenotype.
Clinical Diagnostic Procedure
Clinical assessment in children should mainly be based on a clinical interview with parents, including an exploration of the problems, the detailed developmental history of the child including medical or psychiatric antecedents, information on family functioning, peer relationships, and school history. According to the guidelines of the National Institute for Health and Care Excellence (NICE) in the United Kingdom, this may also include information on the mental health of the parents and the family's economic situation. The child's mental state should be assessed, possibly using a standardized semistructured clinical interview containing ADHD assessments (e.g., Kiddie Schedule for Affective Disorders and Schizophrenia Present and Lifetime version, DSM-5) 92 93 and by observer reports. The exploration should cover behavioral difficulties and strengths in several life contexts, for example, school, peer relationships, and leisure time. The use of informant rating scales, such as Conners' Rating Scales, 3rd edition, 94 or the Strengths and Difficulties Questionnaire 95 may be useful, but diagnosis should not be solely based on rating scales (NICE, AWFM ADHD). 96 97 A further interview should be conducted with the child or adolescent to gain a picture of the patient's perspective on current problems, needs, and goals, even though self-reports are considered less reliable for diagnosis. Information should also be obtained from the school, for example, by face-to-face or telephone contact with the teacher and, if possible, by direct school-based observation. A medical examination should be performed to exclude somatic causes for the behavioral symptoms and to gain an impression of the general physical condition of the patient. Current guidelines do not recommend including objective test procedures (intelligence and neuropsychological tests), neuroimaging, or neurophysiological measures in routine ADHD assessment but do suggest their use as additional tools when questions about cognitive functions, academic problems, coexisting abnormalities in electroencephalography (EEG), or unrecognized neurological conditions arise. After completion of the information gathering, the NICE guidelines recommend a period of “watchful waiting” for up to 10 weeks before delivering a formal diagnosis of ADHD. A younger age of the diagnosed child relative to his/her classmates has to be mentioned as one of the many pitfalls in the assessment of ADHD. It has been shown that the youngest children in a class have the highest probability of being diagnosed with ADHD and of being medicated with stimulants. 98
There is consensus that the diagnosis of ADHD requires a specialist, that is, a child psychiatrist, a pediatrician, or other appropriately qualified health care professionals with training and expertise in diagnosing ADHD. 97
Current Neurobiological and Neuropsychological Concepts
Neuropsychology, neuropsychological pathways and subgroups.
ADHD is related to multiple underlying neurobiological pathways and heterogeneous neuropsychological (NP) profiles. Twenty-five years ago, ADHD was characterized as a disorder of inhibitory self-control, 54 and an early dual pathway model distinguished between an inhibitory/executive function pathway and a motivational/delay aversion pathway (also called “cool” and “hot” executive function pathways in later publications), which are related to distinct neurobiological networks. 99 100 101 Still, the two systems may also interact. 102
Since then, other pathways have been added, such as time processing, 103 but a definitive number of possible pathways is difficult to define. For example, Coghill and colleagues 104 differentiated six cognitive factors in children with ADHD (working memory, inhibition, delay aversion, decision-making, timing, and response time variability) derived from seven subtests of the Cambridge neuropsychological test automated battery. Attempts to empirically classify patients into subgroups with selective performance profiles departing from comprehensive NP data collection were inconclusive. For example, using delay aversion, working memory, and response-time tasks, Lambek and colleagues 105 expected to differentiate corresponding performance profile subgroups in children with ADHD. However, their analysis resulted in subgroups differentiated by the severity of impairments, and not by selective profiles. Other empirical studies using latent profile or cluster analysis of NP tasks in large ADHD samples have differentiated three 106 107 or four 108 NP profile groups, which all included children with ADHD, as well as TD children, differing in severity but not in the type of profile. This might indicate that the identified NP deficit profiles were not ADHD-specific, but rather reflected characteristic distributions of NP performances, which are also present in the general population, with extreme values in children with ADHD. Some other empirical studies in the search for subgroups, however, identified ADHD-specific performance profiles (“poor cognitive control,” 109 “with attentional lapses and fast processing speed” 110 ), among other profiles being shared with TD controls. Obviously, divergent results regarding subgrouping may also be related to differing compilations of tested domains, consequently leading to a limited comparability of these studies.
Which Neuropsychological Functions are Impaired in ADHD and When?
A meta-analysis conducted in 2005 identified consistent executive function deficits with moderate effect sizes in children with ADHD in terms of response inhibition, vigilance, working memory, and planning. 67 Since then, a vast number of studies on NP deficits in children with ADHD compared with TD controls have been published. A recent meta-analysis included 34 meta-analyses on neurocognitive profiles in ADHD (all ages) published until 2016, referring to 12 neurocognitive domains. 111 The authors found that 96% of all standardized mean differences were positive in favor of the control group. Unweighted effect sizes ranged from 0.35 (set shifting) to 0.66 (reaction time variability). Weighted mean effect sizes above 0.50 were found for working memory (0.54), reaction time variability (0.53), response inhibition (0.52), intelligence/achievement (0.51), and planning/organization (0.51). Effects were larger in children and adolescents than in adults. The other domains comprised vigilance, set shifting, selective attention, reaction time, fluency, decision making, and memory.
Nearly every neuropsychological domain has been found to be significantly impaired in ADHD compared with TD controls, though effect sizes are often small. This includes, for example, altered perception (e.g., increased odor sensitivity 112 ; altered sensory profile 113 ; impaired yellow/blue color perception, e.g., Banaschewski et al, 114 for review, see Fuermaier et al 115 ), emotional tasks (e.g., facial affect discrimination), 116 social tasks (e.g., Marton et al 117 ), communication, 118 and memory. 119 Several of the described impairments may be related to deficient top-down cognitive control and strategic deficits, 120 121 122 but there is also evidence for basic processing deficits. 123
Neuropsychological Deficits as Mediators of Gene-Behavior Relations
A vast amount of research has been devoted to the search for neuropsychological endophenotypes (or intermediate phenotypes) for ADHD, that is, neurobiologically based impairments of NP performance characteristic of the disorder that may also be found in nonaffected close relatives. ADHD neuropsychological endophenotypes are assumed to mediate genetic risk from common genetic variants. 124 So far, deficits in working memory, reaction-time variability, inhibition, time processing, response preparation, arousal regulation, and others have been identified as probable endophenotypes for ADHD. 124 125 126 127 Genetic studies indicate an association of an ADHD-specific polygenetic general risk score (i.e., the total number of genetic variants that may be associated with ADHD, mostly related to dopaminergic transmission) with working memory deficits and arousal/alertness, 124 or with a lower intelligence quotient (IQ) and working memory deficits, 128 respectively. More specifically, a link of ADHD-specific variants of DAT1 genes with inattention and hyperactivity symptoms seems to be mediated by inhibitory control deficits. 129
Individual Cognitive Profiles and the Relevance of Cognitive Testing for the Clinical Assessment
Heterogeneity is found with regard to profiles, as well as with regard to the severity of cognitive impairment in individuals with ADHD, as measured by standardized tests. ADHD does not necessarily come with impaired neuropsychological test performance: about one-third of children with ADHD will not present any clinically relevant impairment, while another one-third shows unstable or partial clinical impairment, and about another one-third performs below average in NP tests. The classic concept of NP impairment, which assumes relative stability over time, possibly does not apply to NP deficits observed in ADHD, or only to a lesser extent. For the larger part, the manifestation of performance deficits may depend on contextual factors, 130 such as reward, or specifically its timing, amount, and nature, or on energetic factors, 131 for example, the rate of stimulus presentation or the activation provided by the task.
Many studies have shown that behavioral ratings of ADHD symptoms or questionnaires on executive function deficits are not, or at best weakly, correlated with NP test performance, even when both target the same NP domain. 132 133 In consequence, questionnaires on executive functioning are not an appropriate replacement for neuropsychological testing. Likewise, ADHD symptom rating scales do not predict results of objective attention or executive function tests and vice versa. Although mild intellectual disability and low IQ are more typically associated with the disorder, ADHD can be encountered across the entire IQ spectrum, including highly gifted children. 134 Therefore, an intelligence test should be part of the diagnostic procedure, but is not mandatory according to ADHD guidelines. In some children, intellectual difficulties and not ADHD may be the underlying cause for ADHD-like behaviors, while in other children with ADHD, academic underachievement despite a high IQ may be present.
It has been argued that symptoms defining ADHD may be understood as dimensional markers of several disorders belonging to an ADHD spectrum and, in consequence, the diagnosis of these behavioral symptoms should be the starting point for a more in-depth diagnosis rather than the endpoint. 135 This should include the cognitive performance profile. The ADHD behavioral phenotype predicts neither NP impairment nor intellectual achievement in the individual case, and objective testing is the only way to obtain an accurate picture of the child's cognitive performance under standardized conditions. Its goal is not ADHD classification, but rather to obtain the best possible understanding of the relation between cognitive functioning and behavioral symptoms for a given patient, to establish an individually tailored treatment plan.
Neurophysiology
Neurophysiological methods like EEG, magnetoencephalography, and event-related potentials (ERPs) as task-locked EEG averages capture brain functions in ADHD at high (ms) temporal resolution. The approach covers both fast and slow neural processes and oscillations, and clarifies the type and timing of brain activity altered in ADHD at rest and in tasks. It reveals neural precursors, as well as correlates, and consequences of ADHD behavior. 136 Neurophysiological and particularly EEG measures also have a long and controversial history as potential biomarkers of ADHD. Current evidence clarifies how multiple pathways and deficits are involved in ADHD at the group level, but recent attempts toward individual clinical translation have also revealed considerable heterogeneity, which does not yet support a clinical application for diagnostic uses or treatment personalization, as explained below.
Resting Electroencephalography
The EEG is dominated by oscillations in frequency bands ranging from slow δ (<4 Hz) and θ (4–7 Hz) via α (8–12 Hz) to faster β (13–30 Hz) and γ (30–100 Hz) band activity. The spectral profile reflects maturation and arousal, with slow frequencies dominating during early childhood and slow-wave sleep. Source models can link scalp topography to brain sources and distributed networks.
Initial studies suggested a robust link between ADHD diagnosis and resting EEG markers of reduced attention, hypoarousal, or immaturity, such as increased θ and an increased θ/β ratio (TBR). However, more recent studies, 137 138 some with large samples, 139 140 failed to replicate a consistent TBR increase in ADHD. Instead, the results indicated heterogeneous θ and β power deviations in ADHD not explained by ADHD subtype and psychiatric comorbidity. 141 A cluster analysis of EEG in children with ADHD also revealed considerable heterogeneity regarding θ excess and β attenuation in ADHD. While several clusters with EEG patterns linked to underarousal and immaturity could be identified, only three of the five EEG clusters (60% of the cases with ADHD) had increased θ. 139 Several recent θ and TBR studies that no longer found TBR association with ADHD diagnosis still replicated the reliable age effects, 137 138 142 confirming the high quality of these studies. Increasing sleepiness in adolescents, 143 or shorter EEG recordings, may have reduced the sensitivity to time effects and state regulation deficits in ADHD, 136 144 potentially contributing to these replication failures. Also, conceptualizing TBR as a marker of inattention or maturational lag may be too simple, since θ activity can also reflect concentration, cognitive effort, and activation. 145 146
During sleep, stage profiles reveal no consistent deviations in ADHD, but the slow-wave sleep topography is altered. In particular, frontal slow waves are reduced, leading to a more posterior topography as observed also in younger children. 147 This delayed frontalization can be interpreted as a maturational delay in ADHD, in line with a cluster of resting EEG, changes in task related ERPs during response inhibition, 148 and structural magnetic resonance imaging (MRI) findings. 149
Task Related Event-Related Potentials
Task-related processing measures, particularly ERPs, have critically advanced our understanding of ADHD through their high-time resolution, which can separate intact and compromised brain functions. ERPs have revealed impairments during preparation, attention, inhibition, action control, as well as error, and reward processing, with partly distinct networks but often present during different phases of the same task. In youth and adults with ADHD, the attentional and inhibitory P3 components and the preparatory contingent negative variation (CNV) component are most consistently affected, but state regulation and error or reward processing are also compromised. 136 150 Activity during preparation, attention, or inhibition is typically weaker and more variable but not delayed. This often occurs in task phases without visible behavior and precedes the compromised performance. Familial and genetic factors also modulate these markers of attention and control. Some impairment is also observed in nonaffected siblings or in parents without ADHD, 151 152 and genetic correlates often implicate the dopamine system. 125 Some ERP changes, like the attenuated CNV during preparation, remain stable throughout maturation, and are also markers of persistent ADHD, while other markers, such as the inhibition related P3, remain attenuated despite clinical remission. 148 153
Overall, the ERP results confirm attentional, cognitive, and motivational, rather than sensory or motor impairments in ADHD, in line with current psychological and neurobiological models. However, different ERP studies hardly used the same tests and measures, so valid statements regarding classification accuracy and effect size are particularly difficult, 154 and there is an urgent need for meta-analyses regarding the different ERPs.
Clinical Translation
Despite published failures to replicate robust TBR based classification of ADHD, a TBR-based EEG test was recently approved by the U.S. Food and Drug Administration to assist ADHD diagnosis. 155 Although not promoted as a stand-alone test, children with suspected ADHD, and increased TBR were claimed to likely meet full diagnostic criteria for ADHD; while children with suspected ADHD but no TBR increase should undergo further testing, as they were likely to have other disorders better explaining ADHD symptoms (see also DSM-5 exclusionary criterion E).
This multistage diagnostic approach could possibly identify a homogeneous neurophysiological subgroup, but it omits critical elements of careful, guideline-based ADHD diagnostics. Reliability and predictive value of the TBR remain untested, and the increasing evidence for poor validity of TBR renders it unsuitable for stand-alone ADHD diagnosis. Accordingly, the use of TBR as a diagnostic aid was broadly criticized. 156 157
In sum, the recent literature suggests that neither TBR nor other single EEG or ERP markers are sufficient to diagnose ADHD and are not recommended for clinical routine use, in line with the increasing evidence for heterogeneity in ADHD.
Combining measures across time, frequency, and tasks or states into multivariate patterns may better characterize ADHD. The potential of such approaches is evident in improved classification using machine-learning algorithms based on combinations of EEG measures 142 or EEG and ERP measures. 138 158 However, claims of high-classification accuracies up to 95% (e.g., Mueller et al 158 ) require further independent replication and validation with larger samples, and plausible mapping to neural systems and mechanisms. Modern pattern classification is particularly sensitive to uncontrolled sample characteristics and needs validation through independent large samples. 159
Focusing on EEG-based prediction rather than diagnosis may hold more promise for clinical translation, and may utilize the EEG heterogeneity in clinical ADHD samples. For example, early studies on predicting stimulant response suggested that children with altered wave activity, in particular increased TBR, θ or α slowing, respond well to stimulant medication. However, in recent prospective work with a large sample, TBR was not predictive, and α slowing allowed only limited prediction in a male adolescent subgroup. 160
Predicting response to intense nonpharmacological treatment is of particular interest given the high costs and time requirements. Promising findings have been reported for one neurofeedback study, where α EEG activity and stronger CNV activity together predicted nearly 30% of the treatment response. 161 Still, the lack of independent validation currently allows no clinical application.
In conclusion, neurophysiological measures have clarified a rich set of distinct impairments but also preserved functions which can also serve as markers of persistence or risk. These markers may also contribute in the classification of psychiatric disorders based on neuromarkers (research domain criteria approach). As potential predictors of treatment outcome they may support precision medicine, and proof-of-concept studies also highlight the potential of multivariate profiling. The findings also demonstrate the challenge with this approach, including notable replication failures, and generalizability of most findings remains to be tested. Neurophysiological markers are not ready to serve as tools or aids to reliably diagnose ADHD, or to personalize ADHD treatment in individual patients.
Neuroimaging
Modern brain imaging techniques have critically contributed to elucidating the etiology of ADHD. While MRI provides detailed insights into the brain microstructure, such as for example gray matter volume, density, cortical thickness, or white matter integrity, fMRI allows insights into brain functions through activation and connectivity measures with high–spatial resolution.
Delayed Maturation and Persistent Alterations in the Brain Microstructure in ADHD
The brain undergoes pronounced developmental alterations in childhood and adolescence. Gray matter volume and cortical thickness show nonlinear inverted U -shaped trajectories of maturation with a prepubertal increase followed by a subsequent decrease until adulthood while white matter volume progressively increases throughout adolescence and early adulthood in a rather linear way. 162 163 164 165 Large variations of the maturational curves in different brain regions and subregions suggest that phylogenetically older cortical areas mature earlier than the newer cortical regions. Moreover, brain areas associated with more basic motor or sensory functions mature earlier than areas associated with more complex functions including cognitive control or attention. 163 164 Altered maturation of the cortex for ADHD has been reported for multiple areas and cortical dimensions, 166 167 mainly in the form of delayed developmental trajectories in ADHD but recently also as persistent reductions, particularly in the frontal cortex. 168 Such findings speak for delayed maturation in specific areas rather than a global developmental delay of cortical maturation in ADHD. Microstructural alterations in ADHD have been associated with a decreased intracranial volume 169 and total brain size reduction of around 3 to 5%. 100 168 170 In accordance, increasing ADHD symptoms in the general population correlated negatively with the total brain size. 171 A meta-analysis (Frodl et al) and a recent cross-sectional mega- and meta-analysis (Hoogman et al) indicate that such reductions in brain volume may be due to decreased gray matter volumes in several subcortical structures, such as the accumbens, amygdala, caudate, hippocampus, and putamen but also cortical areas (prefrontal, the parietotemporal cortex) and the cerebellum. 170 172 173 174 175 176 177 Effects sizes of subcortical alterations were highest in children with ADHD and the subcortical structures showed a delayed maturation. 169 Moreover, higher levels of hyperactivity/impulsivity in children were associated with a slower rate of cortical thinning in prefrontal and cingulate regions. 167 178 Differences in brain microstructure have also been reported in a meta-analysis for white matter integrity as measured with diffusion tensor imaging in tracts subserving the frontostriatal-cerebellar circuits. 179 To summarize, diverse neuroanatomical alterations in total brain volume and multiple cortical and subcortical dimensions characterize ADHD. These alterations are most pronounced in childhood and suggest a delayed maturation of specific cortical and subcortical areas along with some persistent reductions in frontal areas in a subgroup of ADHD patients with enduring symptoms into adulthood.
Alterations in the Brain Function of Specific Networks in ADHD
Specific functional networks, mainly those involved in inhibition, attention processes, cognitive control, reward processing, working memory, or during rest have been intensively studied in ADHD using fMRI in the past. Alterations have been reported in the corresponding brain networks and the main findings are summarized below.
Atypical Resting State Connectivity in Children with ADHD
Resting state examines spontaneous, low frequency fluctuations in the fMRI signal during rest, that is , in absence of any explicit task. 180 Resting state networks describe multiple brain regions for which the fMRI signal is correlated (functionally connected) at rest, but the same networks may coactivate also during task-based fMRI. 181 One important resting state network, the so-called default mode network (DMN), comprises brain areas that show higher activation during wakeful rest and deactivations with increasing attentional demands. 182 183 While the DMN usually shows decreasing activation with increasing attentional demands, the cognitive control network shows an opposite pattern and increases its activation. This inverse correlation of DMN and the cognitive control networks is diminished or absent in children and adults with ADHD and may explain impaired sustained attention through attentional lapses that are mediated by the DMN. 181 184 185 186 In addition, a more diffuse pattern of resting state networks connectivity and a delayed functional network development in children with ADHD have been reported. 187 Finally, atypical connectivity in cognitive and limbic cortico-striato-thalamo-cortical loops of patients with ADHD suggest that the neural substrates may either reside in impaired cognitive network and/or affective, motivational systems. 181
Altered Processing of Attention and Inhibition in Fronto-basal Ganglia Circuits in ADHD
Meta-analyses summarizing the findings of functional activation studies report most consistent alterations in brain activation patterns as hypoactivation of the frontoparietal network for executive functions and the ventral attention system for attentional processes in children with ADHD. 188 189 190 More specifically, motor or interference inhibition tasks yielded consistent decreases in a (right lateralized) fronto-basal ganglia network comprising supplementary motor area, anterior cingulate gyrus, left putamen, and right caudate in children with ADHD. 189 190 For tasks targeting attentional processes, decreased activation in a mainly right lateralized dorsolateral fronto-basal ganglia-thalamoparietal network characterized children with ADHD. Depending on the task, hyperactivation can cooccur in partly or distinct cerebellar, cortical, and subcortical regions. 188 189 190
Altered Reward Processing and Motivation
Emotion regulation and motivation is mediated by extended orbitomedial and ventromedial frontolimbic networks in the brain. 191 Abnormal sensitivity to reward seems to be an important factor in the etiology of ADHD as suggested by several models of ADHD, 192 193 194 mainly due to a hypofunctioning dopaminergic system. 195 In accordance, impairments in specific signals that indicate violations of expectations, the so called reward prediction errors (RPE), were shown in the medial prefrontal cortex of adolescents with ADHD during a learning task. 196 RPE signals are known to be encoded by the dopaminergic system of the brain, and deficient learning and decision making in ADHD may thus be a consequence of impaired RPE processing. 196 Abnormal activation has also been reported for the ventral striatum during reward anticipation and in other cortical and subcortical structures of the reward circuitry. 197
Normalization of Atypical Activation and Brain Structural Measures after Treatment
Stimulant medication and neurofeedback studies have pointed to a certain normalization of dysfunctional activation patterns in critical dorsolateral frontostriatal and orbitofrontostriatal regions along with improvements in ADHD symptoms. 198 199 200 201 Also, brain microstructure, especially the right caudate, has shown some gradual normalization with long-term stimulant treatment. 176 190
To conclude, a wide range of neuroimaging studies reveal relatively consistent functional deficits in ADHD during executive functions, including inhibitory control, working memory, reward processes, and attention regulation but also during rest. Some of these alterations are more persistent, others are specific to children and may thus represent a developmental delay. Specific treatments showed trends toward a normalization of alterations in brain microstructure and functional networks.
Genetic Associations with ADHD and ADHD Related Traits
From family studies, as well as twin studies, the heritability for ADHD has been estimated to be between 75 upto 90%. 202 Moreover, the heritability was found to be similar in males and females and for inattentive and hyperactive-impulsive components of ADHD. 202 Interestingly, a strong genetic component was also found when the extreme and subthreshold continuous ADHD trait symptoms were assessed in the Swedish twins. 19 Even over the lifespan, adult ADHD was found to demonstrate high heritability that was not affected by shared environmental effects. 203 Recently, structural and functional brain connectivity assessed in families affected by ADHD has been shown to have heritable components associated with ADHD. 204 Similarly, the heritability of ERPs elicited in a Go/No-Go-task measuring response inhibition known to be altered in ADHD, was found to be significantly heritable. 205
In several studies, ADHD-related traits have also shown significant heritability. For example, in two independent, population based studies, significant single nucleotide polymorphism heritability estimates were found for attention-deficit hyperactivity symptoms, externalizing problems, and total problems. 206 In another study, investigating the two opposite ends of ADHD symptoms, low-extreme ADHD traits were significantly associated with shared environmental factors without significant heritability. 207 While on the other hand, high-extreme ADHD traits showed significant heritability without shared environmental influences. 207 A crossdisorder study including 25 brain disorders from genome wide association studies (GWAS) of 265,218 patients and 784,643 controls, including their relationship to 17 phenotypes from 1,191,588 individuals, could demonstrate significant shared heritability. 208 In particular, ADHD shared common risk variants with bipolar disorder, major depressive disorder, schizophrenia, and with migraine. 208 Indeed, in general, population-based twin studies suggest that genetic factors are associated with related-population traits for several psychiatric disorders including ADHD. 209 This suggests that many psychiatric disorders are likely to be a continuous rather than a categorical phenotype.
