- - Google Chrome
Intended for healthcare professionals
- Access provided by Google Indexer
- My email alerts
- BMA member login
- Username * Password * Forgot your log in details? Need to activate BMA Member Log In Log in via OpenAthens Log in via your institution


Search form
- Advanced search
- Search responses
- Search blogs
- Performing a...
Performing a literature review
- Related content
- Peer review
- Gulraj S Matharu , academic foundation doctor ,
- Christopher D Buckley , Arthritis Research UK professor of rheumatology
- 1 Institute of Biomedical Research, College of Medical and Dental Sciences, School of Immunity and Infection, University of Birmingham, UK
A necessary skill for any doctor
What causes disease, which drug is best, does this patient need surgery, and what is the prognosis? Although experience helps in answering these questions, ultimately they are best answered by evidence based medicine. But how do you assess the evidence? As a medical student, and throughout your career as a doctor, critical appraisal of published literature is an important skill to develop and refine. At medical school you will repeatedly appraise published literature and write literature reviews. These activities are commonly part of a special study module, research project for an intercalated degree, or another type of essay based assignment.
Formulating a question
Literature reviews are most commonly performed to help answer a particular question. While you are at medical school, there will usually be some choice regarding the area you are going to review.
Once you have identified a subject area for review, the next step is to formulate a specific research question. This is arguably the most important step because a clear question needs to be defined from the outset, which you aim to answer by doing the review. The clearer the question, the more likely it is that the answer will be clear too. It is important to have discussions with your supervisor when formulating a research question as his or her input will be invaluable. The research question must be objective and concise because it is easier to search through the evidence with a clear question. The question also needs to be feasible. What is the point in having a question for which no published evidence exists? Your supervisor’s input will ensure you are not trying to answer an unrealistic question. Finally, is the research question clinically important? There are many research questions that may be answered, but not all of them will be relevant to clinical practice. The research question we will use as an example to work through in this article is, “What is the evidence for using angiotensin converting enzyme (ACE) inhibitors in patients with hypertension?”
Collecting the evidence
After formulating a specific research question for your literature review, the next step is to collect the evidence. Your supervisor will initially point you in the right direction by highlighting some of the more relevant papers published. Before doing the literature search it is important to agree a list of keywords with your supervisor. A source of useful keywords can be obtained by reading Cochrane reviews or other systematic reviews, such as those published in the BMJ . 1 2 A relevant Cochrane review for our research question on ACE inhibitors in hypertension is that by Heran and colleagues. 3 Appropriate keywords to search for the evidence include the words used in your research question (“angiotensin converting enzyme inhibitor,” “hypertension,” “blood pressure”), details of the types of study you are looking for (“randomised controlled trial,” “case control,” “cohort”), and the specific drugs you are interested in (that is, the various ACE inhibitors such as “ramipril,” “perindopril,” and “lisinopril”).
Once keywords have been agreed it is time to search for the evidence using the various electronic medical databases (such as PubMed, Medline, and EMBASE). PubMed is the largest of these databases and contains online information and tutorials on how to do literature searches with worked examples. Searching the databases and obtaining the articles are usually free of charge through the subscription that your university pays. Early consultation with a medical librarian is important as it will help you perform your literature search in an impartial manner, and librarians can train you to do these searches for yourself.
Literature searches can be broad or tailored to be more specific. With our example, a broad search would entail searching all articles that contain the words “blood pressure” or “ACE inhibitor.” This provides a comprehensive list of all the literature, but there are likely to be thousands of articles to review subsequently (fig 1). ⇓ In contrast, various search restrictions can be applied on the electronic databases to filter out papers that may not be relevant to your review. Figure 2 gives an example of a specific search. ⇓ The search terms used in this case were “angiotensin converting enzyme inhibitor” and “hypertension.” The limits applied to this search were all randomised controlled trials carried out in humans, published in the English language over the last 10 years, with the search terms appearing in the title of the study only. Thus the more specific the search strategy, the more manageable the number of articles to review (fig 3), and this will save you time. ⇓ However, this method risks your not identifying all the evidence in the particular field. Striking a balance between a broad and a specific search strategy is therefore important. This will come with experience and consultation with your supervisor. It is important to note that evidence is continually becoming available on these electronic databases and therefore repeating the same search at a later date can provide new evidence relevant to your review.

Fig 1 Results from a broad literature search using the term “angiotensin converting enzyme inhibitor”
- Download figure
- Open in new tab
- Download powerpoint

Fig 2 Example of a specific literature search. The search terms used were “angiotensin converting enzyme inhibitor” and “hypertension.” The limits applied to this search were all randomised controlled trials carried out in humans, published in English over the past 10 years, with the search terms appearing in the title of the study only