Though ADHD was found to be highly heritable, the underlying genetic risk factors are still not fully revealed. The current consensus suggests, as in many other psychiatric disorders, a multifactorial polygenic nature of the common disorder. Both common genetic variants studied by hypothesis-driven candidate gene association or by the hypothesis-free GWAS could only reveal the tip of the iceberg. Through the candidate gene approach, only very few findings could show replicable significant association with ADHD, as reported by meta-analysis studies for the dopaminergic, noradrenergic, and serotonergic genes. 210 211 Several GWAS have been conducted followed by meta-analysis, which again failed reaching genome-wide significant results. 212 213 214 215 216 217 218 219 220 221 222 223 224 However, recently, the first genome-wide significance has been reached in a GWAS meta-analysis consisting of over 20,000 ADHD patients and 35,000 controls. 225 Twelve independent loci were found to significantly associate with ADHD, including genes involved in neurodevelopmental processes, such as FOX2 and DUSP6 . 225 But even in these findings the effect sizes are rather small to be used for diagnostic tools. Therefore, polygenic risk score approaches have emerged as a possible tool to predict ADHD. 202 Yet this approach needs further investigation now that genome-wide significance has been reached by Demontis et al. 225 However, at this point, it is not yet possible to exclude that rare SNPs of strong effect may also be responsible (similar to breast cancer) for a small proportion of ADHD cases due to the heterogeneity of symptomatology, illness course, as well as biological marker distribution, as outlined above.
Multimodal Treatment of ADHD
A variety of national and international guidelines on the assessment and management of ADHD have been published over the last 10 years, not only for clinicians but also for patients and caregivers. 96 97 226 227 228 All guidelines recommend a multimodal treatment approach in which psychoeducation forms a cornerstone of the treatment and should be offered to all of those receiving an ADHD diagnosis, as well as to their families and caregivers.
According to the NICE Guidelines, the first step is always a planning process for the multimodal treatment with respect to the psychological, behavioral, and occupational or educational needs of the child and his/her family. 97 This planning phase could be organized as a “round table” with the child, parents, and other caregivers. The following aspects should be taken into account: the severity of ADHD symptoms and impairment, the relative impact of other neurodevelopmental or mental health conditions and how these affect or may affect everyday life (including sleep). In addition, resilience and protective factors, as well as the goals of the child and family, should be considered in the intervention process. The participation of child and parents in the planning and treatment process is more centrally outlined in recent guidelines and is emphasized in detail for the different treatment steps (e.g., NICE and S3 Guidelines). 96 97 The participation process is not just a one-time dialogue but should rather continue throughout all steps of the treatment process. Benefits and harms of nonpharmacological and pharmacological treatments should be discussed carefully and on the basis of the latest evidence. Preferences and concerns, and the importance of adherence to treatment, should be discussed and taken into account within the treatment process. Patients and their families or caregivers should be reassured, as appropriate that they can revisit decisions about treatments.
Multimodal treatment approaches also advocate a systematic adaptive procedure that combines different treatment modules according to the needs and situation of the patient and family. This may, for instance, include a first stage in which parent counseling is initiated, a second-stage encompassing, for example, individual behavioral therapy for the child, while the parents participate in a parent training program in parallel, followed by a third stage in which stimulant medication is started, etc. 229 230 Environment-centered interventions aim at the counseling or training of parents or the instruction of teachers at school or preschool. Parent training programs may be administered individually or in groups and have shown positive effects on parenting skills, ADHD behavior, and comorbid conduct problems. 231 232 233 Family therapy for ADHD focuses on the ADHD family, with the ADHD patient being a part of the family system with dysfunctional interactional patterns. 234 School-based interventions may target (1) the conditions in the classroom, for example, by minimizing distractions; (2) the instruction of the teacher, for example, by suggesting more appropriate teaching methods or by promoting peer tutoring; or (3) the student, for example, by improving self-management and social skills, or by helping to cope with stigma. 235 236 237
Pharmacological Approaches
Starting medication.
All medication for ADHD should only be initiated by a health care professional with training and expertise in diagnosing and managing ADHD. The expert should be familiar with the pharmacokinetic profiles and bioavailability of all the short- and long-acting preparations available for ADHD. The following parameters should be considered before first medication: medical history of the child but possibly also of the parents, current medication, height and weight, baseline pulse and blood pressure, a cardiovascular assessment, and an electrocardiogram if the treatment may affect the QT interval. A cardiology expert opinion should be sought before starting medication for ADHD if there is a history of congenital heart disease, previous cardiac surgery, or a history of sudden death in a first-degree relative under the age of 40 years, or if the blood pressure is consistently above the 95th centile for age and height for children and young people.
Age-Specific Needs
Treatment recommendations are often based on the specific needs of children, youth, or adults. 97 226 According to the NICE guidelines 97 and also pharmacological recommendations (e.g., Walitza and colleagues 238 239 ), a distinction should also be made between children under 5 years of age or preschool children, and school children. For the younger children (under 5 years of age), parent or career training programs and parent group training programs are always first-line treatments. Medication for children under 5 years with ADHD should only be given following a second specialist opinion from an ADHD service with expertise in managing ADHD in young children (ideally from a tertiary service). For children over 5 years of age, education and information about the causes and impact of ADHD and advice on parenting strategies should be offered, as well as liaison with school, college, or university if consent to do so is provided. 97 Children aged 5 years and over and young people should only receive medication if the ADHD symptoms are still causing a persistent significant impairment in at least one life domain after environmental modifications have been implemented and evaluated.
Selection of Pharmacotherapy
In Europe, methylphenidate either as short- or long-acting preparation is the first-line medication for ADHD across the life span. Second-line medications are lisdexamfetamine, atomoxetine, and guanfacine. A switch to lisdexamfetamine is only recommended if children have first undergone at least a 6-week trial of methylphenidate at an adequate dose and have not derived sufficient benefit in terms of reduced ADHD symptoms and associated impairment, or if patients experience adverse side effects. 238 The Canadian Guidelines (2018) recommend an individual treatment approach, which can start with different options, and if medication is to be used, long-acting formulations of psychostimulants or atomoxetine are always the first choice. 226 Comorbid disorders may necessitate adjustments to the treatment plan or alternative treatments.
According to the NICE guidelines, atomoxetine and guanfacine should only be offered if patients cannot tolerate methylphenidate or lisdexamfetamine or if their symptoms have not responded to separate 6-week trials of methylphenidate and lisdexamfetamine, having considered alternative preparations and adequate doses. 97
Evidence for ADHD Medications
In the first “gold standard” study comparing the different treatment approaches for ADHD alone and in combination (National Institute of Mental Health Collaborative Multimodal Treatment Study of Children with ADHD [MTA study]), the effects of both pharmacological therapy (methylphenidate and intensive counseling) and of multimodal therapy (methylphenidate and intensive behavioral therapy) were significantly more effective after 14 months than behavioral therapy alone or than the “standard” therapy (treatment as usual in the community) of the control group. The multimodal therapy was not significantly superior to pharmacological therapy alone, but did result in significant improvements in ADHD symptoms at a lower dosage of methylphenidate. 240 241 242 Since the MTA study, numerous studies have investigated methylphenidate, amphetamine, and nonstimulants like atomoxetine or α 2 -adrenoceptor agonists, such as clonidine and guanfacine, regarding different aspects of effectiveness and tolerability.
The psychostimulants methylphenidate and amphetamine are the most effective agents for the treatment of core ADHD symptoms, with a favorable efficacy and adverse event profile. 243 244 245 Compared with methylphenidate and amphetamine, which both show immediate symptom reduction, the full effects of atomoxetine and guanfacine on reducing ADHD symptoms usually only unfold after some weeks of administration. Atomoxetine and guanfacine are not controlled substances, and are licensed in various European countries and in the United States for treatment of ADHD in children above the age of 6 years. Both have been shown to be effective in decreasing ADHD core symptoms with an effect size of around 0.7, which is somewhat lower than the effect size for methylphenidate, depending on the underlying studies (e.g., Sallee et al 246 ).
Management Strategies and Duration of Pharmacological Treatment
Following an adequate dosage of medication ( Table 1 ) and treatment response, medication for ADHD should be titrated to an optimized dosage with regard to the clinical efficacy, safety, and side effects, which should be continued for as long as it remains clinically necessary and effective. This should be reviewed at least annually, also with a planned “medication break” to decide whether there is a continuing need for care. 238 239 However, there is little available empirical evidence to guide clinicians on questions, such as the optimum duration of treatment and when it is appropriate to consider drug discontinuation. As ADHD can persist into adulthood, decisions on treatment discontinuation need to be taken on a case-by-case basis. 226
Abbreviations: ADHD, attention deficit hyperactivity disorder; max. maximum.
Adapted from (1) Walitza S, Romanos M, Greenhill LL, Banaschewski T. Attention-Deficit/Hyperactivity Disorders. In: Gerlach M, Warnke A, Greenhill LL, eds. Psychiatric Drugs in Children and Adolescents. Wien: Springer; 2014:369–381 238 and (2) Walitza S, Gerlach M, Romanos M, Renner T. Psychostimulanzien und andere Arzneistoffe, die zur Behandlung der Aufmerksamkeitsdefizit-/Hyperaktivitätsstörung (ADHS) angewendet werden. In: Gerlach M, Mehler-Wex C, Walitza S, Warnke A, Wewetzer C, eds. Neuro-/Psychopharmaka im Kindes- und Jugendalter: Grundlagen und Therapie. Berlin, Heidelberg: Springer Berlin Heidelberg; 2016:289–331. 239
Among the most frequent side effects of psychostimulant therapy ( Table 2 ) are reduced appetite and sleep disturbances. 247 Appetite reduction following treatment initiation with an ADHD drug often attenuates with time. Reduced appetite at mealtimes can be avoided by taking the medication after meals rather than before. Should a clinically significant lack of appetite persist, dosage reduction (by one-fourth or half tablet of methylphenidate), discontinuation (rarely necessary), or switching to a different formulation or medication should be considered.
Adapted from (1) Walitza S, Romanos M, Greenhill LL, Banaschewski T. Attention-Deficit/Hyperactivity Disorders. In: Gerlach M, Warnke A, Greenhill LL, eds. Psychiatric Drugs in Children and Adolescents. Wien: Springer; 2014:369–381 238 ; (2) Walitza S, Gerlach M, Romanos M, Renner T. Psychostimulanzien und andere Arzneistoffe, die zur Behandlung der Aufmerksamkeitsdefizit-/Hyperaktivitätsstörung (ADHS) angewendet werden. In: Gerlach M, Mehler-Wex C, Walitza S, Warnke A, Wewetzer C, eds. Neuro-/Psychopharmaka im Kindes- und Jugendalter: Grundlagen und Therapie. Berlin, Heidelberg: Springer Berlin Heidelberg; 2016:289–331 239 ; (3) Huang YS, Tsai MH. Long-term outcomes with medications for attention-deficit hyperactivity disorder: current status of knowledge. CNS Drugs 2011;25:539–554; (4) Storebo OJ, Pedersen N, Ramstad E et al. Methylphenidate for attention deficit hyperactivity disorder (ADHD) in children and adolescents - assessment of adverse events in non-randomized studies. Cochrane Database Syst Rev 2018;5:CD012069284; and (5) Wigal T, Greenhill L, Chuang S et al. Safety and tolerability of methylphenidate in preschool children with ADHD. J Am Acad Child Adolesc Psychiatry 2006;45:1294–1303.
Nonpharmacological Treatments
Cognitive behavioral therapy.
Cognitive behavioral therapy (CBT) is a form of behavioral intervention which aims at reducing ADHD behaviors or associated problems by enhancing positive behaviors and creating situations in which desired behaviors may occur. In the case of preschool and young school children, CBT focuses on parents and educators, who are instructed and trained to act according to CBT principles, while older children and adolescents may be trained directly to use more appropriate behavioral strategies. 248 CBT and its more specific forms (e.g., social skills training, training of planning and organizational skills, and self-management techniques) have positive effects on behavior, parenting skills, child–parent relationships, and certain daily living skills, 232 249 although effects on ADHD core symptoms are inconsistent and relatively low when only blinded assessments are considered. 250 A recent meta-analysis suggested that the combined treatment of medication with CBT is more efficacious than stimulant medication alone (with an estimated standardized mean difference of 0.5). 251
Neuropsychological Treatments
In cognitive training interventions, either PC-supported or in a manualized format, cognitive exercises that tap into cognitive domains, such as working memory or inhibitory control, are performed in a repetitive manner and with increasing difficulty. The evidence base for this type of intervention is poor according to recent studies (e.g., Bikic et al 252 ) and metastudies (e.g., Cortese et al 253 ). While some “near-transfer” improvements in neuropsychological tests tapping into the trained domain are probable, the evidence for “far transfer” to academic achievements or to the ADHD symptom level is weak. Most studies, however, used the same kind of cognitive training with all participants, irrespective of their actual individual cognitive difficulties. Moreover, they did not adhere to theoretically based training principles, which recommend domain-specific training for the functional improvement of a selective neuropsychological deficit. Possibly, future approaches that combine repetitive exercise and top-down strategy application may provide larger benefits for children with ADHD.
In neurofeedback training (NF), EEG activity measured by one or more electrodes applied to the head is transformed into a visual or acoustic signal and fed back online, for example, by a stimulus moving up and down. By steering the stimulus on the screen, the participant may gain control over his/her EEG activity. Many different training protocols have been applied to ADHD. Those which have received the best evaluation are the NF training of the θ/β frequency bands ratio (the goal is generally to decrease θ and to increase β frequencies) and the training of slow cortical potentials (learning to intentionally increase and decrease cortical excitability over short periods of time). However, “normalizing” an ADHD-specific deviant EEG pattern can no longer qualify as a meaningful goal, as no characteristic ADHD pattern seems to exist (Loo et al, 254 see neurophysiology section), although gaining control over one's brain activity and over attentional states continues to be a valid treatment goal. According to parent ratings, clinical improvements after NF are stronger and longer-lasting compared with other behavioral treatment methods, but teacher ratings usually fail to yield significant effects. 255 Recent research has focused on the specificity of treatment effects, defined as the association between the learned regulation of EEG activity and the behavioral outcome. 256 To date, there is no convincing evidence that the learned control over brain activity is responsible for the observed behavioral improvements. Instead, nonspecific treatment effects, such as improved self-efficacy, positive reinforcement, and learning to sit still, seem to contribute in large part to the positive clinical outcome.
Methodologically more sophisticated NF approaches, such as tomographic NF, 257 fMRI-NF, 258 or near-infrared spectroscopy feedback (feedback of hemoglobin oxygenation) 259 are still in the experimental stage.
Noninvasive Brain Stimulation
Repetitive transcranial magnetic stimulation (TMS) and transcranial direct current stimulation (tDCS) represent other potential means to modulate cortical activity. Therefore, these approaches may also be promising in terms of improving clinical and cognitive ADHD symptoms such as inattention and impulsiveness. 258 260 261 262 Based on a meta-analysis, Westwood et al 263 suggested that left and/or right prefrontal stimulation may improve performance in attention, inhibition and/or working memory tasks. However, these approaches are not yet recommended by therapy guidelines.
Alternative Nonpharmacological Treatment Methods
Mindfulness training, physical activity, and yoga seem to have positive effects on ADHD behavior, but for the time being, the scientific evidence is weak and these treatments are seen at best as complementary to other interventions. 264 265 266 267 268 Digital home treatment programs or support apps are currently being developed for ADHD patients or their parents 269 270 ; their usefulness or clinical validity still needs to be tested. Children and adolescents with ADHD often show a great affinity with digital media, which may improve compliance, but one has to take into account that the rate of problematic internet use and gaming is enhanced in youth with ADHD (estimated at 37% in ADHD vs. 12% in TD). 271 Free fatty acid supplementation has been described to bring about small but significant reductions in ADHD symptoms even with probably blinded assessments (standardized mean difference = 0.16). 250
Long-Term Outcome
Follow-up studies have reported divergent results, with some reporting high rates of persistence until adulthood (up to 79%), 153 and others showing much higher rates of remission from childhood to adolescence (e.g., 45–55% of syndromal remissions). 272 273 274 Recent population-based studies from Brazil, the United Kingdom, and New Zealand have claimed that a large portion of de novo ADHD cases emerge at adult age, 275 276 277 but these results can probably be explained by methodological artifacts and missed subthreshold cases. 76 278 279 However, meta-analytic findings by Bonvicini et al 280 indicate that in part, different genes and polymorphisms seem to contribute to childhood ADHD and adulthood ADHD, lending some genetic plausibility to findings of a late manifestation of the disorder. According to the MTA study, the contribution of interventions administered during childhood to outcome in adulthood is negligible, but controlled intervention was limited to a relatively short period of time (14 months). 281 Neurobiologically, the course of ADHD may be explained by different models. 274 According to the first model, remission at adult age may be reduced to the normalization of brain functions through maturation. A second model explains remission through the recruitment of compensatory brain functions. The third model claims that brain function anomalies show life-long persistence, even though behavioral dysfunction may have remitted. 274 Possibly, all of these models, and probably additional ones too (see e.g., Doehnert et al 148 ), apply to different subgroups of patients or functions and may account for the divergent results in the literature.
Conflict of Interest D.B. reports having served as an unpaid scientific advisor for an EU-funded neurofeedback trial unrelated to the present work.
S.W. reports grants from Gertrud Thalmann Fonds of the UPK Basel, Collaborative Project, grants from Ebnet Foundation, grants from Mensia Technologies SA & EU H2020 SME Instrument, grants from University Medical Center Utrecht & Stanley Medical Research Institute, Collaborative Project, grants from Swiss National Foundation, Investigator Initiated Clinical Trial, other from Thieme Neuropychopharmakologie des Kindes und Jugendalters, outside the submitted work; and S.W. has received in the last 5 years royalities from Thieme Hogrefe, Kohlhammer, Springer, Beltz. S.W. has received lecture honoraria from Opopharma in the last 5 years. Her work was supported in the last 5 years by the Swiss National Science Foundation (SNF), diff. EU FP7s, HSM Hochspezialisierte Medizin of the Kanton Zurich, Switzerland, Bfarm Germany, ZInEP, Hartmann Müller Stiftung, Olga Mayenfisch, Gertrud Thalmann Fonds. Outside professional activities and interests are declared under the link of the University of Zurich www.uzh.ch/prof/ssl-dir/interessenbindungen/client/web/ .

NurseStudy.Net
Nursing Education Site
ADHD Nursing Diagnosis and Nursing Care Plan
Last updated on January 27th, 2024 at 08:57 am
Attention Deficit Hyperactivity Disorder ADHD Nursing Care Plans Diagnosis and Interventions
ADHD NCLEX Review and Nursing Care Plans
ADHD Attention Deficit Hyperactivity Disorder is a behavior disorder in the brain wherein the person has trouble paying attention and concentrating. It is the most common mental disorder diagnosed in children, and can also be seen in adolescents.
ADHD can continue into adulthood as it cannot be cured. However, people with ADHD can cope and manage symptoms with proper education and good compliance to treatment and therapy.
Signs and Symptoms of ADHD
The signs and symptoms of ADHD are usually recognizable before the age of 6. The symptoms emerge not just in one setting such as either home or school, but can manifest anytime, anywhere. The general signs and symptoms of ADHD include:
- Inability to pay attention or short attention span
- Inability to concentrate on doing tasks
- Inability to carry out instructions
- Inability to sit still
Once the child with ADHD turns into an adult, the following symptoms may also be noted:
- Frequent lateness
- Low self-esteem
- Work or relationship problems
- Procrastination
- Easily bored and/or frustrated
- Substance addiction
- Inability to control anger or other strong emotions
- Mood swings
- Impulsiveness
Types of ADHD
There are 3 types of ADHD and each has some distinct features. These include:
- Inattentive. Aside from the general ADHD symptoms, child with an inattentive type of ADHD can be observed to have the following signs and symptoms:
- Forgetfulness
- Easily distracted
- Trouble organizing daily tasks
- Dislikes activities that require sitting still such as being in class and listening to the teacher
- Doesn’t appear to be actively listening
- Often daydreams
- Often loses things
2. Hyperactive-Impulsive. In this type of ADHD, the child may exhibit the following signs and symptoms:
- Fidgeting, bouncing, or squirming while sitting
- Talking excessively
- Appears very energetic and “always on the go”
- Interrupts other people when they are talking or doing something
- Blurts out answers as soon as he/she is asked a question
- Finds it hard to wait for his/her turn
- Restlessness – always running around, climbing, jumping, or moving things unnecessarily
3. Combined. This type of ADHD features both the signs and symptoms of inattentive and hyperactive-impulsive types of ADHD.
Causes and Risk Factors of ADHD
The root cause of ADHD is still unknown. However, the following risk factors are related to ADHD, such as:
- Genetics – there is a tendency for ADHD to be passed to the next generations in a family
- Brain structure– research shows that children with ADHD has smaller frontal lobes than children who do not have this condition
- Brain chemistry – the neurotransmitter dopamine is not properly regulated by the central nervous system
- Toxins – toxic substances such as lead may affect the development of a fetus inside the womb, or a child while he/she is growing up; some research shows evidence of the maternal diet having an effect in modulating symptoms of ADHD in a fetus
- Brain disorder or injury – brain damage may lead to trouble controlling emotions, mood, thoughts, and impulses
- Pregnancy-related issues – smoking, substance abuse, drinking, poor nutrition or infections during pregnancy may affect the development of baby’s brain.
Contrary to common belief, sugar, stress, food allergies, or watching too much TV/ using gadgets excessively do not cause or trigger ADHD.
Complications of ADHD
- Accidents and injuries
- Substance abuse
- Overweight or obesity
- Eating disorders
- Sleep problems
- Delinquent or risky behavior
- Poor self-esteem
- Trouble interacting with family, friends, and peers
- Relationship difficulties
Diagnosis of ADHD
- Medical and social history of the child and family – to check for any genetic involvement, pregnancy issues, social problems, presence of any brain injury or disorder, exposure to chemicals and toxins, etc.
- Physical exam – includes neurological assessment of the senses, motor, and verbal skills
- Cognitive tests – to check for aptitude, intelligence, processing skills, or personality traits
- Neuropsychiatric EEG-Based Assessment Aid (NEBA) System – to measure the beta and theta waves in the brain; the ratio of these two waves can help determine ADHD in children and teens
Treatment for ADHD
Currently there is no cure for ADHD; however, there are many approaches to manage the symptoms of ADHD that can allow the child to live a normal life as much as possible. These include:
- Medications. Stimulants are prescribed to control the impulsive and/or hyperactive thinking and behavior in children with ADHD. Taking stimulants may promote a longer attention span and help the child think about his/her actions before doing them. In some cases of ADHD, non-stimulant medications are more beneficial. These non-stimulants include the use of anti-depressants. It is important to note that ADHD drugs may cause several side effects, such as gastrointestinal upset, fatigue, loss of appetite, headache and anxiety. Omega-3 containing supplements may also provide some benefit for ADHD clients.
- Therapy. The following therapies may help a patient with ADHD:
- Cognitive behavioral therapy (CBT) – this can effectively facilitate behavior modification so the child with ADHD may be able to function properly in the society. Through CBT, “good” behaviors can be nurtured, while the bad ones can be pruned out or modified.
- Social skills sessions – these sessions can help to train a child with ADHD on how to talk, behave, and act around other people.
- Psychotherapy – also known as counselling, psychotherapy can help an ADHD patient to explore repressed feelings and thoughts. It is also effective in exercising relaxation techniques and encouraging compliance to treatment and therapy sessions. The family and significant others of the patient should be encouraged to undergo counseling as needed.
- Support groups – involving an ADHD client in a group of people who also have ADHD or have family members who has the condition can help the patient cope with it by listening to others and also by speaking about his/her own experience with ADHD.
3. Lifestyle Changes. Getting enough sleep and exercise, lessening distractions in the child’s room, and eating a healthy and balanced diet can help manage the symptoms of ADHD.
Nursing Diagnosis for ADHD
Adhd nursing care plan 1.
Nursing Diagnosis: Disturbed Thought Process related to dopamine imbalance secondary to ADHD as evidenced by forgetfulness, inability to concentrate and pay attention, inability to do tasks as instructed, blurting of words, poor decision-making skills, and difficulty handling complex tasks
Desired Outcome: The child will perform activities of daily living as he is able to do, while being able to vent out feelings of frustration and being able to retain memory through memory techniques.
ADHD Nursing Care Plan 2
Nursing Diagnosis: Impaired Social Interaction related to hyperactivity secondary to ADHD as evidenced by restlessness, inability to listen, verbalization of low self-esteem , conflict with parents and other people, talking excessively, anxiety, blurting words, and tendency to interrupt other people when they are talking or doing something
Desired Outcome: The patient will demonstrate improved social interaction by increased participation in social events.
ADHD Nursing Care Plan 3
Risk For Delayed Growth And Development
Nursing Diagnosis: Risk for Delayed Growth And Development related to mental illness (hyperactivity) secondary to ADHD.
Desired Outcomes:
- The patient will demonstrate age-appropriate behavior.
- The patient will exhibit developmental progress.
ADHD Nursing Care Plan 4
Compromised Family Coping
Nursing Diagnosis: Compromised Family Coping related to disruptive or intrusive behavior with parents or siblings secondary to ADHD, as evidenced by expressed concern and fear by the family regarding the patient’s status, disproportionate protective behavior, anxiety, and decreased patient contact.
- The family will be able to express their thoughts and feelings, find resources to help them deal with the situation, and address the patient’s needs.
- The family will adopt effective coping strategies.
ADHD Nursing Care Plan 5
Risk For Violence: Self-Directed or Other Directed Violence
Nursing Diagnosis: Risk For Violence: Self-Directed or Other Directed Violence related to impulsivity secondary to ADHD.
- The patient will gain emotional control and refrain from agitating others.
- The patient will show no signs of abusive behavior and will promptly seek help in the event of an impending emotional crisis.
More ADHD Nursing Diagnosis
- Risk for Injury related to hyperactivity and impulsiveness secondary to ADHD
- Risk for Parental Role Conflict
Nursing References
Ackley, B. J., Ladwig, G. B., Makic, M. B., Martinez-Kratz, M. R., & Zanotti, M. (2020). Nursing diagnoses handbook: An evidence-based guide to planning care . St. Louis, MO: Elsevier. Buy on Amazon
Gulanick, M., & Myers, J. L. (2022). Nursing care plans: Diagnoses, interventions, & outcomes . St. Louis, MO: Elsevier. Buy on Amazon
Ignatavicius, D. D., Workman, M. L., Rebar, C. R., & Heimgartner, N. M. (2020). Medical-surgical nursing: Concepts for interprofessional collaborative care . St. Louis, MO: Elsevier. Buy on Amazon
Silvestri, L. A. (2020). Saunders comprehensive review for the NCLEX-RN examination . St. Louis, MO: Elsevier. Buy on Amazon
Disclaimer:
Please follow your facilities guidelines, policies, and procedures.
The medical information on this site is provided as an information resource only and is not to be used or relied on for any diagnostic or treatment purposes.
This information is intended to be nursing education and should not be used as a substitute for professional diagnosis and treatment.
Anna Curran. RN, BSN, PHN

1 thought on “ADHD Nursing Diagnosis and Nursing Care Plan”
need to order this book
Leave a Comment Cancel reply
This site uses Akismet to reduce spam. Learn how your comment data is processed .

Click through the PLOS taxonomy to find articles in your field.
For more information about PLOS Subject Areas, click here .
Loading metrics
Open Access
Peer-reviewed
Research Article
The experiences of medical students with ADHD: A phenomenological study
Roles Conceptualization, Formal analysis, Investigation, Methodology, Project administration, Visualization, Writing – original draft, Writing – review & editing
Affiliation Brighton and Sussex Medical School, Brighton, East Sussex, United Kingdom
Roles Conceptualization, Methodology, Project administration, Supervision, Validation, Writing – review & editing
* E-mail: [email protected]
Affiliation Department of Medical Education, Brighton and Sussex Medical School, Brighton, East Sussex, United Kingdom
- Megan Godfrey-Harris,
- Sebastian Charles Keith Shaw

- Published: August 22, 2023
- https://doi.org/10.1371/journal.pone.0290513
- Reader Comments
Attention Deficit/Hyperactivity ‘Disorder’ (ADHD) is a form of neurodivergence, characterised by lifelong differences in attention, impulsivity, and hyperactivity. University students with ADHD underachieve academically and tend to have lower levels of self-esteem. Medical schools have an obligation to minimise barriers for students with ADHD. Understanding the experiences of medical students with ADHD is vital to promote inclusive approaches. Our exploratory research question was: “What are the experiences of medical students with ADHD?” This was an interpretive phenomenological study. Loosely structured interviews were conducted with participants (medical students with ADHD) over Zoom. Subsequent transcripts were analysed using interpretive phenomenological analysis. Six people participated. Our analysis identified the following themes: Identity and diagnosis; ADHD profile; system issues; conflict, competition and compensation; improving the experience. Participants reported experiences of bullying and isolation at medical school, perpetrated by doctors and peers, as well as feelings of alienation when unable to conform on placement and in exams. From this, participants adopted survival strategies, such as masking, to avoid being ostracised. All recognised their ADHD status when their mental health deteriorated during their medical studies. Of those who disclosed their diagnosis, none were offered personalised support. Participants feared disclosure, largely due to weaponised professionalism and the effects of toxic competitiveness in medicine. They yearned for a sense of belonging. Participants reported strengths associated with ADHD such as empathy and working well under pressure, which are highly desirable aptitudes for doctors. This study has highlighted areas where medical schools can be instrumental in cultivating an environment where medical students with ADHD can thrive, not just survive. This may take the form of peer support groups, alongside reasonable adjustments throughout medical school–particularly for Objective Structured Clinical Examinations, for example. Enabling these students to thrive may help to prevent early burnout and subsequent attrition from medicine.
Citation: Godfrey-Harris M, Shaw SCK (2023) The experiences of medical students with ADHD: A phenomenological study. PLoS ONE 18(8): e0290513. https://doi.org/10.1371/journal.pone.0290513
Editor: Qin Xiang Ng, Singapore General Hospital, SINGAPORE
Received: March 27, 2023; Accepted: August 9, 2023; Published: August 22, 2023
Copyright: © 2023 Godfrey-Harris, Keith Shaw. This is an open access article distributed under the terms of the Creative Commons Attribution License , which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Data Availability: The data behind this meet the criteria for exemption to the data sharing policy as per the PLOS ONE online information. Our ethical approvals do not support data sharing, nor did participants consent for this. Furthermore, the data themselves are personal accounts and are thus potentially identifiable information in their entirety by virtue of what they are. The nature of this study also has the potential to be a highly stigmatised topic. Following the PLOS ONE guidance for such situations, we have included evidencing quotes throughout our results section. Ethical queries can be addressed to: [email protected] .
Funding: The authors received no specific funding for this work.
Competing interests: The authors have declared that no competing interests exist.
Introduction
Under the neurodiversity paradigm, Attention Deficit/Hyperactivity ‘Disorder’ (ADHD) is a form of neurodivergence, alongside others such as autism or dyslexia [ 1 ]. More specifically, ADHD is a neurodevelopmental label, characterised by lifelong differences in attention, impulsivity, and hyperactivity [ 2 ]. Differences may become challenges when mismatched with external factors, such as the sensory environment or differing communication styles. As such, challenges experienced can be pervasive across social, educational and/or occupational settings [ 3 ]. The prevalence of ADHD in UK adults is estimated at 3–4% [ 3 ], with a male-to-female ratio of 3:2 [ 4 ]. Prevalence in UK medical students has been found to be at least 5.5% [ 5 ]. ADHD diagnostic rates vary, influenced by factors such as gender, race, socioeconomic status, and ethnicity [ 6 ]. Students who achieve high grades in academia, such as those needed for entry to medical school, are at a particularly high risk of missed diagnosis of ADHD [ 7 ].
Current diagnostic criteria for ADHD are reliant on identifying deficits in function, consistent with the medical model of disability [ 8 ]. This enables identification of possible challenges and implementation of subsequent supports, such as medication and psychological therapy. However, deficit-based diagnosis ignores strengths such as increased energy, cognitive dynamism, and hyperfocus [ 9 , 10 ]. Cognitive dynamism describes ceaseless mental activity, which facilitates adaptability, innovation, and heightened problem-solving abilities [ 9 ]. Consideration of challenges without consideration of such associated strengths acts to reduce the experience of ADHD to a single dimension, overlooking both intersectionality and more holistic profiles. Furthermore, framing of differences as deficits is dependent on context and socio-environmental expectations, as reflected in the neurodiversity paradigm [ 11 ].
Considering external expectations is particularly important within a medical context. The wider literature is replete with studies arguing that the culture of medical schools is both toxic and competitive [ 12 ]–particularly for neurodivergent students [ 13 ]. Thus, those appearing socially different to the majority may risk falling foul of this culture through their observed differences. In the case of neurodivergent medics, this has taken the form of bullying and isolation from their peers, leading to a sense of learned helplessness [ 14 , 15 ]. Furthermore, the learning process itself is important to consider here. Whilst explicit education remains paramount, medical education continues to rely on social and experiential learning through the hidden curriculum [ 16 ]. This hidden curriculum underlies medical studies in a pervasive fashion, and through this, medical students are expected to absorb the wider culture of medicine–helping to transform them into the next generation of doctors [ 16 ]. However, due to their communication differences, it is possible that medical students with ADHD may be at a further disadvantage here. Previous research has certainly supported this assertion in the case of autistic medical students [ 14 ].
More broadly, university students with ADHD have consistently been shown to underachieve academically [ 17 ] and to have lower levels of self-esteem [ 18 ]. Therefore, students with ADHD may require psychological and social support services, in addition to academic coaching and adjustments, to achieve their full potential [ 19 ]. For example, to ensure the different domains of ADHD are supported, interventions such as cognitive behavioural therapy (CBT) are emerging as useful tools, having been shown to improve executive functioning and wellbeing [ 20 ]. Improved mental wellbeing has, in turn, been shown to have positive effects on intrinsic motivation, engagement with university, and academic success [ 19 ]. However, it is difficult to know how medical students with ADHD can be holistically supported to thrive in medical school without the input of the students themselves.
Giving voice to the experiences of students from marginalised groups is a fundamental step towards achieving social justice. These groups are often discredited and dismissed when sharing their experiences–a concept known as epistemic injustice [ 21 ]. In the case of neurodivergence, access to such stories may also prove helpful for neurodivergent students/trainees through positive role modelling, promoting the celebration of difference and acceptance of oneself [ 22 ]. Research over recent years has led to the inclusion of dyslexic, dyspraxic, and autistic voices within the literature [ 23 – 25 ]. However, what of the voices of those with ADHD? Searches identified no studies exploring the experiences of people with ADHD in medicine, nursing, or any other health professions. Learning may be impacted by differences in working memory and executive functioning similarly to other forms of neurodivergence [ 26 ]. However, differences in social domains, motivation and arousal/regulatory systems unique to ADHD are also likely to have an impact [ 27 , 28 ]. Understanding the experiences of medical students with ADHD is therefore vital to promote inclusive approaches to education, assessment, and practice. For example, under the UK Equality Act (2010), medical schools have an obligation to make adjustments to reduce barriers for medical students with ADHD [ 29 ]. However, whilst the UK General Medical Council (GMC) has provided guidance with broad examples of potential adjustments for disabled students [ 30 ], a lack of research into the experiences of medical students with ADHD means little is known regarding which, if any, of these may be useful. To that end, our research question was: “what are the experiences of medical students with ADHD?”
Materials and methods
Methodology.
This qualitative study used an interpretive phenomenological approach–seeking to explore and interpret lived experience through the perspectives of the participants [ 31 ]. An interpretive phenomenological approach endeavours to find deeper meaning and understanding of experiences in relation to the subjective world around us [ 32 ]. This is achieved by acknowledging and embracing the researchers’ insider perspectives to interpret the meanings within participants’ narratives, leading to a dynamic and intersubjective elucidation of the findings [ 32 ]. Gadamer described this concept as a “fusion of horizons” [ 33 ]. Heidegger, who developed interpretive phenomenology, suggested that humans cannot exist separately from the world around them and, therefore, to understand the everyday and authentic experiences of humans, we must consider the wider cultural, social, and political contexts surrounding us [ 34 ]. Thus, assuming an ontological approach to phenomenology [ 35 ].
Conception and positioning
The first author of this paper, Meg (MGH), is a fourth-year medical student. She was diagnosed with ADHD at the end of her second year of medical school.
“Hi , I’m Meg ! I’m a 4th year medical student . Forgetful , fidgety and fickle . These were the embarrassing aspects of my personality that I found most difficult to deal with until I was diagnosed with ADHD between second and third year of medical school . I spent more time worrying about seeming “unprofessional” than I did engaging with teaching” (MGH–first author).
Meg’s interest in this study stemmed from her own experiences of being signposted to support for dyslexic students in the absence of conclusive support for those with ADHD. This study itself was born of her own experiences, following discussion with Seb (SCKS), the second author of this paper, who is a doctor and researcher with ADHD. Seb is also autistic and dyslexic.
"Hi , I’m Seb ! I’m a lecturer in medical education . I came late to my ADHD diagnosis , during my specialty training . The lack of ADHD voices in the literature led me to not recognise this important aspect of my own intersectional identity . Diagnostic criteria aside , I attribute many of my strengths to my ADHD . For example , my creativity and resourcefulness have proved to be a blessing within the world of qualitative research” (SCKS–second author).
Prior to the study, Meg reflected on her own experience, facilitated by Seb. This reflective process enabled her to acknowledge and contextualise her preconceptions and feelings so that they could be used to positively influence the project [ 36 ]. This is particularly important in interpretative phenomenology when these perspectives are used to guide the study and the analysis of results [ 36 ].
Ethical approval
This study was approved by the BSMS Research Governance and Ethics Committee (reference: ER/BSMS9E80/2).
Recruitment
A purposive sampling approach was used. Following gatekeeper approvals, a recruitment advertisement was emailed to all medical students at a single medical school in the South of England. People who were interested were invited to contact Meg by email. They were then sent a participation information sheet and consent form to read. Informed consent was received and audio-recorded at the start of each interview.
Data collection
Drawing on the wider literature, Meg created an interview topic guide (see S1 Appendix ) iteratively with Seb, using their insider experiences. Meg then conducted loosely structured interviews with participants over Zoom. These lasted about an hour each. Broad topic areas included:
- Learning environments
- Emotional and social experiences
- Learning about ADHD at medical school
Interviews were audio-recorded, transcribed, and encrypted using Zoom’s internal software. Once Meg had reviewed and corrected the transcripts to ensure they were verbatim, they were stored securely on the university OneDrive.
Data analysis
The transcripts were analysed using the approach of Smith, Flowers and Larkin to the interpretive phenomenological analysis framework [ 37 ]. This involved Meg fully immersing herself in the data by closely reading the transcripts multiple times and making notes alongside them. Smith, Flowers and Larkin emphasize the importance of highlighting distinctive phrases and emotional responses [ 37 ], which Meg did physically on paper using pens. Next, Meg examined the notes to search for prevalent and poignant themes for each individual participant, called Personal Experiential Themes (PETs). These PETs were then compared, seeking conceptual similarities that allowed the themes to be constructed into Group Experiential Themes (GETs) across all participants. This reflects the hermeneutic circle in which the transcripts are interpreted in relation to the context, and the context is analysed in relation to the transcripts [ 38 ]. Revising the themes based on their congruence with the transcripts, and in discussion with Seb, enabled an authentic narrative of the experiences of the participants, and the impact of these experiences [ 37 ]. This was an iterative process over several months, with ever-refined changes following re-discussion and reanalysis to ensure each constructed PET and GET reflected participants’ experiences.
Six individuals participated ( Table 1 ). Participants have been given pseudonyms to personify their narratives.
- PPT PowerPoint slide
- PNG larger image
- TIFF original image
https://doi.org/10.1371/journal.pone.0290513.t001
Five GETs were constructed ( Table 2 ).
https://doi.org/10.1371/journal.pone.0290513.t002
GET1: Identity and diagnosis
Participants identified with their ADHD uniquely, and whilst some embraced it wholeheartedly, others found aspects challenging. Acquiring a formal diagnosis was tortuous, but participants valued the advantages it brought, including validation.
1a: Identity.
Participants felt ADHD was an intrinsic and inseparable part of their identity. Zara explained “ you’ve always had it . So , you don’t know what you would be like if you didn’t have it . ” This was a double-edged sword, as some feared their ADHD identity could be quickly removed at a formal psychiatric assessment if found to not have ADHD. Kate explained “ I was so scared because I was like oh my god , what happens if I don’t have it … I was petrified . ” They recognised the contextual nature of ADHD, dependant on the environment and the person. Zara reflected “it’s not one size fits all… everyone’s experience is going to be different . ” Some felt there should be a shift towards identity-first language. Emma explained “I don’t think I have ADHD . I think I am an ADHD person . ” For Amar, the chronicity and perceived lack of positives of ADHD was difficult.
Kate explained the impact of ADHD on her identity in medicine: “people love like the good characteristics of ADHD… But I feel like there’s a lot of stigma with… the bad side of ADHD… there’s still so many negative connotations of ADHD in med school . And I think there’s a lot of gaslighting of it , especially for women” . Some were subsequently apprehensive about their future in medicine. Emma explained “ a lot of the medical training isn’t suited to people with different… ways of thinking , with neurodivergence let’s say . ”
1b: Social media.
Social media had a notable effect on participants’ identities. Increased awareness brought positives and negatives. The depathologisation of ADHD was harmful. For example, Amar explained “ADHD is downplayed quite a lot… it’s like how people say… ‘everyone’s a little bit ADHD’” . Identifying with portrayals of ADHD on social media was challenging, particularly the superpower rhetoric. Emma explained “apparently , it’s big on social media , so I think it’s less stigmatized , but it doesn’t feel that way… I feel like they very much glamorize or romanticize the things that I struggle with… I clearly have something else . I’m clearly more broken somehow , more incapable somehow . ”
However, in the absence of an open culture at medical school, participants found affirmation in hearing similar experiences on social media. It was helpful for suggesting potential coping strategies–both for study and life management–as well as signposting support and treatment outlets. For example, Taylor explained how it has been helpful for them: “ hearing people’s experiences online made me think “Oh , that sounds like me . I should get assessed” … [I’m now implementing] lots of like study hacks that I saw on TikTok or Youtube” .
1c: Recognition of ADHD.
Participants had difficulty recognising and identifying with their ADHD due to stereotypes of laziness, unintelligence, and disorganisation. They also noted how the stereotype of ADHD only affecting young boys was a hindrance. Emma explained “ as a woman with ADHD , nobody had , I guess , caught on that this could be what it was because I was high achieving . ” Differing presentations of ADHD in gender could have been a barrier to diagnosis. Kate argued “I think that’s just because we’re way better at hiding our symptoms , and we’re kind of able to slightly use them more to our advantage . ” Participants experienced diagnostic overshadowing, whereby receiving diagnoses of anxiety and depression meant they were not further investigated, despite unresolved challenges at medical school.
Some had not realised how vastly their experiences differed to their neurotypical peers until their ADHD was recognised. Kate explained “ it was honestly like ground-breaking , because I genuinely thought everyone was like me” . The impact of their ADHD status not being recognised earlier was felt profoundly. Kate explained “it’s like… a mourning for kind of everything you struggled with when you were younger . ”
1d: Benefits of diagnosis.
The main benefit of diagnosis was the professional validation of their experiences and struggles. Zara explained, “ you get like confirmation that it’s just that’s how your brain works , you’re not just being lazy or being stupid , which is quite validating .” Formal diagnosis was helpful in validating their need for medication. Kate described “ diabetes is a deficit of insulin… ADHD is a deficit of dopamine . And I found that so useful in… accepting the condition… I physically am lacking in something . ” The diagnosis was also instrumental for participants’ self-discovery journey. Kate explained “ the diagnosis made me understand myself better and like made me kind to myself… I feel more in control of who I am .” As well as being kinder to themselves, participants felt better at empathising with others, including patients. Amar explained “I’ve definitely appreciated ADHD a lot more… so I think that can definitely be a positive um , especially… when I was doing psychiatry . ”
GET2: ADHD profile
Participants reflected on their strengths and challenges. They felt there were several advantages of having ADHD, as well as areas of medicine being well-suited to individuals with ADHD. However, challenges were experienced throughout medical school, affecting their relationships, mental and physical health.
2a: The positives–multidimensional.
Participants felt their ADHD led them to be more inquisitive, lateral thinkers. “ Thinking outside the box and questioning ”, as Taylor put it. Being highly empathetic was noted to be a positive, enabling them to easily build rapport with patients. Emma explained “ the way that I respond and react to emotional things… I think it helps me better relate to patients… And I think I’m quite bubbly… which makes people comfortable” .
Participants all described their ability to hyperfocus for extended periods of time. Additionally, they work most efficiently under pressure. This was beneficial for studying and working in the National Health Service (NHS). Amar explained, “ I am able to focus quite a lot… get work done , especially when I’m enjoying it… when I get started , and when I’m in the zone I can keep going for hours” . Participants felt that their dynamic learning methods would benefit neurotypical people, and feedback from peer teaching had shown this. Kate explained “ the ways we learn to like compensate it are so fool proof that , like it just works for everyone” .
Some reflected on how ADHD can be advantageous for medical work, especially in emergency medicine. Taylor explained “I knew it would always like be a stimulating environment . And like , I love learning . And I love talking to people” . Kate explained “I love it , and I think my ADHD really suits me [in the emergency department] . I’m really empathetic and intuitive… I’m able to adapt easily to different scenarios” .
2b: The challenges–communication.
Participants felt a mismatch in communication between themselves and surrounding neurotypical people. Participants’ body language was often misinterpreted, causing tension. Emma explained “ It doesn’t look like I’m listening because I need to do multiple things at once to keep engaged… a lot of people have gotten very angry ”. Participants felt their effort to match the communication of their neurotypical peers was not reciprocated. Kate explained “it’s really difficult actually to turn around to someone… to say to them actually that really hurt me , or actually that’s really insensitive… people can be very stubborn about it” .
2c: The challenges–mental health.
No participants were diagnosed with ADHD prior to reaching breaking point in medical school. For most, this came in their clinical years, when they experienced the greatest number of transitions–an absence of continuity and increased responsibility for orchestrating their learning without accountability. Kate explained “I think , because of so much content , so many new people , just so many new environments . It just overwhelmed me… There was no kind of safety in anything ”. Emma felt that medical school had been the catalyst for her diagnosis, explaining “ if I wasn’t in medical school I would never have been in that situation where everything felt out of control and unsupported” .
In a cyclical nature, participants felt their mental health deteriorated in the absence of support, but that help was inaccessible with the normalisation of poor mental wellbeing at medical school. For example, Emma repeatedly reached out for help, but experienced discounting: “ they were like ‘this doesn’t sound like you’re struggling with anything more than a normal medical student would be struggling with’ ”. Participants spiralled without support, unable to study with their deteriorating mental health. However, some precluded themselves from accessing vital ADHD support from the medical school and mental health services due to confidentiality concerns. Amar said “how anonymous is something that’s offered by the medical school . Uh that I would be a bit sceptical of” .
2d: The challenges–emotional understanding.
Participants reflected on how their strong emotive responses have been challenging, especially when not shared by neurotypical peers. Kate explained, "I’ve had to learn… sometimes my friends don’t mean to be mean . They don’t realize what they’re doing is bad” . Whilst hyper-empathy was viewed as an advantage, it was also problematic for some. Emma was aiming for a less patient-facing specialty because “ I struggle with like separating my emotions . I think that I react very strongly to the way that other people are feeling . Um , and I take it home with me , and I ruminate on it ”.
GET 3: System issues
Participants examined how they were disabled by the environment around them, rather than an intrinsic impairment. Zara explained “people with neurodivergent conditions aren’t lesser , it’s just society . ” Throughout medical school, participants felt they had to overcome additional hurdles to survive.
3a: Teaching.
Experiences of lectures felt ableist. This educational approach was physically restrictive and unengaging, placing participants at disadvantage. Kate explained “I used to hate lectures , just sitting there—horrible… I literally had no idea half the time what they were saying . ” But with mandatory attendance, participants had no choice but to attend and compensate later for missed content. Zara explained “if any lectures aren’t recorded , that’s a nightmare , because you even if you’re trying… if you’re paying attention as much as you can throughout the lecture you’ll never like , it just doesn’t pick up as well . ” Kate reflected, “we know that this stupid , old-fashioned way of teaching just is not productive and examining people , and yet we still continue to do it . ”
Participants felt that the medical school expected an unreasonable amount of flexibility for last minute timetable changes. When this was combined with participants’ innate challenges with organisation, they suffered overwhelming stress. Emma explained “having to be so flexible , I find really difficult , and it makes me really stressed… there’s no empathy or sense of understanding as to how much this can actually impact somebody like me’s life” . This was exacerbated difficult when participants had additional appointments, essential for maintaining their wellbeing.