Fig 3 Results from a specific literature search (using the search terms and limits from figure 2)
Reading the abstracts (study summary) of the articles identified in your search may help you decide whether the study is applicable for your review—for example, the work may have been carried out using an animal model rather than in humans. After excluding any inappropriate articles, you need to obtain the full articles of studies you have identified. Additional relevant articles that may not have come up in your original search can also be found by searching the reference lists of the articles you have already obtained. Once again, you may find that some articles are still not applicable for your review, and these can also be excluded at this stage. It is important to explain in your final review what criteria you used to exclude articles as well as those criteria used for inclusion.
The National Institute for Health and Clinical Excellence (NICE) publishes evidence based guidelines for the United Kingdom and therefore provides an additional resource for identifying the relevant literature in a particular field. 4 NICE critically appraises the published literature with recommendations for best clinical practice proposed and graded based on the quality of evidence available. Similarly, there are internationally published evidence based guidelines, such as those produced by the European Society of Cardiology and the American College of Chest Physicians, which can be useful when collecting the literature in a particular field. 5 6
Appraising the evidence
Once you have collected the evidence, you need to critically appraise the published material. Box 1 gives definitions of terms you will encounter when reading the literature. A brief guide of how to critically appraise a study is presented; however, it is advisable to consult the references cited for further details.
Box 1: Definitions of common terms in the literature 7
Prospective—collecting data in real time after the study is designed
Retrospective—analysis of data that have already been collected to determine associations between exposure and outcome
Hypothesis—proposed association between exposure and outcome. If presented in the negative it is called the null hypothesis
Variable—a quantity or quality that changes during the study and can be measured
Single blind—subjects are unaware of their treatment, but clinicians are aware
Double blind—both subjects and clinicians are unaware of treatment given
Placebo—a simulated medical intervention, with subjects not receiving the specific intervention or treatment being studied
Outcome measure/endpoint—clinical variable or variables measured in a study subsequently used to make conclusions about the original interventions or treatments administered
Bias—difference between reported results and true results. Many types exist (such as selection, allocation, and reporting biases)
Probability (P) value—number between 0 and 1 providing the likelihood the reported results occurred by chance. A P value of 0.05 means there is a 5% likelihood that the reported result occurred by chance
Confidence intervals—provides a range between two numbers within which one can be certain the results lie. A confidence interval of 95% means one can be 95% certain the actual results lie within the reported range
The study authors should clearly define their research question and ideally the hypothesis to be tested. If the hypothesis is presented in the negative, it is called the null hypothesis. An example of a null hypothesis is smoking does not cause lung cancer. The study is then performed to assess the significance of the exposure (smoking) on outcome (lung cancer).
A major part of the critical appraisal process is to focus on study methodology, with your key task being an assessment of the extent to which a study was susceptible to bias (the discrepancy between the reported results and the true results). It should be clear from the methods what type of study was performed (box 2).
Box 2: Different study types 7
Systematic review/meta-analysis—comprehensive review of published literature using predefined methodology. Meta-analyses combine results from various studies to give numerical data for the overall association between variables
Randomised controlled trial—random allocation of patients to one of two or more groups. Used to test a new drug or procedure
Cohort study—two or more groups followed up over a long period, with one group exposed to a certain agent (drug or environmental agent) and the other not exposed, with various outcomes compared. An example would be following up a group of smokers and a group of non-smokers with the outcome measure being the development of lung cancer
Case-control study—cases (those with a particular outcome) are matched as closely as possible (for age, sex, ethnicity) with controls (those without the particular outcome). Retrospective data analysis is performed to determine any factors associated with developing the particular outcomes
Cross sectional study—looks at a specific group of patients at a single point in time. Effectively a survey. An example is asking a group of people how many of them drink alcohol
Case report—detailed reports concerning single patients. Useful in highlighting adverse drug reactions
There are many different types of bias, which depend on the particular type of study performed, and it is important to look for these biases. Several published checklists are available that provide excellent resources to help you work through the various studies and identify sources of bias. The CONSORT statement (which stands for CONsolidated Standards Of Reporting Trials) provides a minimum set of recommendations for reporting randomised controlled trials and comprises a rigorous 25 item checklist, with variations available for other study types. 8 9 As would be expected, most (17 of 25) of the items focus on questions relating to the methods and results of the randomised trial. The remaining items relate to the title, abstract, introduction, and discussion of the study, in addition to questions on trial registration, protocol, and funding.
Jadad scoring provides a simple and validated system to assess the methodological quality of a randomised clinical trial using three questions. 10 The score ranges from zero to five, with one point given for a “yes” in each of the following questions. (1) Was the study described as randomised? (2) Was the study described as double blind? (3) Were there details of subject withdrawals, exclusions, and dropouts? A further point is given if (1) the method of randomisation was appropriate, and (2) the method of blinding was appropriate.
In addition, the Critical Appraisal Skills Programme provides excellent tools for assessing the evidence in all study types (box 2). 11 The Oxford Centre for Evidence-Based Medicine levels of evidence is yet another useful resource for assessing the methodological quality of all studies. 12
Ensure all patients have been accounted for and any exclusions, for whatever reason, are reported. Knowing the baseline demographic (age, sex, ethnicity) and clinical characteristics of the population is important. Results are usually reported as probability values or confidence intervals (box 1).
This should explain the major study findings, put the results in the context of the published literature, and attempt to account for any variations from previous work. Study limitations and sources of bias should be discussed. Authors’ conclusions should be supported by the study results and not unnecessarily extrapolated. For example, a treatment shown to be effective in animals does not necessarily mean it will work in humans.
The format for writing up the literature review usually consists of an abstract (short structured summary of the review), the introduction or background, methods, results, and discussion with conclusions. There are a number of good examples of how to structure a literature review and these can be used as an outline when writing your review. 13 14
The introduction should identify the specific research question you intend to address and briefly put this into the context of the published literature. As you have now probably realised, the methods used for the review must be clear to the reader and provide the necessary detail for someone to be able to reproduce the search. The search strategy needs to include a list of keywords used, which databases were searched, and the specific search limits or filters applied. Any grading of methodological quality, such as the CONSORT statement or Jadad scoring, must be explained in addition to any study inclusion or exclusion criteria. 6 7 8 The methods also need to include a section on the data collected from each of the studies, the specific outcomes of interest, and any statistical analysis used. The latter point is usually relevant only when performing meta-analyses.
The results section must clearly show the process of filtering down from the articles obtained from the original search to the final studies included in the review—that is, accounting for all excluded studies. A flowchart is usually best to illustrate this. Next should follow a brief description of what was done in the main studies, the number of participants, the relevant results, and any potential sources of bias. It is useful to group similar studies together as it allows comparisons to be made by the reader and saves repetition in your write-up. Boxes and figures should be used appropriately to illustrate important findings from the various studies.
Finally, in the discussion you need to consider the study findings in light of the methodological quality—that is, the extent of potential bias in each study that may have affected the study results. Using the evidence, you need to make conclusions in your review, and highlight any important gaps in the evidence base, which need to be dealt with in future studies. Working through drafts of the literature review with your supervisor will help refine your critical appraisal skills and the ability to present information concisely in a structured review article. Remember, if the work is good it may get published.
Originally published as: Student BMJ 2012;20:e404
Competing interests: None declared.
Provenance and peer review: Not commissioned; externally peer reviewed.
- ↵ The Cochrane Library. www3.interscience.wiley.com/cgibin/mrwhome/106568753/HOME?CRETRY=1&SRETRY=0 .
- ↵ British Medical Journal . www.bmj.com/ .
- ↵ Heran BS, Wong MMY, Heran IK, Wright JM. Blood pressure lowering efficacy of angiotensin converting enzyme (ACE) inhibitors for primary hypertension. Cochrane Database Syst Rev 2008 ; 4 : CD003823 , doi: 10.1002/14651858.CD003823.pub2. OpenUrl PubMed
- ↵ National Institute for Health and Clinical Excellence. www.nice.org.uk .
- ↵ European Society of Cardiology. www.escardio.org/guidelines .
- ↵ Geerts WH, Bergqvist D, Pineo GF, Heit JA, Samama CM, Lassen MR, et al. Prevention of venous thromboembolism: American College of Chest Physicians evidence-based clinical practice guidelines (8th ed). Chest 2008 ; 133 : 381 -453S. OpenUrl CrossRef
- ↵ Wikipedia. http://en.wikipedia.org/wiki .
- ↵ Moher D, Schulz KF, Altman DG, Egger M, Davidoff F, Elbourne D, et al. The CONSORT statement: revised recommendations for improving the quality of reports of parallel-group randomised trials. Lancet 2001 ; 357 : 1191 -4. OpenUrl CrossRef PubMed Web of Science
- ↵ The CONSORT statement. www.consort-statement.org/ .
- ↵ Jadad AR, Moore RA, Carroll D, Jenkinson C, Reynolds DJ, Gavaghan DJ, et al. Assessing the quality of reports of randomized clinical trials: is blinding necessary? Control Clin Trials 1996 ; 17 : 1 -12. OpenUrl CrossRef PubMed Web of Science
- ↵ Critical Appraisal Skills Programme (CASP). www.sph.nhs.uk/what-we-do/public-health-workforce/resources/critical-appraisals-skills-programme .
- ↵ Oxford Centre for Evidence-based Medicine—Levels of Evidence. www.cebm.net .
- ↵ Van den Bruel A, Thompson MJ, Haj-Hassan T, Stevens R, Moll H, Lakhanpaul M, et al . Diagnostic value of laboratory tests in identifying serious infections in febrile children: systematic review. BMJ 2011 ; 342 : d3082 . OpenUrl Abstract / FREE Full Text
- ↵ Awopetu AI, Moxey P, Hinchliffe RJ, Jones KG, Thompson MM, Holt PJ. Systematic review and meta-analysis of the relationship between hospital volume and outcome for lower limb arterial surgery. Br J Surg 2010 ; 97 : 797 -803. OpenUrl CrossRef PubMed
- University of Detroit Mercy
- Health Professions
Health Services Administration
- Writing a Literature Review
- Find Articles (Databases)
- Evidence-based Practice
- eBooks & Articles
- General Writing Support
- Creating & Printing Posters
- Research Project Web Resources
- Statistics: Health / Medical
- Searching Tips
- Streaming Video
- Database & Library Help
- Medical Apps & Mobile Sites
- Faculty Publications
Literature Review Overview
What is a Literature Review? Why Are They Important?
A literature review is important because it presents the "state of the science" or accumulated knowledge on a specific topic. It summarizes, analyzes, and compares the available research, reporting study strengths and weaknesses, results, gaps in the research, conclusions, and authors’ interpretations.
Tips and techniques for conducting a literature review are described more fully in the subsequent boxes:
- Literature review steps
- Strategies for organizing the information for your review
- Literature reviews sections
- In-depth resources to assist in writing a literature review
- Templates to start your review
- Literature review examples
Literature Review Steps