OSCEs were particularly disabling for participants, largely due to inflexibility in timings and the structure of these assessments. Kate describes her most recent OSCE:
“I felt completely alienated. I felt different, and I knew I had a disability in that moment… all the instructions were verbal. All the questions were verbal. I couldn’t mouth read anyone. I couldn’t, you know, just sit there, and stop for a minute, everything was on the clock… I’ve had to ask them to write out the question, because I don’t know what they’re asking. And they’ll write that down the feedback that would be like ‘oh, you were struggling to like, understand the question’… Because it’s too much noise, and it’s like that auditory processing… The fact you can’t ask certain questions. You can’t check things. No OSCE I’ve been in has been alike to any clinical scenario I’ve ever been in.”
Participants felt their communication style was a disadvantage in exams, with most having failed at least one spoken assessment ( Table 1 ). The OSCEs were a key example of this. Kate examples that examiners “ notice I’m like a bit fidgety… but they think it’s like anxiety . I’m like no , it’s just me… it’s because I’ve got ADHD , and I’m fidgety .” Echoing such issues, Zara reflected:
“You just appear less kind of calm about your responses and… the way you speak is less, um, structured. So, it seems like you’re less confident… definitely fidgeting and structuring answers is always something that comes up, and it’s something I really struggle with, because to me my answer does seem structured. But to them they’re like ‘Oh, no, you’re just jumping about everywhere’” .
3c: Adjustments and helplessness.
Participants reported a lack of true supports, in favour of keeping up appearances. Emma illustrated “ I think the medical school like to sort of claim that they’re inclusive and supportive and do reasonable adjustments… but I don’t always think that it’s true . ” Taylor reflected “ the school’s offered nothing for ADHD in terms of support .” Participants were offered extra time and extensions to deadlines, regardless of helpfulness. Kate explained “ I wish it was more personalized in the learning plan . We’re all different , and we all have different needs .” Participants’ repeated efforts in getting more support were met with resistance by their medical school. This led to helpless states, whereby participants stopped trying to advocate for adjustments. Emma explained “ it’ll be like pulling teeth to get that information from the med school ” when asking for exam guidance. Participants attributed these negative responses to cost or feelings that their concerns were seen as insignificant.
Participants felt a responsibility to spend time and resources advocating for their needs–if they did not, then who would? Some tried but were met with discounting and disbelief. Kate explained, “ I know I’m very privileged , being like cisgender , like heterosexual woman , white… I feel really comfortable going in and being like , ‘okay , I struggle with this thing , and I want to talk about it’… Every day you’re having to say , if not twice a day , you’re having to go up to someone and explain why you are the way you are… And then you also have that extra like emotional burden of having to take on the fact that probably 80% of people aren’t going to listen to you , or fully take on what you’re saying” .
Stonewalling led participants to feel helpless. Amar explained “ It’s just up to their judgment of what it is they decide to attribute to ADHD and what they don’t , uh , rather than necessarily based on your personal experience . ” Kate explained “ we’ve all been having to cope with it so long . We know what helps us” .
3d: Hidden costs.
Costs associated with being in a minority student group, known colloquially as ‘minority tax’, refers to uncompensated efforts and responsibility to reduce inequalities between themselves and their peers. There was a minority tax associated with having ADHD at medical school, taking its toll in time, money, energy, and emotions. Travel was particularly costly, especially in placements far from home. These involved distance from their usual support systems and unfamiliar and/or complex journeys. Emma explained, “ sometimes I think that I need to get a taxi . I’ll get a taxi , and then they won’t reimburse it because there is a bus… on the bus where it’s crowded , lots of different people . Everybody’s loud . Everybody is talking , lots of different smells , lots of different things happening . ” Zara was embarrassed when she explained “I’ve really struggled with… traveling to kind of new places like when it’s a one off or not very frequent… Like… the planning of like the travel and things like that . ”
Medication alleviated many struggles, reducing unhealthy coping mechanisms such as smoking, drinking alcohol and binge eating. These improvements allowed energy and time to be diverted towards studying and engaging with placement. Whilst this was a dramatic improvement, medication cost money and was not the ‘magic bullet’ in providing equity with peers. Kate explained “I’m not quite as focused as the normal person still . But it’s enough for me to cope with” .
Taylor regularly attended therapy, enabling them to cope better with the emotional and social impacts of ADHD at medical school. However, Taylor acknowledged their privilege in being able to access multiple avenues of support privately. They felt that the medical school could play a role in achieving equity. They said, “ I think if other people have support whether that be coping strategies or therapy , or assessments or support groups then that would help people” .
GET 4: Conflict, competition and compensation
Interactions with peers and staff significantly impacted participants’ experiences of medical school. Some experienced direct discrimination against their ADHD, causing overtly negative attributions. However, experiences of additional microaggressions invariably contributed to feelings of mistrust, isolation, and internalised ableism.
4a: Bullying.
The experience of being bullied by doctors, particularly senior doctors, was normalised amongst participants. Emma recited her first-time history taking, “it made me cry because I was trying really hard , and [the doctor] essentially told me that I shouldn’t be a doctor… [I] was reprimanded in a really cruel way” . Taylor also experienced bullying on the ward by a consultant, they said “I went and cried for a bit in the toilets , did my deep breathing , and then went back… we get on with our day” . When Taylor experienced bullying, they blamed themselves for being upset, explaining “someone who was less sensitive or maybe more resilient might have been able to handle it” . Throwaway comments from consultants about ADHD and participants’ ability to achieve was damaging to their self-esteem. Emma explained “ that’s still made me doubt to a certain extent whether I can do this , and that’s something I think I’m gonna struggle with daily” .
4b: Hostility on clinical placements.
New clinical placements triggered anxiety. Participants feared how new teams would receive them, embedded in feelings of personal inferiority. Zara explained “ being new on the ward or being new in a place , and you just don’t know how people are going to react to you… But then , after that , you’ve met them once at least , so you can kind of do better” . More often than not, however, participants were simply ignored. Zara explained “ they just ignore you… it feels like there’s no point in you being there because you’re not taking anything in . ” When they tried to actively engage, they faced hostility. Emma explained, “I have to be really ballsy , and like , ask a lot of questions to keep myself engaged in learning… and then the consultant will be like , “Why are you interrupting my ward round ? Why are you talking ? ” But they won’t answer my questions if I ask .”
4c: Surviving.
Participants developed survival strategies to avoid humiliation–rigorously self-regulating and forming a protective shield. Subsequently, survival became easier with time. Emma explained “I’ve got like tougher skin… consultants call me stupid , I move on… I know a lot of the consultants… so I know how I need to react to them . ”
A vast amount of energy was expended masking (hiding) their ADHD. Take Taylor, for example, who said that “ I do things so people don’t comment” , but later explained “everything is so much easier [with medication] …and not like being so depleted of… all of my spoons” . There was little reserve for learning when participants prioritised masking. Emma explained, “ that extra worry of… making sure that you’re not seeming distracted , and you’re seeming engaged , and you’re making the patient feel safe and comfortable and able to talk to you… that’s a lot of things to have to do all at once” .
Exhaustion from masking on placement exacerbated executive functioning differences and thus negatively impacted motivation for self-study. As a result, basic activities of daily living, such as eating, felt insurmountable with their little remaining energy and executive functioning capabilities. Emma explained “there are literally like a week’s worth of dishes just lying around… Like it’s a mess in here , and the reason it’s a mess is because I’ve got a lot going on at university . ”
Seemingly small mistakes significantly worsened participants’ experience of medical school, especially at regional placements. Zara explained “ I’ve forgotten my laptop . I’ve forgotten chargers , I’ve forgotten clothes . I like really struggle with packing week to week , and so often found kind of I don’t have the things that I need .” Most experienced time blindness, and despite implementing coping strategies, they consistently arrived late. Or worse–lost marks in assessments due to not managing time ‘appropriately’. For example, Tiah explained “ I’m like pretty much late to everything . I always , always feel stressed about it… I find the whole concept of OSCEs very tricky because I struggle so much with time and organizing myself” .
4d: Professionalism.
Fear of weaponised professionalism was a barrier to participants disclosing their ADHD to the medical school. Weaponised professionalism in this context refers to characteristics inherent to ADHD being perceived inappropriately as unprofessional, despite these characteristics likely bearing no true impact on their performance as medical students, or on patient care. Seeing ADHD be used to ‘prove’ incompetence of a peer deterred Amar from disclosing his diagnosis, explaining “ I have an inherent distrust of medical schools .” There was a scepticism of the premise for collecting disability data from medical schools and the GMC. Emma explained, “I worry that because people don’t understand it… they will not… inform me of opportunities that they don’t believe that I can do” . Professionalism concerns had been raised relating to ADHD traits. Kate experienced a strong sense of moral injury when a consultant criticised her professionalism for consoling a distressed patient and fidgeting in clinic. Kate left, explaining “ it felt like such an attack on who I am and everything I stand for” . She also felt her gender had a part to play in being perceived as unprofessional, explaining “like female characteristics they just were so against” .
4e: Peer interactions.
Participants were wary of disclosing their ADHD to peers, but not to people outside of medicine. As Kate explained, “I think my ADHD characteristics [at work] has always been viewed so positively… but I find that in med school , I think I’m negatively treated because of it” . Many experiences with peers centred around either overt judgement or a fear of judgement. This negatively impacted disclosure and wellbeing. Emma recalled, “ the way [peers] talk about [ADHD] before they find out that I’m like that makes me self-conscious and hyper-aware and hyper-vigilant and makes me struggle to be sociable . ” Kate echoed this, “everyone just talks negative about [ADHD] which kind of pulls you down a bit” .
4f: Competitiveness.
Participants attributed negative interactions with peers to a toxically competitive environment at medical school. Kate argued “I think up till now it’s kind of been viewed , if you say things that are disabilities or health issues that you’re making an excuse . I think it’s very toxic” . They felt there was a perceived weakness of ADHD in medicine. Amar explained “ at the end of the day… I don’t think I would get much empathy from anyone… I don’t think they would take me like , you know , um , seriously” .
Some felt ashamed that they needed ADHD medication to survive medical school. Competitiveness led to likening use of ADHD medication to cheating. Emma explained, “I think it feels a bit like cheating because you know that like the medication you take , other students take to study” .
4g: Shamefully perfect.
A combination of feelings of inferiority and the competitive environment led to perfectionist mindsets. In turn, this further fostered masking behaviours in an attempt to hide their secret shame. Kate explained “ I’ve previously always been known to be… hyper-organised . [In] hindsight , that was me compensating” . Participants set impossible expectations for their studies causing overwhelm and frustration. Zara explained “ when you have ADHD you don’t know what’s normal and what’s not normal . You just think you’re kind of like lower in the general ability compared to your peers” .
Participants had difficulty recognising their hard work and the contributions this has to their success. They attributed success to luck, but failures to their own wrongdoings. Some felt fraudulent in having an ADHD diagnosis itself–worried they were just making excuses for not coping. Emma, for example, avoided disclosing initially due to “ suffering with all that imposter syndrome stuff and feeling like a fraud” .
GET 5: Improving the experience
Participants reflected on their positive experiences and how aspects of these could be applied elsewhere in medical school. They also explored how negative experiences could have been improved.
5a: Engagement and accountability.
Environments where participants were encouraged to engage, without fearing repercussions, were most conducive for learning. Examples included small-group sessions and simulation. Amar said, “those are the ones I take the most from… where you get the chance to speak .” Enjoyment on placement correlated with positive engagement from the team. Participants valued having a friendly face on the ward, such as a clinical fellow. It enabled them to quickly become comfortable in potentially hostile environments, maximising learning opportunities that may have otherwise been missed.
Participants needed accountability to stay motivated and engaged with the course. For example, some found regular contact and soft deadlines valuable. Zara explained “ just having more checking ins… I… think it’s quite useful… because it has that outside accountability” . Their attempts at undirected studying with peers had limited success because they often digressed from the task at hand. Instead, they felt academic tutors that provided accountability would be more beneficial.
In their pre-clinical years, a checklist of lectures required for exams was beneficial for participants who had difficultly planning self-study. In the clinical years, however, participants had to fend for themselves, leaving them unable to prioritise and rationalise which knowledge was needed. Emma explained, “ they don’t provide very clear guidelines , or like lists of things that need to be covered , and so that… it gives me too much freedom to do what I actually enjoy , and then I end up , not covering the stuff I need to be covering ”. Participants found initiating self-study in the clinical years became almost impossible with the lack of routine.
5b: Reducing minority tax.
When participants were proactive in accessing support, this was financially and emotionally expensive. To reduce minority tax on placement, Kate suggested the use of learning support cards. She explained “ Like in the clinical years , I just want something that says I’ve got these things , this is what helps me . Just to show that I’m not bull*******g” . It was felt that neurotypical allies could strive to make clinical spaces more inclusive for their colleagues.
5c: Community.
A culture of silence was isolating for participants, who then felt liberated when meeting other students with ADHD. Emma explained “ Nobody talks about it… Why don’t we talk about it ? [Meeting other medics with ADHD] made me feel like I wasn’t so strange” . They yearned for belonging. Taylor explained “ humans like to form communities with people who are similar to them in environments that are different and challenging” . Participants wanted to exchange experiences with other medical students with ADHD, signposting helpful resources and ultimately providing validation. Kate explained “ I love when I get to chat to other medics with ADHD… it kind of fulfils everything I feel about myself” . Participants with an overbearing fear of disclosure were particularly isolated. As Amar described, “ you would be the first medical student I know… I’m not aware of medical students or doctors with ADHD . ”
5d: Role modelling.
Role modelling was important for participants’ self-esteem, providing validation and encouragement. Connecting with doctors with ADHD and senior medical students provided reassurance that their dreams were achievable with ADHD, not despite it. Emma explained “ to see that there are doctors who can achieve the things that people sometimes say “Oh you maybe don’t go for that… don’t aim so high’… It was very encouraging to see that you can aim high and you can achieve it , and it doesn’t stop you from doing anything ”.
Some thought it would be helpful to hear how challenges of ADHD in medicine can be overcome through mentoring. Kate explained “I’d love to go chat someone just be like ‘how is it ? ’ , and I hope they would get paid for it as well” , acknowledging the often-unremunerated nature of mentoring. Meeting a doctor with ADHD on placement meant Emma saw a different style of working, providing her with the confidence and permission to develop her own style of doctoring. Kate also noted the benefit of having visible ADHD role models from an early age. On her paediatrics rotation, parents informed her of the positive impact she had for being proud and unapologetically ADHD.
This was the first study to explore the experiences of medical students with ADHD. Whilst positives, such as cognitive dynamism and increased empathy, were noted, overall experiences were overwhelmingly negative. Ableism was pervasive. In particular, internalised ableism coloured their entire lifeworlds–if they could not pass within the neuromajority, how could they have a place in medicine? Such internalised ableism is associated with low self-esteem, reduced wellbeing, and increased feelings of isolation [ 39 ]. Some participants felt broken, others felt a need to prove they were not broken. Both mindsets fostered a sense of shame, reinforced by fear of ill-treatment if they were identified as different. Participants therefore went to great lengths to mask (or camouflage) their ADHD–sometimes this was conscious, other times not. No studies have explored masking ADHD in adulthood or its impacts. In autistic adults, however, masking has been associated with poor mental health, burnout, and suicide [ 40 , 41 ]. In this study, our participants did indeed describe the vast amount of energy spent on masking their ADHD. This pervasively impacted their whole lives, in and outside of their medical studies–putting strain on their relationships, their mental health, for example. This may, in part, explain the higher rates of mental ill health that neurodivergent doctors seem to experience [ 42 ].
Participants were exhausted from the constant masking. The overbearing pressure to conform–to meet the social norms amongst neurotypical peers–and to embody the cultural norms of medicine more broadly, took its toll. This pressure increased once reaching clinical placements, through fear of weaponised professionalism. The weaponisation of professionalism is not a new phenomenon. The concept of professionalism itself is historically grounded in cultural norms associated with the white, cis-gendered, heteronormative, able-bodied male experience [ 43 ]. Our participants were at a particularly high risk of weaponised professionalism as they all had multiple intersectional identities, which has been shown to increase this risk in healthcare [ 44 ]. For example, throughout the interviews, female participants highlighted how their gender seemed to negatively impact the way they were perceived by others. Participants further alluded to this weaponization of professionalism in their recollection of experiences of OSCEs–recalling negative feedback on differences in communication styles and their sensory needs. Training OSCE examiners in neurodiversity-affirmative marking, including awareness of different neurotypes and communication styles [ 45 ], could be a potential adjustment under the UK Equality Act of 2010. Such an adjustment would be supported by the GMC, who acknowledge that a disability is not a fitness to practise concern in itself [ 30 ].
Participants felt alienated from peers, educators, and the institution, following experiences of direct discrimination and microaggressions. A mismatch in communication styles with neurotypical peers and educators also seemed to contribute to feelings of isolation. This concept is best described by the double empathy problem, often seen in the context of autism, whereby communication difficulties are due to reciprocal mismatches in communicative style between neurotypes rather than a social deficit in the non-neurotypical [ 46 ]. Therefore, had participants’ communication styles been assessed in the context of communicating with others with ADHD, these may have been deemed appropriate (or even excellent) rather than deficient. This acknowledges the effect of power on such entrenched views around right and wrong ways of communicating.
Whilst participants received negative feedback for their communication styles, a body of doctors with diverse communication styles may better meet the needs of the diverse patient population–in line with GMC Welcomed and Valued [ 47 ]. Participants strived to conform to neurotypical communication styles–another form of masking–at the expense of their mental health to avoid being outcast.
Participants felt social media negatively impacted their self-esteem with inaccurate and romanticised depictions of ADHD, which is congruent with recent studies that show over 50% of videos about ADHD on TikTok and YouTube are misleading, especially when they are produced by non-healthcare workers [ 48 , 49 ]. As per our participants’ experiences, wider research also shows that social media can negatively impact psychological wellbeing and self-esteem [ 50 ]. Interestingly, in previous research, videos rated the most useful were those that focused on lived experience [ 50 ]–something that our participants also emphasised. Thus, illustrating the need for doctors with ADHD to be openly visible as role models, showing they can be successful with ADHD, not despite it. This is in keeping with previous research, which found that autistic medical students desired openly autistic role models within the medical profession [ 14 ]. Here, if our participants’ desires for positive role modelling are met, it may well steer them onto a path of increased self-confidence and reduced internalised ableism–helping them to pursue their dreams and advocate for their needs–instead of one that leads to burnout and attrition [ 22 ]. This may help students to embrace their differences, rather than suppressing them. A support network for medical students with ADHD may also contribute to positive outcomes through reducing the reported feelings of alienation and isolation.
Compassion and self-compassion are protective factors against emotional exhaustion and burnout in medical students and doctors [ 51 ]. However, our participants experienced callousness at medical school, from others and themselves. This toxic culture and its impacts have been demonstrated in other studies, likely fostered by an emphasis on competitive achievement needed for the UK ranking system following medical school graduation [ 12 , 52 ]. Perhaps a shift towards collaborative learning, which participants noted to be their favourite, could nurture a more compassionate and kind medical school culture which may ultimately improve patient care [ 52 , 53 ].
Their medical school’s potentially tokenistic approach to inclusion–as reported by our participants–may not be fully in keeping with the UK Medical Schools Council’s active inclusion guidance [ 54 ]. The GMC also highlights that disabled students should be consulted to find the most appropriate adjustments for their individual circumstances [ 30 ]. Despite this, and whilst our participants reported multiple attempts to advocate for their needs, they reported that their cries for help were disbelieved. Adjustments which increase accountability and focus on organisation and time management were felt to be most beneficial. Diagnosis and holistic support for participants was inaccessible without financial wealth. The GMC, however, suggests that medical schools should fund support services and referrals if it is unfeasible through the NHS–and that such services should be independent from the medical school [ 55 ]. This could provide some further protection of confidentiality, which concerned participants.
Limitations and strengths
As this is a qualitative study, our results are not generalizable. Instead, our study presents an in-depth exploration of the experiences of a sample of mostly cis-gender females from one medical school in England. This sample was well-suited for phenomenological research, enabling intimate exploration of participants’ experiences. The study strived for an in-depth analysis of the experiences of current medical students with ADHD. Therefore, it did not include the voices of those whose ADHD may be unrecognized, nor did it include those who may have left medical school.
Others involved in participants’ subjective reports of their experiences may have different recollections of events. However, the purpose of the study is to understand the perspectives of our participants. There may also be an element of volunteer bias, whereby participants chose to volunteer because they have powerful stories to tell. However, this does not mitigate or lessen their own experiences.
This is the first study of the experiences of medical students with ADHD. Meg’s insider status was key to building rapport with participants and to engaging with and understanding their stories during the analysis. It is also worth acknowledging here that, given our insider status, there is a possibility our own subjective experiences and perceptions could have influenced which examples of participants’ reported experiences were focused on. Whilst a positivist or critical realist perspective may consider this a limitation, this may also be considered a strength through a social constructionist approach to interpretive phenomenological research [ 35 , 50 ].
Participants reported strengths associated with ADHD such as empathy and working well under pressure, which are highly desirable aptitudes for doctors. However, participants also reported experiences of bullying and isolation at medical school, perpetrated by doctors and peers, as well as feelings of alienation and inferiority when unable to conform on placement or in exams. From this, participants adopted survival strategies, such as masking, to avoid being ostracised. All recognised their ADHD status when their mental health deteriorated during their medical studies. Of those who disclosed their diagnosis, none were offered personalised support. Participants feared disclosure, largely due to weaponised professionalism and the effects of toxic competitiveness in medicine. They yearned for a sense of belonging. This study suggests a key starting point for medical schools is to listen to their medical students, and take action to support each individual student. To have a wider impact, medical schools should evaluate how they deliver OSCEs and consider additional training for examiners.
This study has highlighted areas where medical schools can be instrumental in cultivating an environment where medical students with ADHD can thrive, not just survive. Further research is now needed to identify which adjustments are effective and to explore the experiences of non-ADHD medical students and staff in relation to medical students with ADHD.
Supporting information
S1 appendix. interview topic guide..
https://doi.org/10.1371/journal.pone.0290513.s001
Acknowledgments
We would like to thank our participants for taking part in this study. This study was undertaken as MGH’s Individual Research Project as part of her medical degree at Brighton and Sussex Medical School. SCKS was her supervisor.
- View Article
- PubMed/NCBI
- Google Scholar
- 2. American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders. American Psychiatric Association; 2013.
- 29. UK Government. Equality Act 2010 [Internet]. Available from: https://www.legislation.gov.uk/ukpga/2010/15/section/6
- 31. Moran D. Introduction to Phenomenology. London: Routledge; 2004.
- 34. Heidegger M. Being and time. Oxford: Blackwell Publishers; 1962.
- 36. Shaw SCK, Anderson JL. Phenomenological research in medical education: an overview of Its philosophy, approaches, and conduct. In: SAGE Research Methods Cases Part 2. SAGE Publications Ltd; 2018.
A .gov website belongs to an official government organization in the United States.
A lock ( ) or https:// means you've safely connected to the .gov website. Share sensitive information only on official, secure websites.
- Data and Statistics on ADHD
- Free Materials on ADHD
- Attention-Deficit / Hyperactivity Disorder Articles
- Clinical Care and Treatment
Attention-Deficit / Hyperactivity Disorder (ADHD)
About Attention-Deficit / Hyperactivity Disorder (ADHD)

Is it ADHD?

Symptoms of ADHD

Treatment of ADHD

ADHD Information and Resources for States

School Changes — Helping Children with ADHD

CDC's Attention-Deficit / Hyperactivity Disorder (ADHD) site includes information on symptoms, diagnosis, treatment, data, research, and free resources.
For Everyone
Health care providers.
Thank you for visiting nature.com. You are using a browser version with limited support for CSS. To obtain the best experience, we recommend you use a more up to date browser (or turn off compatibility mode in Internet Explorer). In the meantime, to ensure continued support, we are displaying the site without styles and JavaScript.