Graphic used with permission: Torres, E. Librarian, Hawai'i Pacific University
1. Choose a topic and define your research question
- Try to choose a topic of interest. You will be working with this subject for several weeks to months.
- Ideas for topics can be found by scanning medical news sources (e.g MedPage Today), journals / magazines, work experiences, interesting patient cases, or family or personal health issues.
- Do a bit of background reading on topic ideas to familiarize yourself with terminology and issues. Note the words and terms that are used.
- Develop a focused research question using PICO(T) or other framework (FINER, SPICE, etc - there are many options) to help guide you.
- Run a few sample database searches to make sure your research question is not too broad or too narrow.
- If possible, discuss your topic with your professor.
2. Determine the scope of your review
The scope of your review will be determined by your professor during your program. Check your assignment requirements for parameters for the Literature Review.
- How many studies will you need to include?
- How many years should it cover? (usually 5-7 depending on the professor)
- For the nurses, are you required to limit to nursing literature?
3. Develop a search plan
- Determine which databases to search. This will depend on your topic. If you are not sure, check your program specific library website (Physician Asst / Nursing / Health Services Admin) for recommendations.
- Create an initial search string using the main concepts from your research (PICO, etc) question. Include synonyms and related words connected by Boolean operators
- Contact your librarian for assistance, if needed.
4. Conduct searches and find relevant literature
- Keep notes as you search - tracking keywords and search strings used in each database in order to avoid wasting time duplicating a search that has already been tried
- Read abstracts and write down new terms to search as you find them
- Check MeSH or other subject headings listed in relevant articles for additional search terms
- Scan author provided keywords if available
- Check the references of relevant articles looking for other useful articles (ancestry searching)
- Check articles that have cited your relevant article for more useful articles (descendancy searching). Both PubMed and CINAHL offer Cited By links
- Revise the search to broaden or narrow your topic focus as you peruse the available literature
- Conducting a literature search is a repetitive process. Searches can be revised and re-run multiple times during the process.
- Track the citations for your relevant articles in a software citation manager such as RefWorks, Zotero, or Mendeley
5. Review the literature
- Read the full articles. Do not rely solely on the abstracts. Authors frequently cannot include all results within the confines of an abstract. Exclude articles that do not address your research question.
- While reading, note research findings relevant to your project and summarize. Are the findings conflicting? There are matrices available than can help with organization. See the Organizing Information box below.
- Critique / evaluate the quality of the articles, and record your findings in your matrix or summary table. Tools are available to prompt you what to look for. (See Resources for Appraising a Research Study box on the HSA, Nursing , and PA guides )
- You may need to revise your search and re-run it based on your findings.
6. Organize and synthesize
- Compile the findings and analysis from each resource into a single narrative.
- Using an outline can be helpful. Start broad, addressing the overall findings and then narrow, discussing each resource and how it relates to your question and to the other resources.
- Cite as you write to keep sources organized.
- Write in structured paragraphs using topic sentences and transition words to draw connections, comparisons, and contrasts.
- Don't present one study after another, but rather relate one study's findings to another. Speak to how the studies are connected and how they relate to your work.
Organizing Information
Options to assist in organizing sources and information :
1. Synthesis Matrix
- helps provide overview of the literature
- information from individual sources is entered into a grid to enable writers to discern patterns and themes
- article summary, analysis, or results
- thoughts, reflections, or issues
- each reference gets its own row
- mind maps, concept maps, flowcharts
- at top of page record PICO or research question
- record major concepts / themes from literature
- list concepts that branch out from major concepts underneath - keep going downward hierarchically, until most specific ideas are recorded
- enclose concepts in circles and connect the concept with lines - add brief explanation as needed
3. Summary Table
- information is recorded in a grid to help with recall and sorting information when writing
- allows comparing and contrasting individual studies easily
- purpose of study
- methodology (study population, data collection tool)
Efron, S. E., & Ravid, R. (2019). Writing the literature review : A practical guide . Guilford Press.
Literature Review Sections
- Lit reviews can be part of a larger paper / research study or they can be the focus of the paper
- Lit reviews focus on research studies to provide evidence
- New topics may not have much that has been published
* The sections included may depend on the purpose of the literature review (standalone paper or section within a research paper)
Standalone Literature Review (aka Narrative Review):
- presents your topic or PICO question
- includes the why of the literature review and your goals for the review.
- provides background for your the topic and previews the key points
- Narrative Reviews: tmay not have an explanation of methods.
- include where the search was conducted (which databases) what subject terms or keywords were used, and any limits or filters that were applied and why - this will help others re-create the search
- describe how studies were analyzed for inclusion or exclusion
- review the purpose and answer the research question
- thematically - using recurring themes in the literature
- chronologically - present the development of the topic over time
- methodological - compare and contrast findings based on various methodologies used to research the topic (e.g. qualitative vs quantitative, etc.)
- theoretical - organized content based on various theories
- provide an overview of the main points of each source then synthesize the findings into a coherent summary of the whole
- present common themes among the studies
- compare and contrast the various study results
- interpret the results and address the implications of the findings
- do the results support the original hypothesis or conflict with it
- provide your own analysis and interpretation (eg. discuss the significance of findings; evaluate the strengths and weaknesses of the studies, noting any problems)
- discuss common and unusual patterns and offer explanations
- stay away from opinions, personal biases and unsupported recommendations
- summarize the key findings and relate them back to your PICO/research question
- note gaps in the research and suggest areas for further research
- this section should not contain "new" information that had not been previously discussed in one of the sections above
- provide a list of all the studies and other sources used in proper APA 7
Literature Review as Part of a Research Study Manuscript:
- Compares the study with other research and includes how a study fills a gap in the research.
- Focus on the body of the review which includes the synthesized Findings and Discussion
Literature Reviews vs Systematic Reviews
Systematic Reviews are NOT the same as a Literature Review:
Literature Reviews:
- Literature reviews may or may not follow strict systematic methods to find, select, and analyze articles, but rather they selectively and broadly review the literature on a topic
- Research included in a Literature Review can be "cherry-picked" and therefore, can be very subjective
Systematic Reviews:
- Systemic reviews are designed to provide a comprehensive summary of the evidence for a focused research question
- rigorous and strictly structured, using standardized reporting guidelines (e.g. PRISMA, see link below)
- uses exhaustive, systematic searches of all relevant databases
- best practice dictates search strategies are peer reviewed
- uses predetermined study inclusion and exclusion criteria in order to minimize bias
- aims to capture and synthesize all literature (including unpublished research - grey literature) that meet the predefined criteria on a focused topic resulting in high quality evidence
Literature Review Examples
- Breastfeeding initiation and support: A literature review of what women value and the impact of early discharge (2017). Women and Birth : Journal of the Australian College of Midwives
- Community-based participatory research to promote healthy diet and nutrition and prevent and control obesity among African-Americans: A literature review (2017). Journal of Racial and Ethnic Health Disparities
- Vitamin D deficiency in individuals with a spinal cord injury: A literature review (2017). Spinal Cord
Resources for Writing a Literature Review
These sources have been used in developing this guide.
Resources Used on This Page
Aveyard, H. (2010). Doing a literature review in health and social care : A practical guide . McGraw-Hill Education.
Purdue Online Writing Lab. (n.d.). Writing a literature review . Purdue University. https://owl.purdue.edu/owl/research_and_citation/conducting_research/writing_a_literature_review.html
Torres, E. (2021, October 21). Nursing - graduate studies research guide: Literature review. Hawai'i Pacific University Libraries. Retrieved January 27, 2022, from https://hpu.libguides.com/c.php?g=543891&p=3727230
- << Previous: General Writing Support
- Next: Creating & Printing Posters >>
- Last Updated: Apr 19, 2024 3:11 PM
- URL: https://udmercy.libguides.com/hsa
Dissecting the fatigue experience: A scoping review of fatigue definitions, dimensions, and measures in non-oncologic medical conditions
Affiliation.
- 1 National Institute of Nursing Research, National Institutes of Health, Bethesda, MD, USA.
- PMID: 34589772
- PMCID: PMC8474156
- DOI: 10.1016/j.bbih.2021.100266
Introduction: Fatigue is a prevalent and potentially debilitating symptom that impacts the health-related quality-of-life of individuals diagnosed with acute and chronic medical conditions. Yet, its etiologic mechanism is not fully understood. Additionally, the assessment and determination of the clinical meaning of fatigue and its multidimensionality may vary by medical condition.
Methods: A scoping literature review was conducted to investigate how fatigue is defined and measured, including its dimensions, in non-oncologic medical conditions. The PubMed database was searched using keywords.
Results: Overall, 8376 articles were screened at the title/abstract levels, where 293 articles were chosen for full-text review that mentioned fatigue or included fatigue measures. The review of the full text excluded 246 articles that did not assess at least one fatigue dimension using validated questionnaires and clinical tests. The final set included 47 articles. Physical fatigue was the most assessed fatigue dimension and the Multidimensional Fatigue Inventory was the most widely used questionnaire to assess fatigue in this review.
Limitations: This review was limited by including only English-language publications and using PubMed as the sole database for the search.
Conclusions: This review affirms that fatigue is a multidimensional construct, agnostic of medical condition, and that individual fatigue dimensions can be measured by validated clinical measures. Future research should focus on expanding the repertoire of clinical measures to assess specific fatigue dimensions.
Keywords: Clinical measure; Fatigue; Fatigue assessment; Fatigue dimension.
Publication types
Health (Nursing, Medicine, Allied Health)
- Find Articles/Databases
- Reference Resources
- Evidence Summaries & Clinical Guidelines
- Drug Information
- Health Data & Statistics
- Patient/Consumer Facing Materials
- Images and Streaming Video
- Grey Literature
- Mobile Apps & "Point of Care" Tools
- Tests & Measures This link opens in a new window
- Citing Sources
- Selecting Databases
- Framing Research Questions
- Crafting a Search
- Narrowing / Filtering a Search
- Expanding a Search
- Cited Reference Searching
- Saving Searches
- Term Glossary
- Critical Appraisal Resources
- What are Literature Reviews?
- Conducting & Reporting Systematic Reviews
- Finding Systematic Reviews
- Tutorials & Tools for Literature Reviews
- Finding Full Text
What are Systematic Reviews? (3 minutes, 24 second YouTube Video)
Systematic Literature Reviews: Steps & Resources
These steps for conducting a systematic literature review are listed below .
Also see subpages for more information about:
- The different types of literature reviews, including systematic reviews and other evidence synthesis methods
- Tools & Tutorials
Literature Review & Systematic Review Steps
- Develop a Focused Question
- Scope the Literature (Initial Search)
- Refine & Expand the Search
- Limit the Results
- Download Citations
- Abstract & Analyze
- Create Flow Diagram
- Synthesize & Report Results
1. Develop a Focused Question
Consider the PICO Format: Population/Problem, Intervention, Comparison, Outcome
Focus on defining the Population or Problem and Intervention (don't narrow by Comparison or Outcome just yet!)
"What are the effects of the Pilates method for patients with low back pain?"
Tools & Additional Resources:
- PICO Question Help
- Stillwell, Susan B., DNP, RN, CNE; Fineout-Overholt, Ellen, PhD, RN, FNAP, FAAN; Melnyk, Bernadette Mazurek, PhD, RN, CPNP/PMHNP, FNAP, FAAN; Williamson, Kathleen M., PhD, RN Evidence-Based Practice, Step by Step: Asking the Clinical Question, AJN The American Journal of Nursing : March 2010 - Volume 110 - Issue 3 - p 58-61 doi: 10.1097/01.NAJ.0000368959.11129.79
2. Scope the Literature
A "scoping search" investigates the breadth and/or depth of the initial question or may identify a gap in the literature.
Eligible studies may be located by searching in:
- Background sources (books, point-of-care tools)
- Article databases
- Trial registries
- Grey literature
- Cited references
- Reference lists
When searching, if possible, translate terms to controlled vocabulary of the database. Use text word searching when necessary.
Use Boolean operators to connect search terms:
- Combine separate concepts with AND (resulting in a narrower search)
- Connecting synonyms with OR (resulting in an expanded search)
Search: pilates AND ("low back pain" OR backache )
Video Tutorials - Translating PICO Questions into Search Queries
- Translate Your PICO Into a Search in PubMed (YouTube, Carrie Price, 5:11)
- Translate Your PICO Into a Search in CINAHL (YouTube, Carrie Price, 4:56)
3. Refine & Expand Your Search
Expand your search strategy with synonymous search terms harvested from:
- database thesauri
- reference lists
- relevant studies
Example:
(pilates OR exercise movement techniques) AND ("low back pain" OR backache* OR sciatica OR lumbago OR spondylosis)
As you develop a final, reproducible strategy for each database, save your strategies in a:
- a personal database account (e.g., MyNCBI for PubMed)
- Log in with your NYU credentials
- Open and "Make a Copy" to create your own tracker for your literature search strategies
4. Limit Your Results
Use database filters to limit your results based on your defined inclusion/exclusion criteria. In addition to relying on the databases' categorical filters, you may also need to manually screen results.
- Limit to Article type, e.g.,: "randomized controlled trial" OR multicenter study
- Limit by publication years, age groups, language, etc.
NOTE: Many databases allow you to filter to "Full Text Only". This filter is not recommended . It excludes articles if their full text is not available in that particular database (CINAHL, PubMed, etc), but if the article is relevant, it is important that you are able to read its title and abstract, regardless of 'full text' status. The full text is likely to be accessible through another source (a different database, or Interlibrary Loan).
- Filters in PubMed
- CINAHL Advanced Searching Tutorial
5. Download Citations
Selected citations and/or entire sets of search results can be downloaded from the database into a citation management tool. If you are conducting a systematic review that will require reporting according to PRISMA standards, a citation manager can help you keep track of the number of articles that came from each database, as well as the number of duplicate records.
In Zotero, you can create a Collection for the combined results set, and sub-collections for the results from each database you search. You can then use Zotero's 'Duplicate Items" function to find and merge duplicate records.