- View all journals
- My Account Login
- Explore content
- About the journal
- Publish with us
- Sign up for alerts
- Population Study Article
- Open access
- Published: 07 May 2024
Risk of traumatic brain injury among patients with ADHD and their unaffected siblings
- Ping-Chung Wu 1 , 2 ,
- Shih-Jen Tsai 2 , 3 ,
- Ju-Wei Hsu 2 , 3 ,
- Kai-Lin Huang 2 , 3 ,
- Tzeng-Ji Chen 4 , 5 , 6 ,
- Tai-Long Pan 7 , 8 , 9 &
- Mu-Hong Chen ORCID: orcid.org/0000-0001-6516-1073 2 , 3
Pediatric Research ( 2024 ) Cite this article
360 Accesses
2 Altmetric
Metrics details
As the relationship between attention deficit hyperactivity disorder (ADHD) and traumatic brain injury (TBI) is gaining increasing attention, the TBI risk in patients with ADHD, unaffected siblings of ADHD probands, and non-ADHD controls remains unclear.
Overall, 18,645 patients with ADHD, 18,880 unaffected siblings of ADHD probands, and 188,800 age-/sex-matched controls were followed up from enrollment to the end of 2011. The cases of TBI and TBI requiring hospitalization were identified during follow-up.
Patients with ADHD (hazard ratio [HR]: 1.57) and unaffected siblings (HR: 1.20) had an increased risk of any TBI compared with non-ADHD controls. Surprisingly, the likelihood of developing TBI requiring hospitalization during follow-up was higher in the unaffected siblings group (HR: 1.21) than in the control group, whereas it was lower in the ADHD probands group (HR: 0.86).
Conclusions
Patients with ADHD and unaffected siblings of ADHD probands were more likely to develop any TBI during follow-up than controls. Unaffected siblings of patients with ADHD exhibited the highest risk of subsequent TBI requiring hospitalization compared with patients with ADHD and healthy controls. Therefore, TBI risk in patients with ADHD and their unaffected siblings would require further investigation.
ADHD diagnosis and ADHD trait are associated with risk of traumatic brain injury (TBI).
Both patients with ADHD and their unaffected siblings were more likely to develop TBI during the follow-up compared with the control group.
TBI requiring hospitalization occurred more in the sibling group than in the proband group.
TBI risk should be closely monitored among unaffected siblings of patients with ADHD.
Similar content being viewed by others

Alzheimer’s disease risk reduction in clinical practice: a priority in the emerging field of preventive neurology
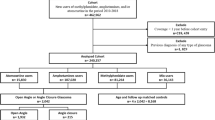
Medications for attention deficit hyperactivity disorder associated with increased risk of developing glaucoma

Introduction
Attention deficit hyperactivity disorder (ADHD) is the most prevalent neurodevelopmental disorder among children, with an estimated prevalence increasing from 6.1% in 1997–1998 to 10.8% in 2022 according to the National Health Interview Survey of the U.S. population. 1 , 2 ADHD often persists into adulthood and affects approximately 2.–3.4% of the adult population. 3 , 4 Individuals with ADHD mostly have symptoms of inattention, hyperactivity, impulsivity, or a combination of these symptoms, which compromise basic functions and may adversely affect subsequent mental and physical health. 5 , 6 , 7 , 8
Previous studies have demonstrated that both ADHD probands and their unaffected siblings tend to have impaired performance in a wide range of neuropsychological functions such as sustained attention and executive functions. 9 , 10 , 11 Gau and Huang assessed attention performance in ADHD probands, unaffected siblings, and healthy controls using the Rapid Visual Information Processing (RVP) task of the Cambridge Neuropsychological Test Automated Battery (CANTAB). Subsequently, they discovered that probands with ADHD and their unaffected siblings had significantly higher total misses and a lower probability of hits in the RVP task than controls. 9 Similarly, through analysis of the results of RVP-total hits, Pironti et al. found that cognitive impairments, especially in sustained attention, were present in both ADHD patients and their relatives. 10 Increasing evidence has suggested that unaffected siblings of ADHD probands may exhibit a common endophenotype with their ADHD siblings and exhibit some deficits in attention, working memory, behavior inhibition, and executive functions. 12 , 13 , 14
Traumatic brain injury (TBI), one of the major causes of death and disability in children, adolescents, and young adults globally, causes severe sequelae and burdens on the lives of patients, their families, and society. 15 , 16 , 17 It has been estimated that more than 1.4 million people sustain a TBI each year in the United States, of whom 50,000 die from their injuries. 18 Nguyen et al. performed a systematic review and meta-analysis of the global incidence of TBI and discovered a pooled incidence rate of 349 per 100,000 person-years for all ages. 19 With its rapidly increasing prevalence and the increasing years of life lived with disability (YLDs) globally, TBI contributes considerably to the global injury burden. 20
Several studies have suggested the potential relationship between ADHD and TBI. 21 , 22 , 23 Ilie et al. conducted a cross-sectional study of 3,993 Canadian adults and observed significant positive associations between lifetime TBI and both current and past ADHD in this population. 21 By comparing student athletes who had sustained a mild TBI with controls of similar age and sex, Biederman et al. reported that mild TBI subjects had a significantly higher rate of ADHD than controls, and that in all subjects, the onset age of ADHD was before the onset age of mild TBI. 22 Furthermore, in a retrospective cohort study, Liou et al. demonstrated that patients with ADHD had a higher incidence of TBI than controls. 23 However, few studies have investigated the likelihood of subsequent TBI development among ADHD patients, unaffected siblings of ADHD probands, and healthy controls. In a study consisting of 5,128 unaffected siblings of ADHD probands and 20,512 age- and sex-matched controls, Wei et al. observed that the unaffected siblings of patients with ADHD were more likely to develop TBI later in life compared with controls. 24 The likelihood of subsequent TBI development among ADHD patients, unaffected siblings, and healthy controls is a topic worth exploring because the relationship between ADHD and TBI is gaining increasing attention, and the fact that unaffected siblings of ADHD probands may exhibit a common endophenotype and similar cognitive impairments with their ADHD siblings should be considered. Nevertheless, further studies and understanding of this topic seem to be limited. Furthermore, the effects of ADHD medications on the risk of subsequent TBI, the severity of subsequent TBI, and the age of TBI diagnosis have been rarely discussed in previous publications.
In this longitudinal, population-based cohort study, we investigated the risk of subsequent TBI, including skull fracture, concussion, contusion, and brain hemorrhage following injury, among patients with ADHD and their unaffected siblings and assessed the effect of ADHD medications on the risk of subsequent TBI, the severity of subsequent TBI, and the age of TBI diagnosis using the Taiwan National Health Insurance Research Database (NHIRD). We hypothesized that ADHD probands may have the highest risk of subsequent TBI, followed by unaffected siblings and controls during follow-up.
Data source
Taiwan NHIRD which consists of healthcare data from >99.7% of the entire Taiwan population is audited and released by National Health Research Institute for scientific and study purposes. In current study, we linked three databases together for the analysis. The first is the registry database for all beneficiaries (~28,000,000), which was used for the genealogy reconstruction and demographic characteristics based on Chen et al’s and Cheng et al’s methods. 25 , 26 The second is the specialized dataset of mental disorders, which includes all medical (mental and non-mental) records between 2000 and 2011 of all insured individuals with mental disorders, and was used for the identification of ADHD probands. The third is the Longitudinal Health Insurance Database, which includes all medical records between 1996 and 2011 of 3,000,000 insured individuals that are randomly selected from entire Taiwanese people (~28,000,000), and was used for the identification of the unaffected siblings and control group. Individual medical records included in the NHIRD are anonymous to protect patient privacy. The diagnostic codes used were based on the International Classification of Diseases, 9th Revision, Clinical Modification (ICD-9-CM). The NHIRD has been used extensively in many epidemiologic studies in Taiwan. 25 , 26 , 27 , 28 Institutional Review Board of Taipei Veterans General Hospital approved the study protocol and waived the requirement for informed consent since this investigation used de-identified data and no human subjects contact was required.
Inclusion criteria for patients with ADHD, unaffected siblings and the control group
Patients who had a diagnosis of ADHD (ICD-9-CM code: 314) without prior TBI history between 2001 and 2010 were identified from the specialized dataset of mental disorders. To ensure diagnostic validity, a diagnosis of ADHD was given by board-certified psychiatrists at least twice (i.e., one psychiatrist at two different time points or two different psychiatrists) according to the clinical diagnostic interview and professional judgment. Individuals who had no ADHD diagnosis at any time in the database but had any sibling with ADHD were included as the ADHD sibling cohort (unaffected sibling group). The term “unaffected” sibling was probably a group that is not meeting the threshold for ADHD diagnosis compared with the identified ADHD probands but may share some of the underlying genetic as well as environmental risk factors for ADHD. 29 , 30 , 31 The age-, sex-, birth time-, and residence-matched (1:10) control cohort was randomly identified from the Longitudinal Health Insurance Database after eliminating the study cases, those who had been given a diagnosis of ADHD at any time in the database, and those with any sibling with ADHD. Those who were diagnosed with TBI prior to January 01 2001 were excluded in the unaffected siblings and control group. The time of ADHD diagnosis was defined as the enrollment time in the ADHD proband group; January 01 2001 or the birthdate was defined as the enrollment time in the unaffected siblings and control groups. In addition, the long-term use of ADHD medications (methylphenidate or atomoxetine) during the follow-up was defined by the cumulative defined daily dose (cDDD) during the follow-up ≥ 365. 8 The DDD recommended by the World Health Organization (WHO) Collaborating Center for Drug Statistics Methodology is a unit for measuring a prescribed amount of drug. The DDD is the assumed average maintenance dose per day of a drug consumed for its main indication. We calculated the sum of the dispensed DDD (cDDD) of ADHD medications during the follow-up period. Level of urbanization (level 1 to level 5; level 1: most urbanized region; level 5: least urbanized region) was also assessed for our study. 32
Main outcomes
TBI, including fracture of skull (ICD-9-CM codes: 800 ~ 801, 803 ~ 804), concussion (ICD-9-CM code: 850), contusion (ICD-9-CM code: 851), brain hemorrhage following injury (ICD-9-CM codes: 852, 853), and unspecified intracranial injury (ICD-9-CM codes: 854, 959.01), was identified during the follow-up (from enrollment to December 31 2011 or to the death). In addition, TBI requiring hospitalization was also identified.
Statistical analysis
For between-group comparisons, the F test was used for continuous variables and Pearson’s X2 test for nominal variables, where appropriate. Cox regression models with adjustment of age, sex, residence and income were used to examine the hazard ratios (HRs) and 95% confidence intervals (CIs) of subsequent TBI and TBI requiring hospitalization in ADHD probands and unaffected siblings compared with the control group. Furthermore, we assessed the TBI and TBI requiring hospitalization likelihoods among ADHD probands with and without long-term use of ADHD medications, unaffected siblings, and control group. A 2-tailed P value of less than 0.05 was considered statistically significant. All data processing and statistical analyses were performed with Statistical Package for Social Science (SPSS) version 17 software (SPSS Inc.) and Statistical Analysis Software (SAS) version 9.1 (SAS Institute, Cary, NC).
In all, 18,645 patients with ADHD, 18,880 unaffected siblings of such patients, and 188,800 age-/sex-matched controls were included in our study. Patients with ADHD (4.48 ± 4.99 years) were younger than the other two groups (~ 6 years, p < 0.001) (Table 1 ). The ADHD proband group was male predominant (79.7%). During the follow-up, the ADHD probands had the highest incidence of developing any TBI (18.9%, p < 0.001), while the unaffected siblings had the highest incidence of developing TBI requiring hospitalization (1.5%, p = 0.005) (Table 1 ). TBI occurred younger in patients with ADHD (8.97 ± 6.15 years) and unaffected siblings (9.85 ± 7.24 years) than in the control (10.17 ± 7.59 years, p < 0.001) (Table 1 ). However, the TBI events took longer to occur in the ADHD proband group (4.56 ± 3.17 years) than in the other two groups (4.04 ± 2.84 years in unaffected siblings, 4.15 ± 2.88 years in the control group, p < 0.001) (Table 1 ).
Kaplan-Meier survival analyses with the log-rank tests of any TBI ( p < 0.001) and TBI requiring hospitalization ( p < 0.001) risks between groups were shown in the Fig. 1 . The Cox regression models with full adjustment of age, sex, income, and level of urbanization showed that the patients with ADHD (HR: 1.57, 95% CI: 1.51–1.63) and the unaffected siblings of such patients (HR: 1.20, 95% CI: 1.15–1.25) were more likely to develop any TBI during the follow-up than the control group (Table 2 ). Surprisingly, the unaffected siblings (HR: 1.21, 95% CI: 1.07–1.37) were more likely, while the ADHD probands (HR: 0.86, 95% CI: 0.75–1.00) were less likely, to develop TBI requiring hospitalization during the follow-up compared with the control group (Table 2 ).
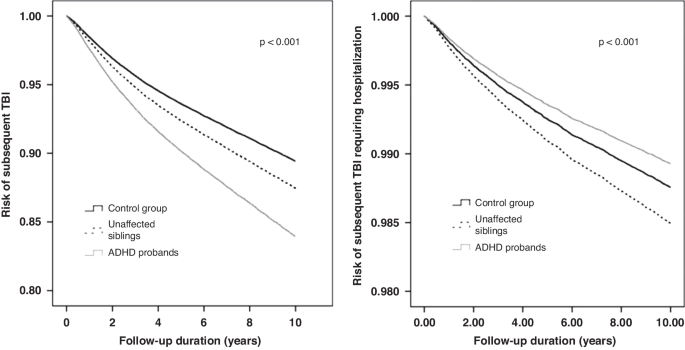
ADHD attention deficit hyperactivity disorder, TBI traumatic brain injury.
Finally, the long-term use of ADHD medications may slightly reduce the risk of any TBI occurrence (HR: 1.44, 95% CI: 1.30–1.60) during the follow-up compared with the short-term use (1.59, 1.53–1.65) among patients with ADHD (Table 2 ).
The results of this large-scale, population-based study supported the hypothesis that ADHD probands had the highest risk of subsequent TBI during the follow-up period, followed by unaffected siblings and healthy controls. In addition, we observed a counter-intuitive result that unaffected siblings had a higher risk of TBI requiring hospitalization than did healthy controls, whereas ADHD probands had a lower risk than controls. Furthermore, our findings suggest that the use of ADHD medications may reduce the risk of subsequent TBI requiring hospitalization, and the results demonstrated an earlier mean age at TBI diagnosis in ADHD probands and unaffected siblings than in controls.
As mentioned in the introduction, the potential relationship between ADHD and TBI has been suggested in several studies. 21 , 22 , 23 However, a meta-analysis comprising 3023 mild TBI patients and 9,716 controls revealed a significant association between ADHD and mild TBI, and the association was significant in studies that have reported on ADHD subsequent to mild TBI, but not in studies that have reported mild TBI subsequent to ADHD. 33 As TBI can exacerbate attention and impulsivity problems, 34 the relationship between ADHD and TBI could become bidirectional and complicated. Moreover, both ADHD and TBI are associated with a wide range of negative outcomes; thus, clarifying the temporal association is essential for developing effective prevention and treatment measures. In a prospective longitudinal study that examined the TBI diagnosis records of 628 male patients from birth to the age of 34 years, Guberman et al. discovered that childhood inattention-hyperactivity assessed using teacher rating scales was significantly associated with an increased risk of TBI from the ages of 11–34 years. 35 Asarnow et al. conducted a meta-analysis of 12,374 patients with TBI of all severity levels and 43,491 controls and reported that 16.0% of patients with TBI presented with ADHD before brain injury; the prevalence of severe TBI was considerably higher than that of 10.8% reported for the general population. 36 As increasing studies have supported the relationship between ADHD and subsequent TBI, 21 , 22 , 23 , 35 , 36 our study discovered a similar mean duration of 4.56 years between study enrollment and subsequent TBI development among ADHD patients. Therefore, because ADHD appears to be a risk factor for TBI, more attention should be paid to this high-risk population. Although studying whether TBI is a risk factor for ADHD is a crucial topic, it is not addressed in this study.
According to previous studies that have assessed ADHD patients, unaffected siblings of ADHD probands, and healthy controls using psychiatric interviews and different executive function tasks, unaffected siblings of ADHD probands may exhibit a common endophenotype with their ADHD siblings, and they may also exhibit some deficits in a wide range of neuropsychological functions. 9 , 10 , 11 , 12 , 13 In addition, several neuroimaging studies have examined neuroanatomical abnormalities in ADHD patients and their unaffected siblings. 10 , 37 , 38 , 39 , 40 Pironti et al. found an abnormal decrease in the gray matter volume in the right inferior frontal gyrus and an abnormal increase in the white matter volume in the caudal portion of the right inferior fronto-occipital fasciculus among ADHD patients and their unaffected first-degree relatives. 10 Hoogman et al. compared unaffected siblings with healthy controls and demonstrated shared familial effects by showing a significantly smaller surface area in the caudal middle frontal, lateral orbital frontal, and superior frontal gyrus in unaffected siblings. 37 Chiang et al. reported increased functional connectivity in the left insula and left inferior frontal gyrus among both ADHD probands and unaffected siblings compared with controls. 38 These studies have provided evidence that neural profiles are shared between ADHD patients and their unaffected siblings, and the results suggest that some of the shared neuroanatomical abnormalities may be associated with the severity of ADHD symptoms in unaffected siblings. 37 , 40 To summarize, neuropsychological and neuroanatomical abnormalities found in ADHD probands and unaffected siblings may lead to the partial expression of ADHD symptoms and further adversely affect their subsequent mental and physical health. 6 , 7 , 24 Although the relationship between ADHD and TBI has been examined in previous research, 21 , 22 , 23 , 33 , 35 , 36 the association between TBI and unaffected siblings of ADHD probands has been rarely discussed. Wei et al. reported that unaffected siblings of ADHD probands were more likely to develop TBI (OR: 1.24, 95% CI: 1.14–1.36) than controls. 24 Our study data also revealed this finding. Consequently, unaffected siblings and ADHD probands appear to be a high-risk population for TBI; thus, increasing the awareness of the increased TBI risk for their families and caregivers is warranted.
The severity of TBI has often been considered when exploring the relationship between TBI and subsequent ADHD. 33 , 36 , 41 However, fewer studies have considered the severity of TBI because more studies are focusing on the association between ADHD and subsequent TBI development. In this study, we also considered the severity of TBI by identifying TBI requiring hospitalization. The results revealed that when compared with controls, unaffected siblings were at a higher risk of TBI requiring hospitalization, whereas ADHD probands were at a lower risk. By using the German Pharmacoepidemiological Research Database, Lindemann et al. performed a large-scale retrospective cohort study to assess the risk of hospitalization due to injury diagnoses in children and adolescents with newly diagnosed ADHD compared with those without ADHD, 42 and the results were different from our findings. Moreover, they reported that the incidence of TBI hospitalization was 1.87% (95% CI: 1.71–2.04) in male ADHD patients, 1.32% (95% CI: 1.19–1.47) in male controls, 1.38% (95% CI: 1.15–1.65) in female ADHD patients, and 0.91% (95% CI: 0.73–1.13) in female controls, with an increased adjusted HR of TBI hospitalization for patients with ADHD compared with those without. By contrast, our study reported that the incidence of TBI requiring hospitalization was 1.1% in ADHD patients and 1.3% in healthy controls, with a decreased adjusted HR of TBI requiring hospitalization for ADHD probands compared with controls. To explain the differences, we proposed the following possible reasons. The differences may be attributed to some biological, psychological, and sociological factors that were not investigated but could influence the incidence rates. For instance, Lindemann et al. did not consider the ADHD medication treatment as a possible protective factor against TBI in ADHD patients; however, the factor was discussed further in the study. Consequently, the results are potentially confounded by the fraction of patients receiving ADHD medications. In addition, other unmeasured potential prognostic factors, such as socioeconomic status, psychological stress, and environmental safety, may influence the results and contribute to the differences. Due to the limited relevant literature, further studies are required to reveal more details. Moreover, our study discovered a counter-intuitive and surprising result that ADHD probands had a decreased risk of TBI requiring hospitalization compared with healthy controls, which might be because ADHD probands may be in a safer setting, be under more protection, and receive more care from caregivers given their diagnosis of ADHD than other healthy individuals. The aforementioned reasons may also explain our finding of the longest duration between enrollment and TBI occurrence in the ADHD probands compared with the other two groups. Nevertheless, these measures to prevent ADHD patients from physical injuries have some limitations because of the increased TBI risk among ADHD patients shown in this study, but they may play an important role in reducing their risk of TBI hospitalization. The beneficial effect of the use of ADHD medications on subsequent TBI requiring hospitalization could also explain the difference. However, the result should be interpreted with caution, and further studies are needed to confirm the hypothesis. Additionally, our study reported that the unaffected siblings of ADHD probands were more likely to develop both TBI and TBI requiring hospitalization than healthy controls. Hence, we recommend that more attention be paid to preventing subsequent TBI development in this population.
Previous studies have revealed that ADHD medications are related to decreases in the risks of a wide range of ADHD-associated functional outcomes, including TBI and accidents and injuries. 23 , 43 , 44 , 45 , 46 , 47 Mikolajczyk et al. demonstrated a 34% risk reduction for hospitalization due to brain injury diagnoses during the periods with ADHD medication compared with nonmedicated periods. 45 Liou et al. examined 72,181 ADHD patients and 72,181 age-and sex-matched non-ADHD controls and reported the association between the long-term use of ADHD medications and a reduced risk of subsequent TBI. 23 Boland et al. conducted a meta-analysis of 21 studies in 2020 and revealed a robust protective effect of ADHD medications on academic outcomes, accidents and injuries, and mood disorders, along with a statistically insignificant protective effect on TBI. 46 More recently, Brunkhorst-Kanaan et al. conducted a systematic review and suggested that stimulant medication appeared to be effective for injury prevention in ADHD patients over their lifespan. 47 Compatible with the results of previous studies, our study results suggest that the use of ADHD medications may reduce the risk of subsequent TBI requiring hospitalization. Therefore, early diagnosis and optimal treatment for individuals with ADHD are critical in clinical practice to minimize the risk of subsequent TBI requiring hospitalization. In addition, further well-designed clinical studies may be needed to quantify the protective effects of ADHD medications on subsequent TBI risk.
Age at TBI diagnosis may influence neurocognitive, academic, and behavior outcomes following TBI and is a topic worth exploring. 48 , 49 , 50 , 51 , 52 , 53 However, previous studies have reported mixed results. Some studies have supported the theory of neuroplasticity describing that children injured at an earlier age have better outcomes due to the ability for neuronal circuits in the young brain to undergo adaptive changes on structural and functional levels, 51 , 52 whereas other studies have supported the theory of vulnerability stating that children injured at an earlier age have poorer outcomes because of the incomplete development of the brain after TBI. 48 , 49 , 50 , 53 The impact of age at TBI diagnosis on the results is difficult to assess because of the increasing difficulty of detecting neurocognitive impairments in younger children, the lack of large-scale studies, and variations in the distribution of age categories and the timing of follow-up evaluations in various studies. 54 , 55 In this study, we collected a wide range of demographic data on age at TBI diagnosis from a considerably large-sized sample. In addition, we observed an earlier mean age at TBI diagnosis in ADHD probands and unaffected siblings compared with controls. However, the impact of age at injury on outcomes following TBI remains controversial; therefore, further studies are necessary to corroborate this finding.
However, this study has several limitations. First, the incidence of TBI and TBI requiring hospitalization may have been underestimated because only those who seek medical help are registered in the NHIRD. Second, information on the severity of ADHD and TBI is unavailable in the NHIRD. Therefore, we did not account for the severity of ADHD and identified TBI requiring hospitalization as an alternative way to assess the severity of TBI. Further studies would be required to clarify the association of ADHD diagnosis and trait with the exact severity, which was defined by the TBI neuroimaging criteria and Glasgow Coma Scale, of TBI. Finally, because the NHIRD does not provide information on factors such as psychosocial stress, family relationships, personal lifestyle, and environment, we could not explore their influence. Therefore, these limitations should be considered when interpreting the results.
In conclusion, this large-scale, population-based study suggested that ADHD probands had the highest risk of subsequent TBI, followed by their unaffected siblings and controls. We also found that unaffected siblings had a higher risk of TBI requiring hospitalization than controls, whereas ADHD probands had a lower risk. Hence, we recommend that more attention should be paid in order to prevent subsequent TBI development in the unaffected siblings of ADHD probands. In addition, this study demonstrated that the use of ADHD medications may reduce the risk of subsequent TBI requiring hospitalization, which supports the importance of early diagnosis and optimal treatment for individuals with ADHD.
Data availability
The NHIRD was released and audited by the Department of Health and Bureau of the NHI Program for the purpose of scientific research ( https://www.apre.mohw.gov.tw/ ). The NHIRD can be accessed through a formal application that is regulated by the Health and Welfare Data Science Center of Ministry of Health and Welfare, Taiwan.
Xu, G., Strathearn, L., Liu, B., Yang, B. & Bao, W. Twenty-year trends in diagnosed attention-deficit/hyperactivity disorder among US children and adolescents, 1997–2016. JAMA Netw. Open 1 , e181471–e181471 (2018).
Article PubMed PubMed Central Google Scholar
Li, Y. et al. Prevalence and trends in diagnosed ADHD among US children and adolescents, 2017–2022. JAMA Netw. Open 6 , e2336872–e2336872 (2023).
Sayal, K., Prasad, V., Daley, D., Ford, T. & Coghill, D. ADHD in children and young people: Prevalence, care pathways, and service provision. Lancet Psychiatry 5 , 175–186 (2018).
Article PubMed Google Scholar
Asherson, P., Buitelaar, J., Faraone, S. V. & Rohde, L. A. Adult attention-deficit hyperactivity disorder: Key conceptual issues. Lancet Psychiatry 3 , 568–578 (2016).
Feldman, H. M. & Reiff, M. I. Attention deficit–hyperactivity disorder in children and adolescents. N. Engl. J. Med. 370 , 838–846 (2014).
Article CAS PubMed Google Scholar
Rappley, M. D. Attention deficit–hyperactivity disorder. N. Engl. J. Med. 352 , 165–173 (2005).
Biederman, J. & Faraone, S. V. Attention-deficit hyperactivity disorder. Lancet 366 , 237–248 (2005).
Chen, M. H. et al. Sexually transmitted infection among adolescents and young adults with attention-deficit/hyperactivity disorder: A nationwide longitudinal study. J. Am. Acad. Child Adolesc. Psychiatry 57 , 48–53 (2018).
Gau, S. S. & Huang, W. L. Rapid visual information processing as a cognitive endophenotype of attention deficit hyperactivity disorder. Psychol. Med. 44 , 435–446 (2014).
Pironti, V. A. et al. Neuroanatomical abnormalities and cognitive impairments are shared by adults with attention-deficit/hyperactivity disorder and their unaffected first-degree relatives. Biol. Psychiatry 76 , 639–647 (2014).
Gau, S. S. & Shang, C. Y. Executive functions as endophenotypes in ADHD: evidence from the Cambridge Neuropsychological Test Battery (CANTAB). J. Child Psychol. Psychiatry 51 , 838–849 (2010).
Oerlemans, A. M. et al. Cognitive impairments are different in single-incidence and multi-incidence ADHD families. J. Child Psychol. Psychiatry 56 , 782–791 (2015).
van Dongen, E. V. et al. Distinct effects of ASD and ADHD symptoms on reward anticipation in participants with ADHD, their unaffected siblings and healthy controls: a cross-sectional study. Mol. Autism 6 , 48 (2015).
Yang, L. K., Shang, C. Y. & Gau, S. S. Psychiatric comorbidities in adolescents with attention-deficit hyperactivity disorder and their siblings. Can. J. Psychiatry 56 , 281–292 (2011).
Hyder, A. A., Wunderlich, C. A., Puvanachandra, P., Gururaj, G. & Kobusingye, O. C. The impact of traumatic brain injuries: a global perspective. NeuroRehabilitation 22 , 341–353 (2007).
Consensus conference. Rehabilitation of persons with traumatic brain injury. NIH Consensus Development Panel on Rehabilitation of Persons With Traumatic Brain Injury. JAMA 282 , 974–983 (1999).
Article Google Scholar
Feigin, V. L. et al. Incidence of traumatic brain injury in New Zealand: a population-based study. Lancet Neurol. 12 , 53–64 (2013).
Traumatic brain injury: time to end the silence. Lancet Neurol 9 , 331 (2010).
Nguyen, R. et al. The international incidence of traumatic brain injury: A systematic review and meta-analysis. Can. J. Neurol. Sci. 43 , 774–785 (2016).
Global, regional, and national burden of traumatic brain injury and spinal cord injury, 1990-2016: a systematic analysis for the Global Burden of Disease Study 2016. Lancet Neurol. 18 , 56–87 (2019).
Ilie, G. et al. The association between traumatic brain injury and ADHD in a Canadian adult sample. J. Psychiatr. Res. 69 , 174–179 (2015).
Biederman, J. et al. Mild traumatic brain injury and attention-deficit hyperactivity disorder in young student athletes. J. Nerv. Ment. Dis. 203 , 813–819 (2015).
Liou, Y. J. et al. Risk of traumatic brain injury among children, adolescents, and young adults with attention-deficit hyperactivity disorder in Taiwan. J. Adolesc. Health.: Off. Publ. Soc. Adolesc. Med. 63 , 233–238 (2018).
Wei, H. T. et al. Risks of bipolar disorder, depressive disorder, and traumatic brain injury among siblings of patients with attention-deficit hyperactivity disorder. J. Affect. Disord. 245 , 335–339 (2019).
Chen, M. H. et al. Risk and coaggregation of major psychiatric disorders among first-degree relatives of patients with bipolar disorder: a nationwide population-based study. Psychol. Med. 49 , 2397–2404 (2019).
Chen, M. H. et al. Risk of developing type 2 diabetes in adolescents and young adults with autism spectrum disorder: A nationwide longitudinal study. Diabetes Care 39 , 788–793 (2016).
Cheng, C. M. et al. Co-aggregation of major psychiatric disorders in individuals with first-degree relatives with schizophrenia: a nationwide population-based study. Mol. Psychiatry 23 , 1756–1763 (2018).
Huang, M. H. et al. Familial coaggregation of major psychiatric disorders among first-degree relatives of patients with obsessive-compulsive disorder: a nationwide study. Psychol. Med. 51 , 680–687 (2021).
Mulder, M. J. et al. Familial vulnerability to ADHD affects activity in the cerebellum in addition to the prefrontal systems. J. Am. Acad. Child Adolesc. Psychiatry 47 , 68–75 (2008).
van Rooij, D. et al. Altered neural connectivity during response inhibition in adolescents with attention-deficit/hyperactivity disorder and their unaffected siblings. Neuroimage: Clin. 7 , 325–335 (2015).
van Rooij, D. et al. Distinguishing adolescents with ADHD from their unaffected siblings and healthy comparison subjects by neural activation patterns during response inhibition. Am. J. Psychiatry 172 , 674–683 (2015).
Liu, C.-Y. et al. Incorporating development stratification of Taiwan townships into sampling design of large scale health interview survey. J. Health Manag 4 , 1–22 (2006).
CAS Google Scholar
Adeyemo, B. O. et al. Mild traumatic brain injury and ADHD: a systematic review of the literature and meta-analysis. J. Atten. Disord. 18 , 576–584 (2014).
Yeates, K. O. et al. Long-term attention problems in children with traumatic brain injury. J. Am. Acad. Child Adolesc. Psychiatry 44 , 574–584 (2005).
Guberman, G. I. et al. A prospective study of childhood predictors of traumatic brain injuries sustained in adolescence and adulthood. Can. J. Psychiatry 65 , 36–45 (2020).
Asarnow, R. F., Newman, N., Weiss, R. E. & Su, E. Association of attention-deficit/hyperactivity disorder diagnoses with pediatric traumatic brain injury: A meta-analysis. JAMA Pediatr. 175 , 1009–1016 (2021).
Hoogman, M. et al. Brain imaging of the cortex in ADHD: a coordinated analysis of large-scale clinical and population-based samples. Am. J. Psychiatry 176 , 531–542 (2019).
Chiang, H.-L., Tseng, W.-Y. I., Wey, H.-Y. & Gau, S. S.-F. Shared intrinsic functional connectivity alterations as a familial risk marker for ADHD: a resting-state functional magnetic resonance imaging study with sibling design. Psychol. Med. 52 , 1736–1745 (2022).
Durston, S. et al. Magnetic resonance imaging of boys with attention-deficit/hyperactivity disorder and their unaffected siblings. J. Am. Acad. Child Adolesc. Psychiatry 43 , 332–340 (2004).
Bralten, J. et al. Voxel-based morphometry analysis reveals frontal brain differences in participants with ADHD and their unaffected siblings. J. Psychiatry Neurosci. 41 , 272–279 (2016).
Chang, H.-K. et al. Traumatic brain injury in early childhood and risk of attention-deficit/hyperactivity disorder and autism spectrum disorder: a nationwide longitudinal study. J. Clin. Psychiatry 79 , 21226 (2018).
Lindemann, C., Langner, I., Banaschewski, T., Garbe, E. & Mikolajczyk, R. T. The risk of hospitalizations with injury diagnoses in a matched cohort of children and adolescents with and without attention deficit/hyperactivity disorder in Germany: a database study. Front. Pediatr. 5 , 220 (2017).
Man, K. K. et al. Methylphenidate and the risk of trauma. Pediatrics 135 , 40–48 (2015).
Gobbo, M. A. & Louzã, M. R. Influence of stimulant and non-stimulant drug treatment on driving performance in patients with attention deficit hyperactivity disorder: a systematic review. Eur. Neuropsychopharmacol. 24 , 1425–1443 (2014).
Mikolajczyk, R. et al. Injury prevention by medication among children with attention-deficit/hyperactivity disorder: a case-only study. JAMA Pediatr. 169 , 391–395 (2015).
Boland, H. et al. A literature review and meta-analysis on the effects of ADHD medications on functional outcomes. J. Psychiatr. Res. 123 , 21–30 (2020).
Brunkhorst-Kanaan, N. et al. ADHD and accidents over the life span–A systematic review. Neurosci. Biobehav. Rev. 125 , 582–591 (2021).
Karver, C. L. et al. Age at injury and long-term behavior problems after traumatic brain injury in young children. Rehab. Psychol. 57 , 256 (2012).
Keenan, H. T., Clark, A. E., Holubkov, R., Cox, C. S. & Ewing-Cobbs, L. Psychosocial and executive function recovery trajectories one year after pediatric traumatic brain injury: the influence of age and injury severity. J. Neurotrauma 35 , 286–296 (2018).
Rostami, E., Figaji, A. & Adelson, P. D. Pediatric TBI-current state of the art and future perspective. Front. Neurol. 12 , 649676 (2021).
Andruszkow, H. et al. Physical and psychological long-term outcome after traumatic brain injury in children and adult patients. Health Qual. Life Outcomes 12 , 1–8 (2014).
Krasny-Pacini, A. et al. Executive function after severe childhood traumatic brain injury–Age-at-injury vulnerability periods: The TGE prospective longitudinal study. Ann. Phys. Rehab. Med. 60 , 74–82 (2017).
Crowe, L. M., Catroppa, C., Babl, F. E., Rosenfeld, J. V. & Anderson, V. Timing of traumatic brain injury in childhood and intellectual outcome. J. Pediatr. Psychol. 37 , 745–754 (2012).
Li, L. & Liu, J. The effect of pediatric traumatic brain injury on behavioral outcomes: a systematic review. Dev. Med. Child Neurol. 55 , 37–45 (2013).
Au, A. K. & Clark, R. S. Paediatric traumatic brain injury: Prognostic insights and outlooks. Curr. Opin. Neurol. 30 , 565–572 (2017).
Download references
Acknowledgements
We thank Mr. I-Fan Hu, MA (Courtauld Institute of Art, University of London; National Taiwan University) for his friendship and support. Mr. Hu declares no conflicts of interest.
The study was supported by grant from Taipei Veterans General Hospital (V111C-010, V111C-040, V111C-029), Yen Tjing Ling Medical Foundation (CI-109-21, CI-109-22, CI-110-30) and Ministry of Science and Technology, Taiwan (MOST110-2314-B-075-026, MOST110-2314-B-075-024 -MY3, MOST 109-2314-B-010-050-MY3, MOST111-2314-B-075 -014 -MY2, MOST 111-2314-B-075 -013). The funding source had no role in any process of our study. Open Access funding enabled and organized by National Yang Ming Chiao Tung University.
Author information
Authors and affiliations.
Department of Medical Education, Taipei Veterans General Hospital, Taipei, Taiwan
Ping-Chung Wu
Department of Psychiatry, College of Medicine, National Yang Ming Chiao Tung University, Taipei, Taiwan
Ping-Chung Wu, Shih-Jen Tsai, Ju-Wei Hsu, Kai-Lin Huang & Mu-Hong Chen
Department of Psychiatry, Taipei Veterans General Hospital, Taipei, Taiwan
Shih-Jen Tsai, Ju-Wei Hsu, Kai-Lin Huang & Mu-Hong Chen
Department of Family Medicine, Taipei Veterans General Hospital, Taipei, Taiwan
Tzeng-Ji Chen
Institute of Hospital and Health Care Administration, National Yang Ming Chiao Tung University, Taipei, Taiwan
Department of Family Medicine, Taipei Veterans General Hospital, Hsinchu Branch, Hsinchu, Taiwan
School of Traditional Chinese Medicine, Chang Gung University, Taoyuan, Taiwan
Tai-Long Pan
Research Center for Chinese Herbal Medicine and Research Center for Food and Cosmetic Safety, College of Human Ecology, Chang Gung University of Science and Technology, Taoyuan, Taiwan
Liver Research Center, Chang Gung Memorial Hospital, Taoyuan, Taiwan
You can also search for this author in PubMed Google Scholar
Contributions
Drs MHC, TLP and SJT designed the study; Drs MHC and PCW drafted the manuscript; Dr MHC analyzed the data; Drs JWH, KLH, and TJC reviewed the literature and critically reviewed the manuscript. All authors contributed substantially to the manuscript, and approved the final manuscript for submission. All authors are responsible for the integrity, accuracy and presentation of the data.
Corresponding authors
Correspondence to Tai-Long Pan or Mu-Hong Chen .
Ethics declarations
Competing interests.
The authors declare no competing interests.
Statement regarding the patient consent
Institutional Review Board of Taipei Veterans General Hospital approved the study protocol and waived the requirement for informed consent since this investigation used de-identified data and no human subjects contact was required.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ .
Reprints and permissions
About this article
Cite this article.
Wu, PC., Tsai, SJ., Hsu, JW. et al. Risk of traumatic brain injury among patients with ADHD and their unaffected siblings. Pediatr Res (2024). https://doi.org/10.1038/s41390-024-03233-0
Download citation
Received : 16 January 2024
Revised : 31 March 2024
Accepted : 09 April 2024
Published : 07 May 2024
DOI : https://doi.org/10.1038/s41390-024-03233-0
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
Quick links
- Explore articles by subject
- Guide to authors
- Editorial policies
- Share full article
Advertisement
Supported by
Doctors Are Still Figuring Out Adult A.D.H.D.
It’s one of the most common psychiatric disorders in adults. Yet there are no U.S. guidelines for diagnosing and treating patients beyond childhood.

By Christina Caron
Just before Katie Marsh dropped out of college, she began to worry that she might have attention deficit hyperactivity disorder.
“Boredom was like a burning sensation inside of me,” said Ms. Marsh, who is now 30 and lives in Portland, Ore. “I barely went to class. And when I did, I felt like I had a lot of pent-up energy. Like I had to just move around all the time.”
So she asked for an A.D.H.D. evaluation — but the results, she was surprised to learn, were inconclusive. She never did return to school. And only after seeking help again four years later was she diagnosed by an A.D.H.D. specialist.
“It was pretty frustrating,” she said.
A.D.H.D. is one of the most common psychiatric disorders in adults. Yet many health care providers have uneven training on how to evaluate it, and there are no U.S. clinical practice guidelines for diagnosing and treating patients beyond childhood.
Without clear rules, some providers, while well-intentioned, are just “making it up as they go along,” said Dr. David W. Goodman, an assistant professor of psychiatry and behavioral sciences at the Johns Hopkins University School of Medicine.
This lack of clarity leaves providers and adult patients in a bind.
“We desperately need something to help guide the field,” said Dr. Wendi Waits, a psychiatrist with Talkiatry, an online mental health company. “When everyone’s practicing somewhat differently, it makes it hard to know how best to approach it.”
Can A.D.H.D. symptoms emerge in adulthood?
A.D.H.D. is defined as a neurodevelopmental disorder that begins in childhood and is typically characterized by inattention, disorganization, hyperactivity and impulsivity. Patients are generally categorized into three types: hyperactive and impulsive, inattentive, or a combination of the two.
The latest data suggest that about 11 percent of children ages 5 to 17 in the United States have been diagnosed with A.D.H.D. And about 4 percent of adults are estimated to have the disorder. But as recently as two decades ago, most mental health providers “didn’t really believe in adult A.D.H.D.,” Dr. Goodman said.
Now, for the most part, that’s no longer the case. And during the pandemic, stimulant prescriptions, primarily used to treat A.D.H.D., “sharply increased,” particularly among young adults and women, according to a study published in JAMA Psychiatry in January.
When diagnosing the condition, providers rely on the D.S.M.-5., the American Psychiatric Association’s official manual of mental disorders, which contains a somewhat arbitrary requirement: In order to meet the diagnostic criteria for A.D.H.D., significant symptoms, such as continual forgetfulness and talking out of turn, should be present in at least two settings before age 12.
But sometimes, older patients either do not recall childhood symptoms or say that those symptoms were mild. Judy Sandler, 62, who lives in Lincolnville, Maine , was not diagnosed with A.D.H.D. until her mid-50s, after retiring from her job as a teacher: It was the first time in her life she felt like she couldn’t get anything done. She wanted to write, but when she would sit down to focus, she immediately had the urge to get up and do something else: “I’ll just do the laundry,” she would think. “And then go walk the dog.”
During her working years, she benefited from a “hyper-structured” schedule — up until retirement. “All of a sudden, I felt like the rug had been pulled out,” she said.
Patients like Ms. Sandler fall into a gray area. She did not recall having significant symptoms in school or at home, rather she indicated that her symptoms became most problematic later in life. Her husband of 33 years, however, had noticed symptoms for years: She was often forgetful, for example, and found it challenging to slow down.
“There’s a lot more subtlety in making this diagnosis — especially in high-functioning, bright people — than just a symptom checklist,” Dr. Goodman said.
Is the D.S.M. missing symptoms?
The D.S.M. lists nine symptoms of inattention and nine symptoms of impulsivity-hyperactivity that are used to evaluate whether an adult or a child has A.D.H.D.
The D.S.M. does not formally include symptoms related to emotional dysregulation, which is when someone has difficulty managing their mood. It also does not officially mention deficits of executive functioning, or problems with planning, organization and self-regulation. But studies have found that these are some of the most common symptoms that adults with A.D.H.D. experience, said Russell Ramsay, a psychologist who treats adult A.D.H.D.
When the D.S.M.-5 was published in 2013, there was not enough high-quality research to support the addition of these symptoms, Dr. Goodman said. But experts say they are still useful to consider when assessing someone.
Dr. Goodman is working with Dr. Ramsay and other A.D.H.D. specialists from around the world to develop the first U.S. guidelines for diagnosing and treating adults with A.D.H.D., in collaboration with the American Professional Society of A.D.H.D. and Related Disorders.
There is an urgency to do so, in part because of new research that has emerged in the last decade. In addition, while adult A.D.H.D . is often undiagnosed and untreated, some people might be getting diagnosed who don’t actually have the disorder — and given medication they don’t truly need, Dr. Goodman said.
The new guidelines, which are expected to be available for public comment later this year, will aim to create a more uniform process for diagnosing adults, but the D.S.M. will continue to be the “gold standard” for providers, Dr. Ramsay said.
“It’s not wrong,” he added. “It’s just incomplete.”
Is it A.D.H.D or something else?
For adults, a proper A.D.H.D. diagnosis typically requires several steps: an interview with the patient, a medical and developmental history, symptom questionnaires and, if possible, conversations with other people in the patient’s life, like a spouse.
“There are no shortcuts,” said Dr. Lenard A. Adler, a professor of psychiatry at the N.Y.U. Grossman School of Medicine, while speaking to hundreds of providers at the American Psychiatric Association conference in early May. “This isn’t easy.”
While everybody has some trouble paying attention or is restless from time to time, he added, it’s really how pervasive and significant the symptoms are and how consistent and impairing they’ve been throughout the patient’s life that helps doctors decide if an A.D.H.D. diagnosis is appropriate.
But several factors can make it tricky.
People who consider themselves heavy users of digital technology are more likely to report A.D.H.D. symptoms, research suggests .
There’s a “chicken or the egg” dilemma, Dr. Waits said. Are people with A.D.H.D. drawn to using digital technology more than the average person? Or did their A.D.H.D. develop because of their technology use?
People with A.D.H.D. are also likely to have another coexisting condition , like substance use disorder, depression or anxiety, which can make it challenging for both doctors and patients to understand if their symptoms are a result of A.D.H.D., particularly if the symptoms overlap.
Ms. Marsh, who had been diagnosed with depression as a teenager and took up to 10 different medications to treat it without much success, finally received an A.D.H.D. diagnosis after visiting a psychologist in her hometown. This time, the practitioner took the time to talk with her parents and her partner, and then did a fresh analysis of the test results that had been deemed inconclusive four years earlier.
After Ms. Marsh began therapy and started taking the stimulant Focalin, the difference in how she felt was “insane,” she said. Her depression improved as well.
“I could keep track of things in my brain easier,” she added. “I’ve just been able to do a lot more things because I have the motivation for it.”
Christina Caron is a Times reporter covering mental health. More about Christina Caron
Understanding A.D.H.D.
The challenges faced by those with attention deficit hyperactivity disorder can be daunting. but people who are diagnosed with it can still thrive..
Millions of children in the United States have received a diagnosis of A.D.H.D . Here is how their families can support them .
The condition is also being recognized more in adults . These are some of the behaviors that might be associated with adult A.D.H.D.
Since a nationwide Adderall shortage started, some people with A.D.H.D. have said their medication no longer helps with their symptoms. But there could be other factors at play .
Everyone has bouts of distraction and forgetfulness. Here is when psychiatrists diagnose it as something clinical .
The disorder can put a strain on relationships. But there are ways to cope .
Though meditation can be beneficial to those with A.D.H.D., sitting still and focusing on breathing can be hard for them. These tips can help .
- Open access
- Published: 14 May 2024
Developing a survey to measure nursing students’ knowledge, attitudes and beliefs, influences, and willingness to be involved in Medical Assistance in Dying (MAiD): a mixed method modified e-Delphi study
- Jocelyn Schroeder 1 ,
- Barbara Pesut 1 , 2 ,
- Lise Olsen 2 ,
- Nelly D. Oelke 2 &
- Helen Sharp 2
BMC Nursing volume 23 , Article number: 326 ( 2024 ) Cite this article
181 Accesses
Metrics details
Medical Assistance in Dying (MAiD) was legalized in Canada in 2016. Canada’s legislation is the first to permit Nurse Practitioners (NP) to serve as independent MAiD assessors and providers. Registered Nurses’ (RN) also have important roles in MAiD that include MAiD care coordination; client and family teaching and support, MAiD procedural quality; healthcare provider and public education; and bereavement care for family. Nurses have a right under the law to conscientious objection to participating in MAiD. Therefore, it is essential to prepare nurses in their entry-level education for the practice implications and moral complexities inherent in this practice. Knowing what nursing students think about MAiD is a critical first step. Therefore, the purpose of this study was to develop a survey to measure nursing students’ knowledge, attitudes and beliefs, influences, and willingness to be involved in MAiD in the Canadian context.
The design was a mixed-method, modified e-Delphi method that entailed item generation from the literature, item refinement through a 2 round survey of an expert faculty panel, and item validation through a cognitive focus group interview with nursing students. The settings were a University located in an urban area and a College located in a rural area in Western Canada.