- Citation Managers - General Guide
6. Abstract and Analyze
- Migrate citations to data collection/extraction tool
- Screen Title/Abstracts for inclusion/exclusion
- Screen and appraise full text for relevance, methods,
- Resolve disagreements by consensus
Covidence is a web-based tool that enables you to work with a team to screen titles/abstracts and full text for inclusion in your review, as well as extract data from the included studies.

- Covidence Support
- Critical Appraisal Tools
- Data Extraction Tools
7. Create Flow Diagram
The PRISMA (Preferred Reporting Items for Systematic reviews and Meta-Analyses) flow diagram is a visual representation of the flow of records through different phases of a systematic review. It depicts the number of records identified, included and excluded. It is best used in conjunction with the PRISMA checklist .

Example from: Stotz, S. A., McNealy, K., Begay, R. L., DeSanto, K., Manson, S. M., & Moore, K. R. (2021). Multi-level diabetes prevention and treatment interventions for Native people in the USA and Canada: A scoping review. Current Diabetes Reports, 2 (11), 46. https://doi.org/10.1007/s11892-021-01414-3
- PRISMA Flow Diagram Generator (ShinyApp.io, Haddaway et al. )
- PRISMA Diagram Templates (Word and PDF)
- Make a copy of the file to fill out the template
- Image can be downloaded as PDF, PNG, JPG, or SVG
- Covidence generates a PRISMA diagram that is automatically updated as records move through the review phases
8. Synthesize & Report Results
There are a number of reporting guideline available to guide the synthesis and reporting of results in systematic literature reviews.
It is common to organize findings in a matrix, also known as a Table of Evidence (ToE).