During phase 1, a 56-item survey was developed from existing literature that included demographic items and items designed to measure experience with death and dying (including MAiD), education and preparation, attitudes and beliefs, influences on those beliefs, and anticipated future involvement. During phase 2, an expert faculty panel reviewed, modified, and prioritized the items yielding 51 items. During phase 3, a sample of nursing students further evaluated and modified the language in the survey to aid readability and comprehension. The final survey consists of 45 items including 4 case studies.
Systematic evaluation of knowledge-to-date coupled with stakeholder perspectives supports robust survey design. This study yielded a survey to assess nursing students’ attitudes toward MAiD in a Canadian context.
The survey is appropriate for use in education and research to measure knowledge and attitudes about MAiD among nurse trainees and can be a helpful step in preparing nursing students for entry-level practice.
Peer Review reports
Medical Assistance in Dying (MAiD) is permitted under an amendment to Canada’s Criminal Code which was passed in 2016 [ 1 ]. MAiD is defined in the legislation as both self-administered and clinician-administered medication for the purpose of causing death. In the 2016 Bill C-14 legislation one of the eligibility criteria was that an applicant for MAiD must have a reasonably foreseeable natural death although this term was not defined. It was left to the clinical judgement of MAiD assessors and providers to determine the time frame that constitutes reasonably foreseeable [ 2 ]. However, in 2021 under Bill C-7, the eligibility criteria for MAiD were changed to allow individuals with irreversible medical conditions, declining health, and suffering, but whose natural death was not reasonably foreseeable, to receive MAiD [ 3 ]. This population of MAiD applicants are referred to as Track 2 MAiD (those whose natural death is foreseeable are referred to as Track 1). Track 2 applicants are subject to additional safeguards under the 2021 C-7 legislation.
Three additional proposed changes to the legislation have been extensively studied by Canadian Expert Panels (Council of Canadian Academics [CCA]) [ 4 , 5 , 6 ] First, under the legislation that defines Track 2, individuals with mental disease as their sole underlying medical condition may apply for MAiD, but implementation of this practice is embargoed until March 2027 [ 4 ]. Second, there is consideration of allowing MAiD to be implemented through advanced consent. This would make it possible for persons living with dementia to receive MAID after they have lost the capacity to consent to the procedure [ 5 ]. Third, there is consideration of extending MAiD to mature minors. A mature minor is defined as “a person under the age of majority…and who has the capacity to understand and appreciate the nature and consequences of a decision” ([ 6 ] p. 5). In summary, since the legalization of MAiD in 2016 the eligibility criteria and safeguards have evolved significantly with consequent implications for nurses and nursing care. Further, the number of Canadians who access MAiD shows steady increases since 2016 [ 7 ] and it is expected that these increases will continue in the foreseeable future.
Nurses have been integral to MAiD care in the Canadian context. While other countries such as Belgium and the Netherlands also permit euthanasia, Canada is the first country to allow Nurse Practitioners (Registered Nurses with additional preparation typically achieved at the graduate level) to act independently as assessors and providers of MAiD [ 1 ]. Although the role of Registered Nurses (RNs) in MAiD is not defined in federal legislation, it has been addressed at the provincial/territorial-level with variability in scope of practice by region [ 8 , 9 ]. For example, there are differences with respect to the obligation of the nurse to provide information to patients about MAiD, and to the degree that nurses are expected to ensure that patient eligibility criteria and safeguards are met prior to their participation [ 10 ]. Studies conducted in the Canadian context indicate that RNs perform essential roles in MAiD care coordination; client and family teaching and support; MAiD procedural quality; healthcare provider and public education; and bereavement care for family [ 9 , 11 ]. Nurse practitioners and RNs are integral to a robust MAiD care system in Canada and hence need to be well-prepared for their role [ 12 ].
Previous studies have found that end of life care, and MAiD specifically, raise complex moral and ethical issues for nurses [ 13 , 14 , 15 , 16 ]. The knowledge, attitudes, and beliefs of nurses are important across practice settings because nurses have consistent, ongoing, and direct contact with patients who experience chronic or life-limiting health conditions. Canadian studies exploring nurses’ moral and ethical decision-making in relation to MAiD reveal that although some nurses are clear in their support for, or opposition to, MAiD, others are unclear on what they believe to be good and right [ 14 ]. Empirical findings suggest that nurses go through a period of moral sense-making that is often informed by their family, peers, and initial experiences with MAID [ 17 , 18 ]. Canadian legislation and policy specifies that nurses are not required to participate in MAiD and may recuse themselves as conscientious objectors with appropriate steps to ensure ongoing and safe care of patients [ 1 , 19 ]. However, with so many nurses having to reflect on and make sense of their moral position, it is essential that they are given adequate time and preparation to make an informed and thoughtful decision before they participate in a MAID death [ 20 , 21 ].
It is well established that nursing students receive inconsistent exposure to end of life care issues [ 22 ] and little or no training related to MAiD [ 23 ]. Without such education and reflection time in pre-entry nursing preparation, nurses are at significant risk for moral harm. An important first step in providing this preparation is to be able to assess the knowledge, values, and beliefs of nursing students regarding MAID and end of life care. As demand for MAiD increases along with the complexities of MAiD, it is critical to understand the knowledge, attitudes, and likelihood of engagement with MAiD among nursing students as a baseline upon which to build curriculum and as a means to track these variables over time.
Aim, design, and setting
The aim of this study was to develop a survey to measure nursing students’ knowledge, attitudes and beliefs, influences, and willingness to be involved in MAiD in the Canadian context. We sought to explore both their willingness to be involved in the registered nursing role and in the nurse practitioner role should they chose to prepare themselves to that level of education. The design was a mixed-method, modified e-Delphi method that entailed item generation, item refinement through an expert faculty panel [ 24 , 25 , 26 ], and initial item validation through a cognitive focus group interview with nursing students [ 27 ]. The settings were a University located in an urban area and a College located in a rural area in Western Canada.
Participants
A panel of 10 faculty from the two nursing education programs were recruited for Phase 2 of the e-Delphi. To be included, faculty were required to have a minimum of three years of experience in nurse education, be employed as nursing faculty, and self-identify as having experience with MAiD. A convenience sample of 5 fourth-year nursing students were recruited to participate in Phase 3. Students had to be in good standing in the nursing program and be willing to share their experiences of the survey in an online group interview format.
The modified e-Delphi was conducted in 3 phases: Phase 1 entailed item generation through literature and existing survey review. Phase 2 entailed item refinement through a faculty expert panel review with focus on content validity, prioritization, and revision of item wording [ 25 ]. Phase 3 entailed an assessment of face validity through focus group-based cognitive interview with nursing students.
Phase I. Item generation through literature review
The goal of phase 1 was to develop a bank of survey items that would represent the variables of interest and which could be provided to expert faculty in Phase 2. Initial survey items were generated through a literature review of similar surveys designed to assess knowledge and attitudes toward MAiD/euthanasia in healthcare providers; Canadian empirical studies on nurses’ roles and/or experiences with MAiD; and legislative and expert panel documents that outlined proposed changes to the legislative eligibility criteria and safeguards. The literature review was conducted in three online databases: CINAHL, PsycINFO, and Medline. Key words for the search included nurses , nursing students , medical students , NPs, MAiD , euthanasia , assisted death , and end-of-life care . Only articles written in English were reviewed. The legalization and legislation of MAiD is new in many countries; therefore, studies that were greater than twenty years old were excluded, no further exclusion criteria set for country.
Items from surveys designed to measure similar variables in other health care providers and geographic contexts were placed in a table and similar items were collated and revised into a single item. Then key variables were identified from the empirical literature on nurses and MAiD in Canada and checked against the items derived from the surveys to ensure that each of the key variables were represented. For example, conscientious objection has figured prominently in the Canadian literature, but there were few items that assessed knowledge of conscientious objection in other surveys and so items were added [ 15 , 21 , 28 , 29 ]. Finally, four case studies were added to the survey to address the anticipated changes to the Canadian legislation. The case studies were based upon the inclusion of mature minors, advanced consent, and mental disorder as the sole underlying medical condition. The intention was to assess nurses’ beliefs and comfort with these potential legislative changes.
Phase 2. Item refinement through expert panel review
The goal of phase 2 was to refine and prioritize the proposed survey items identified in phase 1 using a modified e-Delphi approach to achieve consensus among an expert panel [ 26 ]. Items from phase 1 were presented to an expert faculty panel using a Qualtrics (Provo, UT) online survey. Panel members were asked to review each item to determine if it should be: included, excluded or adapted for the survey. When adapted was selected faculty experts were asked to provide rationale and suggestions for adaptation through the use of an open text box. Items that reached a level of 75% consensus for either inclusion or adaptation were retained [ 25 , 26 ]. New items were categorized and added, and a revised survey was presented to the panel of experts in round 2. Panel members were again asked to review items, including new items, to determine if it should be: included, excluded, or adapted for the survey. Round 2 of the modified e-Delphi approach also included an item prioritization activity, where participants were then asked to rate the importance of each item, based on a 5-point Likert scale (low to high importance), which De Vaus [ 30 ] states is helpful for increasing the reliability of responses. Items that reached a 75% consensus on inclusion were then considered in relation to the importance it was given by the expert panel. Quantitative data were managed using SPSS (IBM Corp).
Phase 3. Face validity through cognitive interviews with nursing students
The goal of phase 3 was to obtain initial face validity of the proposed survey using a sample of nursing student informants. More specifically, student participants were asked to discuss how items were interpreted, to identify confusing wording or other problematic construction of items, and to provide feedback about the survey as a whole including readability and organization [ 31 , 32 , 33 ]. The focus group was held online and audio recorded. A semi-structured interview guide was developed for this study that focused on clarity, meaning, order and wording of questions; emotions evoked by the questions; and overall survey cohesion and length was used to obtain data (see Supplementary Material 2 for the interview guide). A prompt to “think aloud” was used to limit interviewer-imposed bias and encourage participants to describe their thoughts and response to a given item as they reviewed survey items [ 27 ]. Where needed, verbal probes such as “could you expand on that” were used to encourage participants to expand on their responses [ 27 ]. Student participants’ feedback was collated verbatim and presented to the research team where potential survey modifications were negotiated and finalized among team members. Conventional content analysis [ 34 ] of focus group data was conducted to identify key themes that emerged through discussion with students. Themes were derived from the data by grouping common responses and then using those common responses to modify survey items.
Ten nursing faculty participated in the expert panel. Eight of the 10 faculty self-identified as female. No faculty panel members reported conscientious objector status and ninety percent reported general agreement with MAiD with one respondent who indicated their view as “unsure.” Six of the 10 faculty experts had 16 years of experience or more working as a nurse educator.
Five nursing students participated in the cognitive interview focus group. The duration of the focus group was 2.5 h. All participants identified that they were born in Canada, self-identified as female (one preferred not to say) and reported having received some instruction about MAiD as part of their nursing curriculum. See Tables 1 and 2 for the demographic descriptors of the study sample. Study results will be reported in accordance with the study phases. See Fig. 1 for an overview of the results from each phase.
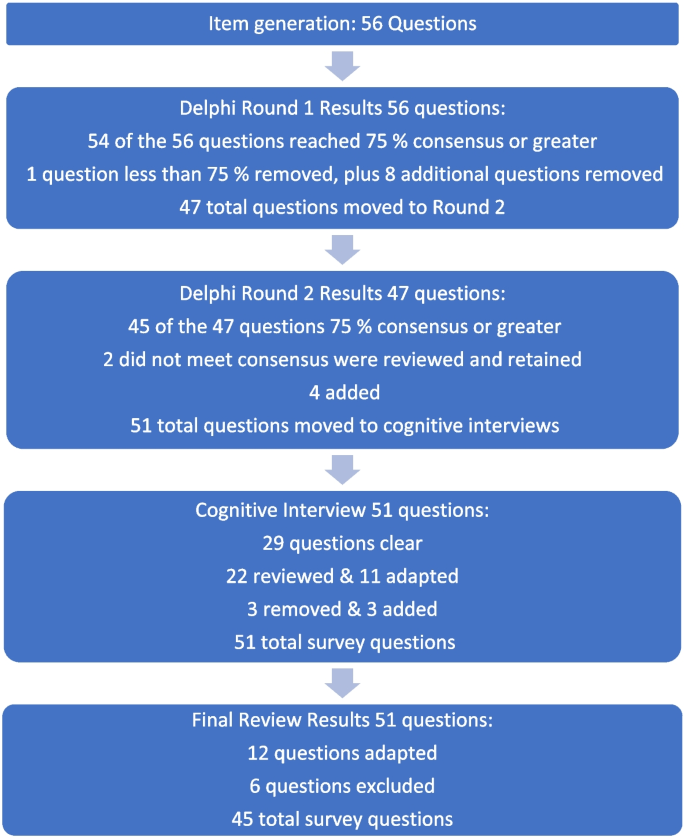
Fig. 1 Overview of survey development findings
Phase 1: survey item generation
Review of the literature identified that no existing survey was available for use with nursing students in the Canadian context. However, an analysis of themes across qualitative and quantitative studies of physicians, medical students, nurses, and nursing students provided sufficient data to develop a preliminary set of items suitable for adaptation to a population of nursing students.
Four major themes and factors that influence knowledge, attitudes, and beliefs about MAiD were evident from the literature: (i) endogenous or individual factors such as age, gender, personally held values, religion, religiosity, and/or spirituality [ 35 , 36 , 37 , 38 , 39 , 40 , 41 , 42 ], (ii) experience with death and dying in personal and/or professional life [ 35 , 40 , 41 , 43 , 44 , 45 ], (iii) training including curricular instruction about clinical role, scope of practice, or the law [ 23 , 36 , 39 ], and (iv) exogenous or social factors such as the influence of key leaders, colleagues, friends and/or family, professional and licensure organizations, support within professional settings, and/or engagement in MAiD in an interdisciplinary team context [ 9 , 35 , 46 ].
Studies of nursing students also suggest overlap across these categories. For example, value for patient autonomy [ 23 ] and the moral complexity of decision-making [ 37 ] are important factors that contribute to attitudes about MAiD and may stem from a blend of personally held values coupled with curricular content, professional training and norms, and clinical exposure. For example, students report that participation in end of life care allows for personal growth, shifts in perception, and opportunities to build therapeutic relationships with their clients [ 44 , 47 , 48 ].
Preliminary items generated from the literature resulted in 56 questions from 11 published sources (See Table 3 ). These items were constructed across four main categories: (i) socio-demographic questions; (ii) end of life care questions; (iii) knowledge about MAiD; or (iv) comfort and willingness to participate in MAiD. Knowledge questions were refined to reflect current MAiD legislation, policies, and regulatory frameworks. Falconer [ 39 ] and Freeman [ 45 ] studies were foundational sources for item selection. Additionally, four case studies were written to reflect the most recent anticipated changes to MAiD legislation and all used the same open-ended core questions to address respondents’ perspectives about the patient’s right to make the decision, comfort in assisting a physician or NP to administer MAiD in that scenario, and hypothesized comfort about serving as a primary provider if qualified as an NP in future. Response options for the survey were also constructed during this stage and included: open text, categorical, yes/no , and Likert scales.
Phase 2: faculty expert panel review
Of the 56 items presented to the faculty panel, 54 questions reached 75% consensus. However, based upon the qualitative responses 9 items were removed largely because they were felt to be repetitive. Items that generated the most controversy were related to measuring religion and spirituality in the Canadian context, defining end of life care when there is no agreed upon time frames (e.g., last days, months, or years), and predicting willingness to be involved in a future events – thus predicting their future selves. Phase 2, round 1 resulted in an initial set of 47 items which were then presented back to the faculty panel in round 2.
Of the 47 initial questions presented to the panel in round 2, 45 reached a level of consensus of 75% or greater, and 34 of these questions reached a level of 100% consensus [ 27 ] of which all participants chose to include without any adaptations) For each question, level of importance was determined based on a 5-point Likert scale (1 = very unimportant, 2 = somewhat unimportant, 3 = neutral, 4 = somewhat important, and 5 = very important). Figure 2 provides an overview of the level of importance assigned to each item.
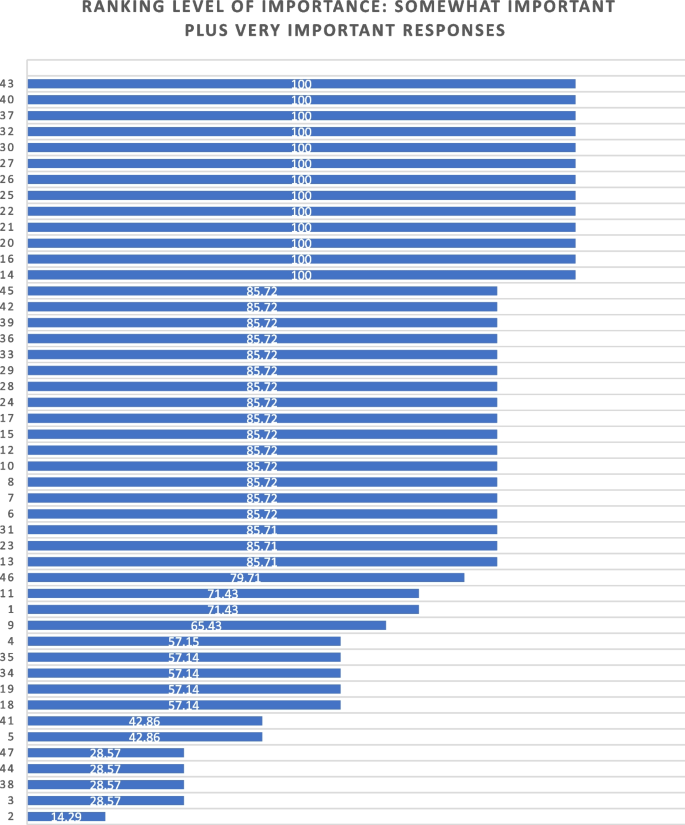
Ranking level of importance for survey items
After round 2, a careful analysis of participant comments and level of importance was completed by the research team. While the main method of survey item development came from participants’ response to the first round of Delphi consensus ratings, level of importance was used to assist in the decision of whether to keep or modify questions that created controversy, or that rated lower in the include/exclude/adapt portion of the Delphi. Survey items that rated low in level of importance included questions about future roles, sex and gender, and religion/spirituality. After deliberation by the research committee, these questions were retained in the survey based upon the importance of these variables in the scientific literature.
Of the 47 questions remaining from Phase 2, round 2, four were revised. In addition, the two questions that did not meet the 75% cut off level for consensus were reviewed by the research team. The first question reviewed was What is your comfort level with providing a MAiD death in the future if you were a qualified NP ? Based on a review of participant comments, it was decided to retain this question for the cognitive interviews with students in the final phase of testing. The second question asked about impacts on respondents’ views of MAiD and was changed from one item with 4 subcategories into 4 separate items, resulting in a final total of 51 items for phase 3. The revised survey was then brought forward to the cognitive interviews with student participants in Phase 3. (see Supplementary Material 1 for a complete description of item modification during round 2).
Phase 3. Outcomes of cognitive interview focus group
Of the 51 items reviewed by student participants, 29 were identified as clear with little or no discussion. Participant comments for the remaining 22 questions were noted and verified against the audio recording. Following content analysis of the comments, four key themes emerged through the student discussion: unclear or ambiguous wording; difficult to answer questions; need for additional response options; and emotional response evoked by questions. An example of unclear or ambiguous wording was a request for clarity in the use of the word “sufficient” in the context of assessing an item that read “My nursing education has provided sufficient content about the nursing role in MAiD.” “Sufficient” was viewed as subjective and “laden with…complexity that distracted me from the question.” The group recommended rewording the item to read “My nursing education has provided enough content for me to care for a patient considering or requesting MAiD.”
An example of having difficulty answering questions related to limited knowledge related to terms used in the legislation such as such as safeguards , mature minor , eligibility criteria , and conscientious objection. Students were unclear about what these words meant relative to the legislation and indicated that this lack of clarity would hamper appropriate responses to the survey. To ensure that respondents are able to answer relevant questions, student participants recommended that the final survey include explanation of key terms such as mature minor and conscientious objection and an overview of current legislation.
Response options were also a point of discussion. Participants noted a lack of distinction between response options of unsure and unable to say . Additionally, scaling of attitudes was noted as important since perspectives about MAiD are dynamic and not dichotomous “agree or disagree” responses. Although the faculty expert panel recommended the integration of the demographic variables of religious and/or spiritual remain as a single item, the student group stated a preference to have religion and spirituality appear as separate items. The student focus group also took issue with separate items for the variables of sex and gender, specifically that non-binary respondents might feel othered or “outed” particularly when asked to identify their sex. These variables had been created based upon best practices in health research but students did not feel they were appropriate in this context [ 49 ]. Finally, students agreed with the faculty expert panel in terms of the complexity of projecting their future involvement as a Nurse Practitioner. One participant stated: “I certainly had to like, whoa, whoa, whoa. Now let me finish this degree first, please.” Another stated, “I'm still imagining myself, my future career as an RN.”
Finally, student participants acknowledged the array of emotions that some of the items produced for them. For example, one student described positive feelings when interacting with the survey. “Brought me a little bit of feeling of joy. Like it reminded me that this is the last piece of independence that people grab on to.” Another participant, described the freedom that the idea of an advance request gave her. “The advance request gives the most comfort for me, just with early onset Alzheimer’s and knowing what it can do.” But other participants described less positive feelings. For example, the mature minor case study yielded a comment: “This whole scenario just made my heart hurt with the idea of a child requesting that.”
Based on the data gathered from the cognitive interview focus group of nursing students, revisions were made to 11 closed-ended questions (see Table 4 ) and 3 items were excluded. In the four case studies, the open-ended question related to a respondents’ hypothesized actions in a future role as NP were removed. The final survey consists of 45 items including 4 case studies (see Supplementary Material 3 ).
The aim of this study was to develop and validate a survey that can be used to track the growth of knowledge about MAiD among nursing students over time, inform training programs about curricular needs, and evaluate attitudes and willingness to participate in MAiD at time-points during training or across nursing programs over time.
The faculty expert panel and student participants in the cognitive interview focus group identified a need to establish core knowledge of the terminology and legislative rules related to MAiD. For example, within the cognitive interview group of student participants, several acknowledged lack of clear understanding of specific terms such as “conscientious objector” and “safeguards.” Participants acknowledged discomfort with the uncertainty of not knowing and their inclination to look up these terms to assist with answering the questions. This survey can be administered to nursing or pre-nursing students at any phase of their training within a program or across training programs. However, in doing so it is important to acknowledge that their baseline knowledge of MAiD will vary. A response option of “not sure” is important and provides a means for respondents to convey uncertainty. If this survey is used to inform curricular needs, respondents should be given explicit instructions not to conduct online searches to inform their responses, but rather to provide an honest appraisal of their current knowledge and these instructions are included in the survey (see Supplementary Material 3 ).
Some provincial regulatory bodies have established core competencies for entry-level nurses that include MAiD. For example, the BC College of Nurses and Midwives (BCCNM) requires “knowledge about ethical, legal, and regulatory implications of medical assistance in dying (MAiD) when providing nursing care.” (10 p. 6) However, across Canada curricular content and coverage related to end of life care and MAiD is variable [ 23 ]. Given the dynamic nature of the legislation that includes portions of the law that are embargoed until 2024, it is important to ensure that respondents are guided by current and accurate information. As the law changes, nursing curricula, and public attitudes continue to evolve, inclusion of core knowledge and content is essential and relevant for investigators to be able to interpret the portions of the survey focused on attitudes and beliefs about MAiD. Content knowledge portions of the survey may need to be modified over time as legislation and training change and to meet the specific purposes of the investigator.
Given the sensitive nature of the topic, it is strongly recommended that surveys be conducted anonymously and that students be provided with an opportunity to discuss their responses to the survey. A majority of feedback from both the expert panel of faculty and from student participants related to the wording and inclusion of demographic variables, in particular religion, religiosity, gender identity, and sex assigned at birth. These and other demographic variables have the potential to be highly identifying in small samples. In any instance in which the survey could be expected to yield demographic group sizes less than 5, users should eliminate the demographic variables from the survey. For example, the profession of nursing is highly dominated by females with over 90% of nurses who identify as female [ 50 ]. Thus, a survey within a single class of students or even across classes in a single institution is likely to yield a small number of male respondents and/or respondents who report a difference between sex assigned at birth and gender identity. When variables that serve to identify respondents are included, respondents are less likely to complete or submit the survey, to obscure their responses so as not to be identifiable, or to be influenced by social desirability bias in their responses rather than to convey their attitudes accurately [ 51 ]. Further, small samples do not allow for conclusive analyses or interpretation of apparent group differences. Although these variables are often included in surveys, such demographics should be included only when anonymity can be sustained. In small and/or known samples, highly identifying variables should be omitted.