- Reporting Guidelines for Systematic Reviews
- Download a sample template of a health sciences review matrix (GoogleSheets)
Steps modified from:
Cook, D. A., & West, C. P. (2012). Conducting systematic reviews in medical education: a stepwise approach. Medical Education , 46 (10), 943–952.
- << Previous: Critical Appraisal Resources
- Next: What are Literature Reviews? >>
- Last Updated: Apr 18, 2024 3:22 PM
- URL: https://guides.nyu.edu/health

- Collections
- Recent Additions
- Public Access
- Submit Content
- home Rosa P
The Effects of Medical Conditions on Driving Performance: A Literature Review and Synthesis
Search our Collections & Repository
- Advanced Search
- Custom Query
All these words:
For very narrow results
This exact word or phrase:
When looking for a specific result
Any of these words:
Best used for discovery & interchangable words
None of these words:
Recommended to be used in conjunction with other fields
Publication Date Range:
Document Type:
Collection:
Query Builder
For additional assistance using the Custom Query please check out our Help Page
- By Lococo, Kathy H. ; Staplin, Loren ; Schultz, Matthew W.
- Creators: Lococo, Kathy H. ; Staplin, Loren ; Schultz, Matthew W. Lococo, Kathy H. ; Staplin, Loren ; Schultz, Matthew W. Less -
- Corporate Creators: TransAnalytics, LLC
- Corporate Contributors: United States. National Highway Traffic Safety Administration. Office of Behavioral Safety Research
- Subject/TRT Terms: [+] Aged Drivers Aging (Biology) Diseases And Medical Conditions Driver Performance Functional Ability Highways Highway Safety Literature Reviews Safety Safety And Human Factors
- Publication/ Report Number: DOT HS 812 526
- DOI: https://doi.org/10.21949/1525955
- Resource Type: Tech Report
- Geographical Coverage: United States
- Edition: Final Report
- Contracting Officer: Sifrit, Kathy
- Corporate Publisher: United States. Department of Transportation. National Highway Traffic Safety Administration
- Abstract: This literature review relates changes in performance or safety outcome measures for older drivers to their medical conditions or medication use, and associated functional impairments. It was carried out as an initial task in the project, The Effects of Medical Conditions on Driving Performance. Researchers conducted a search of peer-reviewed journals, technical reports, and government reports that bear on medical fitness to drive, published between 2000 through 2011. Results were integrated with knowledge gained through a prior, exhaustive literature review carried out under the NHTSA project, Taxonomy of Older Driver Behaviors and Crash Risk, to produce a synthesis that considered the prevalence within the U.S. population, effects on the functional abilities needed for safe driving, effects on driving performance, and relationships with motor vehicle crash and violation risk. Researchers prioritized diabetes, dementia, glaucoma, hepatic encephalopathy, macular degeneration, obstructive sleep apnea, Parkinson’s disease, and stroke in terms of the potential for impaired performance and crash risk among older drivers. More ▼ -->
- Format: PDF
- Funding: DTNH2209D00135, Task Order No.04
- Collection(s): NHTSA - Behavioral Safety Research
- Main Document Checksum: [+] urn:sha256:5ee531cc798ba75f3094fb13e7c1083b541a32d77638eb46c4f048b3d36cc4cd
- Download URL: https://rosap.ntl.bts.gov/view/dot/38687/dot_38687_DS1.pdf
Supporting Files
You may also like.
Checkout today's featured content at rosap.ntl.bts.gov
Exit Notification/Disclaimer Policy
Thank you for visiting.
You are about to access a non-government link outside of the U.S. Department of Transportation's National Transportation Library.
Please note: While links to Web sites outside of DOT are offered for your convenience, when you exit DOT Web sites, Federal privacy policy and Section 508 of the Rehabilitation Act (accessibility requirements) no longer apply. In addition, DOT does not attest to the accuracy, relevance, timeliness or completeness of information provided by linked sites. Linking to a Web site does not constitute an endorsement by DOT of the sponsors of the site or the products presented on the site. For more information, please view DOT's Web site linking policy.
To get back to the page you were previously viewing, click your Cancel button.
U.S. DEPARTMENT OF TRANSPORTATION
Bureau of Transportation Statistics
1200 NEW JERSEY AVENUE, SE
WASHINGTON, DC 20590
800-853-1351
Subscribe to email updates
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- Springer Nature - PMC COVID-19 Collection