There are several limitations associated with the development of this survey. The expert panel was comprised of faculty who teach nursing students and are knowledgeable about MAiD and curricular content, however none identified as a conscientious objector to MAiD. Ideally, our expert panel would have included one or more conscientious objectors to MAiD to provide a broader perspective. Review by practitioners who participate in MAiD, those who are neutral or undecided, and practitioners who are conscientious objectors would ensure broad applicability of the survey. This study included one student cognitive interview focus group with 5 self-selected participants. All student participants had held discussions about end of life care with at least one patient, 4 of 5 participants had worked with a patient who requested MAiD, and one had been present for a MAiD death. It is not clear that these participants are representative of nursing students demographically or by experience with end of life care. It is possible that the students who elected to participate hold perspectives and reflections on patient care and MAiD that differ from students with little or no exposure to end of life care and/or MAiD. However, previous studies find that most nursing students have been involved with end of life care including meaningful discussions about patients’ preferences and care needs during their education [ 40 , 44 , 47 , 48 , 52 ]. Data collection with additional student focus groups with students early in their training and drawn from other training contexts would contribute to further validation of survey items.
Future studies should incorporate pilot testing with small sample of nursing students followed by a larger cross-program sample to allow evaluation of the psychometric properties of specific items and further refinement of the survey tool. Consistent with literature about the importance of leadership in the context of MAiD [ 12 , 53 , 54 ], a study of faculty knowledge, beliefs, and attitudes toward MAiD would provide context for understanding student perspectives within and across programs. Additional research is also needed to understand the timing and content coverage of MAiD across Canadian nurse training programs’ curricula.
The implementation of MAiD is complex and requires understanding of the perspectives of multiple stakeholders. Within the field of nursing this includes clinical providers, educators, and students who will deliver clinical care. A survey to assess nursing students’ attitudes toward and willingness to participate in MAiD in the Canadian context is timely, due to the legislation enacted in 2016 and subsequent modifications to the law in 2021 with portions of the law to be enacted in 2027. Further development of this survey could be undertaken to allow for use in settings with practicing nurses or to allow longitudinal follow up with students as they enter practice. As the Canadian landscape changes, ongoing assessment of the perspectives and needs of health professionals and students in the health professions is needed to inform policy makers, leaders in practice, curricular needs, and to monitor changes in attitudes and practice patterns over time.
Availability of data and materials
The datasets used and/or analysed during the current study are not publicly available due to small sample sizes, but are available from the corresponding author on reasonable request.
Abbreviations
British Columbia College of Nurses and Midwives
Medical assistance in dying
Nurse practitioner
Registered nurse
University of British Columbia Okanagan
Nicol J, Tiedemann M. Legislative Summary: Bill C-14: An Act to amend the Criminal Code and to make related amendments to other Acts (medical assistance in dying). Available from: https://lop.parl.ca/staticfiles/PublicWebsite/Home/ResearchPublications/LegislativeSummaries/PDF/42-1/c14-e.pdf .
Downie J, Scallion K. Foreseeably unclear. The meaning of the “reasonably foreseeable” criterion for access to medical assistance in dying in Canada. Dalhousie Law J. 2018;41(1):23–57.
Nicol J, Tiedeman M. Legislative summary of Bill C-7: an act to amend the criminal code (medical assistance in dying). Ottawa: Government of Canada; 2021.
Google Scholar
Council of Canadian Academies. The state of knowledge on medical assistance in dying where a mental disorder is the sole underlying medical condition. Ottawa; 2018. Available from: https://cca-reports.ca/wp-content/uploads/2018/12/The-State-of-Knowledge-on-Medical-Assistance-in-Dying-Where-a-Mental-Disorder-is-the-Sole-Underlying-Medical-Condition.pdf .
Council of Canadian Academies. The state of knowledge on advance requests for medical assistance in dying. Ottawa; 2018. Available from: https://cca-reports.ca/wp-content/uploads/2019/02/The-State-of-Knowledge-on-Advance-Requests-for-Medical-Assistance-in-Dying.pdf .
Council of Canadian Academies. The state of knowledge on medical assistance in dying for mature minors. Ottawa; 2018. Available from: https://cca-reports.ca/wp-content/uploads/2018/12/The-State-of-Knowledge-on-Medical-Assistance-in-Dying-for-Mature-Minors.pdf .
Health Canada. Third annual report on medical assistance in dying in Canada 2021. Ottawa; 2022. [cited 2023 Oct 23]. Available from: https://www.canada.ca/en/health-canada/services/medical-assistance-dying/annual-report-2021.html .
Banner D, Schiller CJ, Freeman S. Medical assistance in dying: a political issue for nurses and nursing in Canada. Nurs Philos. 2019;20(4): e12281.
Article PubMed Google Scholar
Pesut B, Thorne S, Stager ML, Schiller CJ, Penney C, Hoffman C, et al. Medical assistance in dying: a review of Canadian nursing regulatory documents. Policy Polit Nurs Pract. 2019;20(3):113–30.
Article PubMed PubMed Central Google Scholar
College of Registered Nurses of British Columbia. Scope of practice for registered nurses [Internet]. Vancouver; 2018. Available from: https://www.bccnm.ca/Documents/standards_practice/rn/RN_ScopeofPractice.pdf .
Pesut B, Thorne S, Schiller C, Greig M, Roussel J, Tishelman C. Constructing good nursing practice for medical assistance in dying in Canada: an interpretive descriptive study. Global Qual Nurs Res. 2020;7:2333393620938686. https://doi.org/10.1177/2333393620938686 .
Article Google Scholar
Pesut B, Thorne S, Schiller CJ, Greig M, Roussel J. The rocks and hard places of MAiD: a qualitative study of nursing practice in the context of legislated assisted death. BMC Nurs. 2020;19:12. https://doi.org/10.1186/s12912-020-0404-5 .
Pesut B, Greig M, Thorne S, Burgess M, Storch JL, Tishelman C, et al. Nursing and euthanasia: a narrative review of the nursing ethics literature. Nurs Ethics. 2020;27(1):152–67.
Pesut B, Thorne S, Storch J, Chambaere K, Greig M, Burgess M. Riding an elephant: a qualitative study of nurses’ moral journeys in the context of Medical Assistance in Dying (MAiD). Journal Clin Nurs. 2020;29(19–20):3870–81.
Lamb C, Babenko-Mould Y, Evans M, Wong CA, Kirkwood KW. Conscientious objection and nurses: results of an interpretive phenomenological study. Nurs Ethics. 2018;26(5):1337–49.
Wright DK, Chan LS, Fishman JR, Macdonald ME. “Reflection and soul searching:” Negotiating nursing identity at the fault lines of palliative care and medical assistance in dying. Social Sci & Med. 2021;289: 114366.
Beuthin R, Bruce A, Scaia M. Medical assistance in dying (MAiD): Canadian nurses’ experiences. Nurs Forum. 2018;54(4):511–20.
Bruce A, Beuthin R. Medically assisted dying in Canada: "Beautiful Death" is transforming nurses' experiences of suffering. The Canadian J Nurs Res | Revue Canadienne de Recherche en Sci Infirmieres. 2020;52(4):268–77. https://doi.org/10.1177/0844562119856234 .
Canadian Nurses Association. Code of ethics for registered nurses. Ottawa; 2017. Available from: https://www.cna-aiic.ca/en/nursing/regulated-nursing-in-canada/nursing-ethics .
Canadian Nurses Association. National nursing framework on Medical Assistance in Dying in Canada. Ottawa: 2017. Available from: https://www.virtualhospice.ca/Assets/cna-national-nursing-framework-on-maidEng_20170216155827.pdf .
Pesut B, Thorne S, Greig M. Shades of gray: conscientious objection in medical assistance in dying. Nursing Inq. 2020;27(1): e12308.
Durojaiye A, Ryan R, Doody O. Student nurse education and preparation for palliative care: a scoping review. PLoS ONE. 2023. https://doi.org/10.1371/journal.pone.0286678 .
McMechan C, Bruce A, Beuthin R. Canadian nursing students’ experiences with medical assistance in dying | Les expériences d’étudiantes en sciences infirmières au regard de l’aide médicale à mourir. Qual Adv Nurs Educ - Avancées en Formation Infirmière. 2019;5(1). https://doi.org/10.17483/2368-6669.1179 .
Adler M, Ziglio E. Gazing into the oracle. The Delphi method and its application to social policy and public health. London: Jessica Kingsley Publishers; 1996
Keeney S, Hasson F, McKenna H. Consulting the oracle: ten lessons from using the Delphi technique in nursing research. J Adv Nurs. 2006;53(2):205–12.
Keeney S, Hasson F, McKenna H. The Delphi technique in nursing and health research. 1st ed. City: Wiley; 2011.
Willis GB. Cognitive interviewing: a tool for improving questionnaire design. 1st ed. Thousand Oaks, Calif: Sage; 2005. ISBN: 9780761928041
Lamb C, Evans M, Babenko-Mould Y, Wong CA, Kirkwood EW. Conscience, conscientious objection, and nursing: a concept analysis. Nurs Ethics. 2017;26(1):37–49.
Lamb C, Evans M, Babenko-Mould Y, Wong CA, Kirkwood K. Nurses’ use of conscientious objection and the implications of conscience. J Adv Nurs. 2018;75(3):594–602.
de Vaus D. Surveys in social research. 6th ed. Abingdon, Oxon: Routledge; 2014.
Boateng GO, Neilands TB, Frongillo EA, Melgar-Quiñonez HR, Young SL. Best practices for developing and validating scales for health, social, and behavioral research: A primer. Front Public Health. 2018;6:149. https://doi.org/10.3389/fpubh.2018.00149 .
Puchta C, Potter J. Focus group practice. 1st ed. London: Sage; 2004.
Book Google Scholar
Streiner DL, Norman GR, Cairney J. Health measurement scales: a practical guide to their development and use. 5th ed. Oxford: Oxford University Press; 2015.
Hsieh H-F, Shannon SE. Three approaches to qualitative content analysis. Qual Health Res. 2005;15(9):1277–88.
Adesina O, DeBellis A, Zannettino L. Third-year Australian nursing students’ attitudes, experiences, knowledge, and education concerning end-of-life care. Int J of Palliative Nurs. 2014;20(8):395–401.
Bator EX, Philpott B, Costa AP. This moral coil: a cross-sectional survey of Canadian medical student attitudes toward medical assistance in dying. BMC Med Ethics. 2017;18(1):58.
Beuthin R, Bruce A, Scaia M. Medical assistance in dying (MAiD): Canadian nurses’ experiences. Nurs Forum. 2018;53(4):511–20.
Brown J, Goodridge D, Thorpe L, Crizzle A. What is right for me, is not necessarily right for you: the endogenous factors influencing nonparticipation in medical assistance in dying. Qual Health Res. 2021;31(10):1786–1800.
Falconer J, Couture F, Demir KK, Lang M, Shefman Z, Woo M. Perceptions and intentions toward medical assistance in dying among Canadian medical students. BMC Med Ethics. 2019;20(1):22.
Green G, Reicher S, Herman M, Raspaolo A, Spero T, Blau A. Attitudes toward euthanasia—dual view: Nursing students and nurses. Death Stud. 2022;46(1):124–31.
Hosseinzadeh K, Rafiei H. Nursing student attitudes toward euthanasia: a cross-sectional study. Nurs Ethics. 2019;26(2):496–503.
Ozcelik H, Tekir O, Samancioglu S, Fadiloglu C, Ozkara E. Nursing students’ approaches toward euthanasia. Omega (Westport). 2014;69(1):93–103.
Canning SE, Drew C. Canadian nursing students’ understanding, and comfort levels related to medical assistance in dying. Qual Adv Nurs Educ - Avancées en Formation Infirmière. 2022;8(2). https://doi.org/10.17483/2368-6669.1326 .
Edo-Gual M, Tomás-Sábado J, Bardallo-Porras D, Monforte-Royo C. The impact of death and dying on nursing students: an explanatory model. J Clin Nurs. 2014;23(23–24):3501–12.
Freeman LA, Pfaff KA, Kopchek L, Liebman J. Investigating palliative care nurse attitudes towards medical assistance in dying: an exploratory cross-sectional study. J Adv Nurs. 2020;76(2):535–45.
Brown J, Goodridge D, Thorpe L, Crizzle A. “I am okay with it, but I am not going to do it:” the exogenous factors influencing non-participation in medical assistance in dying. Qual Health Res. 2021;31(12):2274–89.
Dimoula M, Kotronoulas G, Katsaragakis S, Christou M, Sgourou S, Patiraki E. Undergraduate nursing students’ knowledge about palliative care and attitudes towards end-of-life care: A three-cohort, cross-sectional survey. Nurs Educ Today. 2019;74:7–14.
Matchim Y, Raetong P. Thai nursing students’ experiences of caring for patients at the end of life: a phenomenological study. Int J Palliative Nurs. 2018;24(5):220–9.
Canadian Institute for Health Research. Sex and gender in health research [Internet]. Ottawa: CIHR; 2021 [cited 2023 Oct 23]. Available from: https://cihr-irsc.gc.ca/e/50833.html .
Canadian Nurses’ Association. Nursing statistics. Ottawa: CNA; 2023 [cited 2023 Oct 23]. Available from: https://www.cna-aiic.ca/en/nursing/regulated-nursing-in-canada/nursing-statistics .
Krumpal I. Determinants of social desirability bias in sensitive surveys: a literature review. Qual Quant. 2013;47(4):2025–47. https://doi.org/10.1007/s11135-011-9640-9 .
Ferri P, Di Lorenzo R, Stifani S, Morotti E, Vagnini M, Jiménez Herrera MF, et al. Nursing student attitudes toward dying patient care: a European multicenter cross-sectional study. Acta Bio Medica Atenei Parmensis. 2021;92(S2): e2021018.
PubMed PubMed Central Google Scholar
Beuthin R, Bruce A. Medical assistance in dying (MAiD): Ten things leaders need to know. Nurs Leadership. 2018;31(4):74–81.
Thiele T, Dunsford J. Nurse leaders’ role in medical assistance in dying: a relational ethics approach. Nurs Ethics. 2019;26(4):993–9.
Download references
Acknowledgements
We would like to acknowledge the faculty and students who generously contributed their time to this work.
JS received a student traineeship through the Principal Research Chairs program at the University of British Columbia Okanagan.
Author information
Authors and affiliations.
School of Health and Human Services, Selkirk College, Castlegar, BC, Canada
Jocelyn Schroeder & Barbara Pesut
School of Nursing, University of British Columbia Okanagan, Kelowna, BC, Canada
Barbara Pesut, Lise Olsen, Nelly D. Oelke & Helen Sharp
You can also search for this author in PubMed Google Scholar
Contributions
JS made substantial contributions to the conception of the work; data acquisition, analysis, and interpretation; and drafting and substantively revising the work. JS has approved the submitted version and agreed to be personally accountable for the author's own contributions and to ensure that questions related to the accuracy or integrity of any part of the work, even ones in which the author was not personally involved, are appropriately investigated, resolved, and the resolution documented in the literature. BP made substantial contributions to the conception of the work; data acquisition, analysis, and interpretation; and drafting and substantively revising the work. BP has approved the submitted version and agreed to be personally accountable for the author's own contributions and to ensure that questions related to the accuracy or integrity of any part of the work, even ones in which the author was not personally involved, are appropriately investigated, resolved, and the resolution documented in the literature. LO made substantial contributions to the conception of the work; data acquisition, analysis, and interpretation; and substantively revising the work. LO has approved the submitted version and agreed to be personally accountable for the author's own contributions and to ensure that questions related to the accuracy or integrity of any part of the work, even ones in which the author was not personally involved, are appropriately investigated, resolved, and the resolution documented in the literature. NDO made substantial contributions to the conception of the work; data acquisition, analysis, and interpretation; and substantively revising the work. NDO has approved the submitted version and agreed to be personally accountable for the author's own contributions and to ensure that questions related to the accuracy or integrity of any part of the work, even ones in which the author was not personally involved, are appropriately investigated, resolved, and the resolution documented in the literature. HS made substantial contributions to drafting and substantively revising the work. HS has approved the submitted version and agreed to be personally accountable for the author's own contributions and to ensure that questions related to the accuracy or integrity of any part of the work, even ones in which the author was not personally involved, are appropriately investigated, resolved, and the resolution documented in the literature.
Authors’ information
JS conducted this study as part of their graduate requirements in the School of Nursing, University of British Columbia Okanagan.
Corresponding author
Correspondence to Barbara Pesut .
Ethics declarations
Ethics approval and consent to participate.
The research was approved by the Selkirk College Research Ethics Board (REB) ID # 2021–011 and the University of British Columbia Behavioral Research Ethics Board ID # H21-01181.
All participants provided written and informed consent through approved consent processes. Research was conducted in accordance with the Declaration of Helsinki.
Consent for publication
Not applicable.
Competing interests
The authors declare they have no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Supplementary material 1., supplementary material 2., supplementary material 3., rights and permissions.
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Schroeder, J., Pesut, B., Olsen, L. et al. Developing a survey to measure nursing students’ knowledge, attitudes and beliefs, influences, and willingness to be involved in Medical Assistance in Dying (MAiD): a mixed method modified e-Delphi study. BMC Nurs 23 , 326 (2024). https://doi.org/10.1186/s12912-024-01984-z
Download citation
Received : 24 October 2023
Accepted : 28 April 2024
Published : 14 May 2024
DOI : https://doi.org/10.1186/s12912-024-01984-z
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Medical assistance in dying (MAiD)
- End of life care
- Student nurses
- Nursing education
BMC Nursing
ISSN: 1472-6955
- General enquiries: [email protected]

COMMENTS
1.1. Evaluation of ADHD. The current diagnostic criteria for ADHD can be found in the DSM-5 [] and in the International Statistical Classification of Diseases and Related Health Problems, eleventh revision, from the World Health Organization [].Various evaluation instruments are used to identify ADHD, from general assessments via broad scales such as the Wechsler scale, to more specific tests ...
Nurse Sienna knows that ADHD is likely a group of disorders thought to be caused by abnormalities in the function of the central nervous system, which regulates concentration, attention, focus, and impulse control. As a result, patients can experience inattention, hyperactivity, and impulsivity, which may lead to disrupted learning, school ...
undergraduate students with ADHD, and we adapted this approach to our setting. The following section presents a case study of a coaching intervention and its impact on a for-mer nursing student with ADHD, the fourth author (WYM) of this paper. Information about the impact of the coach-ing intervention originates in a structured conversation that
In adult ADHD, the symptoms may be comorbid or mimic other conditions making diagnosis and treatment difficult. Adults with ADHD require an in-depth assessment for proper diagnosis and treatment. The presentation and treatment of adults with ADHD can be complex and often requires interdisciplinary care.
5. Try the Pomodoro Technique. This strategy works with the short attention span that many people with ADHD experience. The Pomodoro Technique is a time management tool that sets a 25-minute limit on the amount of time you work on any assignment before taking a scheduled five-minute break.
Stimulant medications have been shown to be effective in the treatment of ADHD in both children and adults. The mechanism of action for drug therapy is believed to be linked to an increase in extracellular dopamine and norepinephrine levels in the frontal cortex by inhibiting the reuptake of these neurotransmitters (Contini et al., 2013).The overall outcome is improvement in impulsive behavior ...
Fig. 1 summarizes suggested steps in caring for adults with ADHD and can guide providers with limited experience in treating the disorder. With improved science and longer life spans, many disorders once seen only during childhood are now continuing into adulthood. ADHD is one of many disorders once thought to only occur in children and resolve as
A fantastic method that many students with ADHD utilize is the Pomodoro technique. This technique involves identifying a specific task, working on it for 25 minutes followed by a 5-minute break. This cycle repeats four times and then you take a longer break of about 15 to 30 minutes.
Case Study 1 - Jack Jack is a 7 year old male Grade 1 student who lives in Toronto with his parents. He is the only child to two parents, both of whom have completed post-graduate education. There is an extended family history of Attention Deficit/Hyperactivity Disorder (ADHD), mental health concerns as well as academic excellence.
ADHD increases the risk of substance misuse disorders 1.5-fold (2.4-fold for smoking) and problematic media use 9.3-fold in adolescence 55 56 and increases the risk of becoming obese 1.23-fold for adolescent girls. 57 58 59 It is also associated with different forms of dysregulated eating in children and adolescents.
ADHD case study for mental health module 13 case study adhd case study amy lin arizona college of nursing nur 356 professor ignacio nunez july 31, 2022 module. Skip to document. University; High School. Books; ... Students also viewed. POST EXAM 1-1 - post exam worksheet on rhythms;
We present a case study to illustrate the coaching intervention we adapted from the education literature for a nursing student with ADHD who was struggling in clinical practice courses.
ADHD Nursing Care Plan 1. Nursing Diagnosis: Disturbed Thought Process related to dopamine imbalance secondary to ADHD as evidenced by forgetfulness, inability to concentrate and pay attention, inability to do tasks as instructed, blurting of words, poor decision-making skills, and difficulty handling complex tasks.
ADHD case study nursing plan of care assessment: frankie is year old boy who keeps the class in an uproar and has been suspended from school three times within ... and is reported to distract other students. Frankie's mother reports that his behavior has been difficult from a toddler and he has become unbearably restless and demanding ...
The use of neurofeedback in interventions for ADHD began in 1973, although the first study with positive results was published in 1976 [17]. Since then, various studies have reported benefits from using neurofeedback in infants, with improvements in behavior, attention, and impulsivity control (e.g., [18-22]).
up the case study, names those activities in brief without the full details and explicit information each client-family receives in why and how to implement the program. Go to www.handle.org for more information. The HANDLE® Institute 7 Mt. Lassen Drive, Suite B110 San Rafael, CA 94903 415-479-1800
Case Study: Interventions 3 Case Study: Interventions for an ADHD Student This case-study is based on one of my 2nd-grade students. Pseudonyms have been used to maintain anonymity. On Saturday, January 26, 2008 I called Mr. and Mrs. Petrenko's residence via telephone. I spoke to Mrs. Petrenko and outlined the study by reading to her
ADHA Case Study Emily Enriquez Arizona College of Nursing NUR356: Mental Health Theory & Application Professor Stacey Fife August 5th, 2023. ADHA Case Study. Assessment: Frankie is a 9-year-old kid who constantly disrupts the lessons and has been expelled from school on three occasions.
The prevalence of ADHD in UK adults is estimated at 3-4% [ 3 ], with a male-to-female ratio of 3:2 [ 4 ]. Prevalence in UK medical students has been found to be at least 5.5% [ 5 ]. ADHD diagnostic rates vary, influenced by factors such as gender, race, socioeconomic status, and ethnicity [ 6 ]. Students who achieve high grades in academia ...
Click on a case study below to view in our Nursing Case Study Examples course which holds all of our 40+ nursing case studies with answers. Acute Kidney Injury Nursing Case Study. Continue Case Study. Cardiogenic Shock Nursing Case Study. Continue Case Study. Breast Cancer Nursing Case Study. Continue Case Study. Respiratory Nursing Case Study.
ADHD symptoms can change over time and presents itself in three different ways. May 15, 2024. Treatment of ADHD. ADHD treatment recommendations vary by age group. May 15, 2024. ADHD Information and Resources for States. Read this page for more information and resources on ADHD.
Attention deficit hyperactivity disorder (ADHD) is the most prevalent neurodevelopmental disorder among children, with an estimated prevalence increasing from 6.1% in 1997-1998 to 10.8% in 2022 ...
And during the pandemic, stimulant prescriptions, primarily used to treat A.D.H.D., "sharply increased," particularly among young adults and women, according to a study published in JAMA ...
The final survey consists of 45 items including 4 case studies. Systematic evaluation of knowledge-to-date coupled with stakeholder perspectives supports robust survey design. This study yielded a survey to assess nursing students' attitudes toward MAiD in a Canadian context.