Artificial intelligence in disease diagnosis: a systematic literature review, synthesizing framework and future research agenda
Yogesh kumar.
1 Department of Computer Engineering, Indus Institute of Technology and Engineering, Indus University, Ahmedabad, 382115 India
Apeksha Koul
2 Shri Mata Vaishno Devi University, Jammu, India
Ruchi Singla
3 Department of Research, Innovations, Sponsored Projects and Entrepreneurship, CGC Landran, Mohali, India
Muhammad Fazal Ijaz
4 Department of Intelligent Mechatronics Engineering, Sejong University, Seoul, 05006 South Korea
Artificial intelligence can assist providers in a variety of patient care and intelligent health systems. Artificial intelligence techniques ranging from machine learning to deep learning are prevalent in healthcare for disease diagnosis, drug discovery, and patient risk identification. Numerous medical data sources are required to perfectly diagnose diseases using artificial intelligence techniques, such as ultrasound, magnetic resonance imaging, mammography, genomics, computed tomography scan, etc. Furthermore, artificial intelligence primarily enhanced the infirmary experience and sped up preparing patients to continue their rehabilitation at home. This article covers the comprehensive survey based on artificial intelligence techniques to diagnose numerous diseases such as Alzheimer, cancer, diabetes, chronic heart disease, tuberculosis, stroke and cerebrovascular, hypertension, skin, and liver disease. We conducted an extensive survey including the used medical imaging dataset and their feature extraction and classification process for predictions. Preferred reporting items for systematic reviews and Meta-Analysis guidelines are used to select the articles published up to October 2020 on the Web of Science, Scopus, Google Scholar, PubMed, Excerpta Medical Database, and Psychology Information for early prediction of distinct kinds of diseases using artificial intelligence-based techniques. Based on the study of different articles on disease diagnosis, the results are also compared using various quality parameters such as prediction rate, accuracy, sensitivity, specificity, the area under curve precision, recall, and F1-score.
Introduction
Healthcare is shaping up in front of our eyes with advances in digital healthcare technologies such as artificial intelligence (AI), 3D printing, robotics, nanotechnology, etc. Digitized healthcare presents numerous opportunities for reducing human errors, improving clinical outcomes, tracking data over time, etc. AI methods from machine learning to deep learning assume a crucial function in numerous well-being-related domains, including improving new clinical systems, patient information and records, and treating various illnesses (Usyal et al. 2020 ; Zebene et al. 2019 ). The AI techniques are also most efficient in identifying the diagnosis of different types of diseases. The presence of computerized reasoning (AI) as a method for improved medical services offers unprecedented occasions to recuperate patient and clinical group results, decrease costs, etc. The models used are not limited to computerization, such as providing patients, “family” (Musleh et al. 2019 ; Dabowsa et al. 2017 ), and medical service experts for data creation and suggestions as well as disclosure of data for shared evaluation building. AI can also help to recognize the precise demographics or environmental areas where the frequency of illness or high-risk behaviors exists. Researchers have effectively used deep learning classifications in diagnostic approaches to computing links between the built environment and obesity frequency (Bhatt et al. 2019 ; Plawiak et al. 2018 ).
AI algorithms must be trained on population-representative information to accomplish presentation levels essential for adaptable “accomplishment”. Trends, such as the charge for putting away and directing realities, information collection through electronic well-being records (Minaee et al. 2020 ; Kumar 2020 ), and exponential client state of information, have made a data-rich medical care biological system. This enlargement in health care data struggles with the lack of well-organized mechanisms for integrating and reconciling these data ahead of their current silos. However, numerous frameworks and principles facilitate summation and accomplish adequate data quantity for AI (Vasal et al. 2020 ). The challenges in the operational dynamism of AI technologies in healthcare systems are immeasurable despite the information that this is one of the most vital expansion areas in biomedical research (Kumar et al. 2020 ). The AI commune must build an integrated best practice method for execution and safeguarding by incorporating active best practices of principled inclusivity, software growth, implementation science, and individual–workstation interaction. At the same time, AI applications have an enormous ability to work on patient outcomes. Simultaneously, they could make significant hazards regarding inappropriate patient risk assessment, diagnostic inaccuracy, healing recommendations, privacy breaches, and other harms (Gouda et al. 2020 ; Khan and Member 2020 ).
Researchers have used various AI-based techniques such as machine and deep learning models to detect the diseases such as skin, liver, heart, alzhemier, etc. that need to be diagnosed early. Hence, in related work, the techniques like Boltzmann machine, K nearest neighbour (kNN), support vector machine (SVM), decision tree, logistic regression, fuzzy logic, and artificial neural network to diagnose the diseases are presented along with their accuracies. For example, a research study by Dabowsa et al. ( 2017 ) used a backpropagation neural network in diagnosing skin disease to achieve the highest level of accuracy. The authors used real-world data collected from the dermatology department. Ansari et al. ( 2011 ) used a recurrent neural network (RNN) to diagnose liver disease hepatitis virus and achieved 97.59%, while a feed-forward neural network achieved 100%. Owasis et al. ( 2019 ) got 97.057 area under the curve by using residual neural network and long short-term memory to diagnose gastrointestinal disease. Khan and Member ( 2020 ) introduced a computerized arrangement framework to recover the data designs. They proposed a five-phase machine learning pipeline that further arranged each stage in various sub levels. They built a classifier framework alongside information change and highlighted choice procedures inserted inside a test and information investigation plan. Skaane et al. ( 2013 ) enquired the property of digital breast tomosynthesis on period and detected cancer in residents based screening. They did a self-determining dual analysis examination by engaging ladies of 50–69 years and comparing full-field digitized mammography plus data building tool with full-field digital mammography. Accumulation of the data building tool resulted in a non-significant enhancement in sensitivity by 76.2% and a significant increase by 96.4%. Tigga et al. ( 2020 ) aimed to assess the diabetic risk among the patients based on their lifestyle, daily routines, health problems, etc. They experimented on 952 collected via an offline and online questionnaire. The same was applied to the Pima Indian Diabetes database. The random forest classifier stood out to be the best algorithm. Alfian et al. ( 2018 ) presented a personalized healthcare monitoring system using Bluetooth-based sensors and real-time data processing. It gathers the user’s vital signs data such as blood pressure, heart rate, weight, and blood glucose from sensor nodes to a smartphone. Katherine et al. ( 2019 ) gave an overview of the types of data encountered during the setting of chronic disease. Using various machine learning algorithms, they explained the extreme value theory to better quantify severity and risk in chronic disease. Gonsalves et al. ( 2019 ) aimed to predict coronary heart disease using historical medical data via machine learning technology. The presented work supported three supervised learning techniques named Naïve Bayes, Support vector machine, and Decision tree to find the correlations in coronary heart disease, which would help improve the prediction rate. The authors worked on the South African Heart Disease dataset of 462 instances and machine learning techniques using 10-fold cross-validation. Momin et al. ( 2019 ) proposed a secure internet of things-based healthcare system utilizing a body sensor network called body sensor network care to accomplish the requirements efficiently. The sensors used analogue to digital converter, Microcontroller, cloud database, network, etc. A study by Ijaz et al. ( 2018 ) has used IoT for a healthcare monitoring system for diabetes and hypertension patients at home and used personal healthcare devices that perceive and estimate a persons’ biomedical signals. The system can notify health personnel in real-time when patients experience emergencies. Shabut et al. ( 2018 ) introduced an examination to improve a smart, versatile, empowered master to play out a programmed discovery of tuberculosis. They applied administered AI method to achieve parallel grouping from eighteenth lower request shading minutes. Their test indicated a precision of 98.4%, particularly for the tuberculosis antigen explicit counteracting agent identification on the portable stage. Tran et al. ( 2019 ) provided the global trends and developments of artificial intelligence applications related to stroke and heart diseases to identify the research gaps and suggest future research directions. Matusoka et al. ( 2020 ) stated that the mindfulness, treatment, and control of hypertension are the most significant in overcoming stroke and cardiovascular infection. Rathod et al. ( 2018 ) proposed an automated image-based retrieval system for skin disease using machine learning classification. Srinivasu et al. ( 2021a , b ) proposed an effective model that can help doctors diagnose skin disease efficiently. The system combined neural networks with MobileNet V2 and Long Short Term Memory (LSTM) with an accuracy rate of 85%, exceeding other state-of-the-art deep models of deep learning neural networks. This system utilized the technique to analyse, process, and relegate the image data predicted based on various features. As a result, it gave more accuracy and generated faster results as compared to the traditional methods. Uehara et al. ( 2018 ) worked at the Japanese extremely chubby patients utilizing artificial brainpower with rule extraction procedure. They had 79 Non-alcoholic steatohepatitis, and 23 non- Non-alcoholic steatohepatitis patients analyse d to make the desired model. They accomplished the prescient exactness by 79.2%. Ijaz et al. ( 2020 ) propose a cervical cancer prediction model for early prediction of cervical cancer using risk factors as inputs. The authors utilize several machine learning approaches and outlier detection for different pre-processing tasks. Srinivasu et al. ( 2021a , b ) used an AW-HARIS algorithm to perform automated segmentation of CT scan images to identify abnormalities in the human liver. It is observed that the proposed approach has outperformed in the majority of the cases with an accuracy of 78%.
To fully understand how AI assists in the diagnosis and prediction of a disease, it is essential to understand the use and applicability of diverse techniques such as SVM, KNN, Naïve Bayes, Decision Tree, Ada Boost, Random Forest, K-Mean clustering, RNN, Convolutional neural networks (CNN), Deep-CNN, Generative Adversarial Networks (GAN), and Long short-term memory (LSTM) and many others for various disease detection system (Owasis et al. 2019 ; Nithya et al. 2020 ). We conducted an extensive survey based on the machine and deep learning models for disease diagnosis. The study covers the review of various diseases and their diagnostic methods using AI techniques. This contribution explains by addressing the four research questions: RQ1. What is the state-of-the-art research for AI in disease diagnosis? RQ2. What are the various types of diseases wherein AI is applied? RQ3. What are the emergent limitations and challenges that the literature advances for this research area? RQ4.What are the future avenues in healthcare that might benefit from the application of AI? The rest of the work is organized into various sections. Initially, a brief description of AI in healthcare and disease diagnosis using multiple machines and deep learning techniques is given in Sect. 1 . Then, it is named an introduction that includes Fig. 1 to describe all the papers taken from different organized sources for various diseases in the contribution sub-section. Materials and Methods is named as Sect. 2 , which includes the quality assessment and the investigation part regarding AI techniques and applications. Section 3 covers symptoms of diseases and challenges to diagnostics, a framework for AI in disease detection modelling, and various AI applications in healthcare. Section 4 includes the reported work of multiple diseases and the comparative analysis of different techniques with the used dataset, applied machine and deep learning methods with computed outcomes in terms of various parameters such as accuracy, sensitivity, specificity, the area under the curve, and F-score. In Sect. 5 , the discussion part is covered that answers the investigation part mentioned in Sect. 2 . Finally, in Sect. 6 , the work that helps researchers chooses the best approach for diagnosing the diseases is concluded along with the future scope.

Distribution of published papers for diseases diagnosis using artificial intelligence techniques

Contribution
Diseases usually are quantified by signs and symptoms. A sign is identified as an objective appearance of a disease that doctors can specify, whereas a symptom is a particular indication of the patient’s illness (Plawiak et al. 2018 ). Thus, every disease has various signs and symptoms, such as fever, which is found in countless conditions.
As shown in Fig. 1 , the number of papers reviewed under preferred reporting items for systematic reviews and Meta-Analysis (PRISMA) guidelines for different types of diseases using AI from the year 2009 to the year 2020. The present work emphasizes various diseases and their diagnostics measures using machine and deep learning classifications. To the best of our knowledge, most of the past work focused on disease diagnostics for one or two disease prediction systems. Hence, the present study explores ten different disease symptoms and their detection using AI techniques. Furthermore, this paper is unique, as it contains an elaborate discussion about various disease diagnoses and predictions based upon the extensive survey conducted for detection methods.
Materials and methods
We have directed this review according to the preferred reporting items for systematic reviews and Meta-Analysis guidelines. The survey offers the readers wide-ranging knowledge of the literature on AI (decision tree, which breaks down the dataset into smaller subsets and to build it, two types of entropy using frequencies are calculated in which X, S is a discrete random variable which occurs with probability p(i),…. p(c) and logarithm with base 2 gives the unit of bits or Shannons where entropy using the frequency table of one attribute is given as (Sabottke and Spieler 2020 )
and entropy using the frequency table of two attributes is given as
K-nearest neighbour algorithm is a supervised machine learning technique that is used to solve classification issues as well as to calculate the distance between the test data and the input to give the prediction by using Euclidean distance formula in which p, q are the two points in Euclidean n-space, and qi and pi are the Euclidean vectors starting from the origin of the space (Zaar et al. 2020 ).
Whereas regression is used to determine the relationship between independent and dependent variables. The equation Y represents it is equal to an X plus b, where Y is the dependent variable, an is the slope of the regression equation, x is the independent variable, and b is constant (Kolkur et al. 2018 )
where Y is the dependent variable, X is the independent variable; a is the intercept, b is the slope and is the residual error, Naïve Bayes which provides a way of calculating the posterior probability, P (c | x) from P(c), P(x) and P(x | c). Naïve Bayes classifier assumes that the effect of the value of an attribute (x) on a given class (c) is independent of the values of other predictors (Spann et al. 2020 )
P(c | x) is the posterior probability of class given attribute, P(x | c) is the likelihood which is the probability of the attribute given class, P(x) is the prior probability of attribute, P(c) is the prior probability of a class, k-means ( Fujita et al. 2020 ) which is used to define k centers, one for each cluster and these centres should be placed far away from each other. This algorithm also aims at minimizing an objective function which is known as squared error function, given by :
||x i -v j || is the Euclidean distance between x i -v j, Ci is the number of data points in ith cluster, C is the number of cluster center’s, convolution neural network which is a type of feed-forward artificial neural network in which the connectivity pattern between its neurons is inspired by the organization of the animal visual cortex. Convolution is the first step in the process that convolution neural network undergoes (Zhang et al. 2019 )
where (f*g)(t) = functions that are being convoluted, t = real number variable of functions f and g, g( τ ) = convolution of time function, τ ′ = first derivative of tau function, a recurrent neural network which is used for handling sequential data and its formula in which h(t) is a function f of the previously hidden state h(t − 1) and the current input x(t). The theta are the parameters of the function f is (Yang et al. 2020 )
Boltzmann machine, which optimizes the weights, a quantity related to the particular problem. Its main objective is to maximize the Consensus function (CF), which is given by the following formula (Zhou et al. 2019 )
where U i and U j are the set of units, w ij is the fixed weight, gradient descent which is an iterative process and is formulated by (Chang et al. 2018 )
where θ 1 is the next position, θ 0 is the current position, α is the small step, ∇ J θ is the direction of fastest increase) in healthcare (Zhang et al. 2017 ). The extensive survey also promotes expounding prevailing knowledge gaps and subsequent identification of paths for future research (Lin et al. 2019 ). The current study reformed the structure, which produced wide-ranging article valuation standards from earlier published articles. Articles incorporated in our research are selected using keywords like “Artificial Intelligence”, “Disease Detection”, “Disease diagnosis using machine learning”, “Disease diagnosis using deep learning”, “Artificial Intelligence in Healthcare”, and combinations of these keywords. In addition, research articles associated with the applications of AI-based techniques in predicting diseases and diagnosing them are incorporated for review. Table 1 lists the publications that are included or omitted based on a variety of criteria such as time, studies to define how old papers/articles can be accessed, the problem on which the article is based, comparative analysis of the work, methods to represent the techniques used, and research design to analyse the results that are obtained. These characteristics assisted us in carrying out the research study very quickly, without wasting time on irrelevant or unnecessary searches and investigations. The standards for inclusion and exclusion are developed by the requirements of the problem of an article.
Inclusion and exclusion parameters
Quality assessment
Research articles included in this review are identified using several quality evaluation constraints. The significance of the study is assessed based on inclusion and exclusion standards. All research articles included for review encompass machine or deep learning-based prediction models for automatically detecting and diagnosing diseases. Each research work incorporated in this study carried empirical research and had experimental outcomes. The description of these research articles is stated in a separate subsection entitled literature survey.
The comprehensive selection of research papers is carried out in four phases: (1) identifying where records are identified through various databases. At this phase, we must do the searches we’ve planned through the abstract and citation databases we’ve chosen. Take note of how many results the searches returned. We can also include data found in other places, such as Google Scholar or the reference lists of related papers. Then, in one citation management application, aggregate all of the records retrieved from the searches. Keep in mind that each database has its own set of rules for searching for terms of interest and combining keywords for a more efficient search. As a result, our search technique may vary significantly depending on the database, (2) screening the selection process is done transparently by reporting on decisions made at various stages of the systematic review. One of the investigators reviews the title and abstract of each record to see if the publication provides information that might be useful or relevant to the systematic review. In certain situations, the title and abstract screening is done by two investigators. They don’t split the job amongst themselves! Each investigator screens every title and abstract, and then their judgments are compared. If one of them decides to leave out an item that the other thinks should be included, they may go over the entire text together and come to a common conclusion. They can also enlist the help of a third party (usually the project manager or main investigator) to decide whether or not the study should be included. Make sure that the most acceptable justification for excluding an item is chosen. (3) Eligibility we study the complete contents of the articles that cleared the title and abstract screening to see whether they may assist in answering our research topic. Two investigators do this full-text screening. Each one examines the entire content of each article before deciding whether or not to include it. We must note the number of articles we remove and the number of articles under each cause for exclusion in the full-text screening, just as we did in the title/abstract screening. Hence, in this stage, full-text articles are assessed and then finally are included in qualitative analysis in (4) included phase by utilizing the Preferred reporting items for systematic reviews and meta-analysis (PRISMA) flowchart as depicted in Fig. 2 . In this stage, we’ll know how many papers will be included in our systematic review after removing irrelevant studies from the full-text screen. We assess how many of these studies may be included in a quantitative synthesis, commonly known as “meta-analysis,“ in the fourth and final screening stage.

PRISMA flow chart
To address the RQ1, RQ2, RQ3, and RQ4, the current survey examined the number of articles on different disease diagnoses using AI techniques from various data sources, including Psychological Information, Excerpta Medica Database, Google Scholar, PubMed, Scopus, and Web of Science. The above sources are popular sources of information for articles on AI in health informatics in previous studies. As previously explained, articles are chosen based on specified inclusion and exclusion criteria (Zhang et al. 2017 ). These were derived from (Behera et al. 2019 ), where the authors established and accepted the variations. To better understand the state of research on AI in disease detection, peer-reviewed papers are cited. The current review suggests that AI and healthcare have developed a present synergy.
Investigation
Investigation 1: Why do we need AI?
Investigation 2: What is the impact of AI on medical diagnosis and treatment?
Investigation 3: Why is AI important, and how is it used to analyse these diseases?
Investigation 4: Which AI-based algorithm is used in disease diagnosis?
Investigation 5: What are the challenges faced by the researchers while using AI models in several disease diagnoses?
Investigation 6: How are AI-based techniques helping doctors in diagnosing diseases?
Artificial intelligence in disease diagnosis
Detecting any irresistible ailment is nearly an afterward movement and forestalling its spread requires ongoing data and examination. Hence, acting rapidly with accurate data tosses a significant effect on the lives of individuals around the globe socially and financially (Minaee et al. 2020 ). The best thing about applying AI in health care is to improve from gathering and processing valuable data to programming surgeon robots. This section expounds on the various techniques and applications of artificial intelligence, disease symptoms, diagnostics issues, and a framework for disease detection modelling using learning models and AI in healthcare applications (Kumar and Singla 2021 ).
Framework for AI in disease detection modelling
AI describes the capability of a machine to study the way a human learns, e.g., through image identification and detecting pattern in a problematic situation. AI in health care alters how information gets composed, analysed, and developed for patient care (Ali et al. 2019 ).
System planning is the fundamental abstract design of the system. It includes the framework’s views, the course of action of the framework, and how the framework carries on underneath clear conditions. A solid grip of the framework design can help the client realize the limits and boundaries of the said framework. Figure 3 shows a pictorial portrayal of the ailment recognition model using utilitarian machines and profound learning classification strategies. In pre-preparing, real-world information requires upkeep and pre-preparing before being taken care of by the calculation (Jo et al. 2019 ). Because of the justifiable explanation, real-world data regularly contains mistakes regarding the utilized measures yet cannot practice such blunders. Accordingly, information pre-preparing takes this crude information, cycles it, eliminates errors, and spares it an extra examination. Information experiences a progression of steps during pre-handling (Chen et al. 2019a , b ): Information is purged by various strategies in information cleaning. These strategies involve gathering information, such as filling the information spaces that are left clear or decreasing information, such as the disposal of commas or other obscure characters. In information osmosis, the information is joined from a combination of sources. The information is then amended for any blend of mistakes, and they are quickly taken care of. Information Alteration : Data in this progression is standardized, which depends upon the given calculation. Information standardization can be executed utilizing several ways (Nasser et al. 2019 ). This progression is obligatory in most information mining calculations, as the information wants to be as perfect as possible. Information is then mutual and developed. Information Lessening : This progression in the strategy centers to diminish the information to more helpful levels. Informational collection and test information : The informational collection is segregated into parts preparing and testing informational indexes. The preparation information is utilized to gauge the actual examples of the data (Sarao et al. 2020 ). Equivalent to information needed for preparing and testing, experimental data is often replicated from a similar informational index. After the model has been pre-handled, the jiffy step is to test the accuracy of the framework. Systematic model : Analytical displaying strategies are utilized to calculate the probability of a given occurrence function given commitment factors, and it is very productive in illness expectation. It tends to imagine what the individual is experiencing in light of their info indications and prior determinations (Keenan et al. 2020 ; Rajalakshmi et al. 2018 ).

Framework for disease detection system
Medical imaging for diseases diagnosis
Clinical Imaging is seen to assign the arrangement of procedures that produce pictures of the inside part of the body. The procedure and cycles are used to take pictures of the human body for clinical purposes, such as uncovering, analysing, or looking at an injury, brokenness, and pathology (Bibault et al. 2020 ). Computed tomography (CT) scan outputs are great representations of helpful indicative imaging that encourages exact conclusion, mediation, and evaluation of harms and dysfunctions that actual advisors address consistently (Chen et al. 2017 ). Additional contemplates demonstrate overuse of Imaging, for example, X-rays or magnetic resonance imaging (MRI) for intense and complicated work, as shown in Table 2 .
Medical imaging types with their respective descriptions
Symptoms of diseases and challenges to diagnostics
The disease may be severe, persistent, cruel, or benign. Of these terms, persistent and severe have to do with the interval of a disease, lethal and begin with the potential for causing death. Additionally, different manifestations that may be irrelevant could post the warnings for more restorative severe illness or situation. The followings are a couple of diseases with their sign and indications for events:
- Heart assault signs incorporate hurt, nervousness, crushing, or feeling of breadth in the focal point of the chest that endures more than a couple of moments; agony or anxiety in different territories of the chest area; succinctness of breath; cold perspiration; heaving; or unsteadiness (Aggarwal et al. 2020 ).
- Stroke signs incorporate facial listing, arm shortcoming, the intricacy with discourse, quickly creating happiness or equalization, unexpected absence of sensation or weak point, loss of vision, puzzlement, or agonizing torment (Lukwanto et al. 2015 ).
- Reproductive wellbeing manages the signs that develop the issues such as blood misfortune or spotting between periods; tingling, copying, disturbance at genital region; agony or disquiet during intercourse; genuine or sore feminine dying; extreme pelvic/stomach torment; strange vaginal release; the sentiment of totality in the lower mid-region; and customary pee or urinary weight (Kather et al. 2019 ).
- Breast issue side effects include areola release, abnormal bosom delicacy or torment, bosom or areola skin changes, knot or thickening in or close to bosom or in the underarm zone (Memon et al. 2019 ).
- Lung issue side effects include hacking of blood, succinctness of breath, difficult breathing, consistent hack, rehashed episodes of bronchitis or pneumonia, and puffing (Ma et al. 2020 ).
- Stomach or stomach-related issue manifestations incorporate rectal dying, blood in the stool or dark stools, changes in gut properties or not having the option to control guts, stoppage, loose bowels, indigestion or heartburn, or spewing blood (Kather et al. 2019 ).
- Bladder issue manifestations include confounded or excruciating pee, incessant pee, loss of bladder control, blood in pee, waking routinely to pee around evening time to pee or wetting the bed around evening time, or spilling pee (Shkolyar et al. 2019 ).
- Skin issue indications remember changes for skin moles, repetitive flushing and redness of face and neck, jaundice, skin sores that do not disappear or re-establish to wellbeing, new development or moles on the skin, and thick, red skin with bright patches (Rodrigues et al. 2020 ).
- Emotional issues include nervousness, sadness, weariness, feeling tense, flashbacks and bad dreams, lack of engagement in daily exercises, self-destructive musings, mind flights, and fancies (Krittanawong et al. 2018 ).
- Headache issues indications (excluding ordinary strain cerebral pains) incorporate migraines that please unexpectedly, “the most noticeably awful migraine of your life”, and cerebral pain connected with extreme energy, queasiness, heaving, and powerlessness to walk (Mueller 2020 ).
Above, we have described the variety of illness signals and their symptoms. In contrast, illness recognition errors in medication are reasonably regular, can have a stringent penalty, and are only now the foundation to materialize outstandingly in patient safety. Here we have critical issues for various diagnostic types while detecting the particular diseases (Chuang 2011 ; Park et al. 2020 ).
- Analysis that is accidentally deferred wrong, or on the other hand, missed as decided from a definitive delight of more amazing data.
- Any fault or malfunction in the analytical course which is essential to a missed finding or a conceded conclusion comprises a breakdown in occasional admittance to mind; elicitation or comprehension of side effects, images, research facility result; detailing and weighing of difference investigation; and ideal development and strength arrangement or appraisal.
Healthcare applications
The healthcare system has long been an early adopter of generally innovative technologies. Today, artificial intelligence and its subset machine and deep learning are on their way to becoming a mean element in the healthcare system, from creating new health check actions to treat patient records and accounts. One of the maximum burdens physician practices today is the association and performance of organizational tasks (Fukuda et al. 2019 ). By automating them, healthcare institutions could help resolve the trouble and allow physicians to do their best, i.e., spend more time with patients. The following are the details of the artificial intelligence techniques in healthcare applications as shown in Table 3 :
Healthcare applications and their purpose
Reported work
This section highlights the best finding for different diseases with their diagnosis methods via machine and deep learning algorithms. It covers the extensive survey on various diseases such as alzheimer’s, cancer, diabetes, chronic, heart disease, tuberculosis, stroke and cerebrovascular, hypertension, skin and liver disease (Chui et al. 2020 ).
Diagnosis of Alzheimer’s disease
Alzheimer’s is a disease that worsens the dementia symptoms over several years (Zebene et al. 2019 ). During its early stage, it affects memory loss, but in the end, it loses the ability to carry the conservation and respond to the environment. Usyal et al. ( 2020 ) decided on the analysis of dementia in Alzheimer’s through investigating neuron pictures. They utilized the alzheimer’s disease neuroimaging initiative convention that comprises T1 weighted magnetic resonance information for finding. The prescient shows the precision estimated the characterization models, affectability, and explicitness esteem. Ljubic et al. ( 2020 ) presented the method to diagnose Alzheimer’s disease from electronic medical record (EMR) data. The results acquired showed the accuracy by 90% on using the SCRL dataset. Soundarya et al. ( 2020 ) proposed the methodology in which description of shrink brain tissue is used for the ancient analysis of Alzheimer’s disease. They have implemented various machine and deep learning algorithms. The deep algorithm has been considered the better solution provider to recognize the ailment at its primary stage with reasonable accuracy. Park et al. ( 2020 ) used a vast range of organizational health data to test the chance of machine learning models to expect the outlook occurrence of Alzheimer’s disease. Lin et al. ( 2019 ) proposed a method that used the spectrogram features extracted from speech data to identify Alzheimer’s disease. The system used the voice data collected via the internet of things (IoT) and transmitted to the cloud server where the original data is stored. The received data is used for training the model to identify the Alzheimer’s disease symptoms.
As seen in Fig. 4 , (Subasi 2020 ) proposed a broad framework for detecting Alzheimer’s illness using AI methods. The learning process is the process of optimizing model parameters using a training dataset or prior practice. Learning models can be predictive, predicting the future, descriptive, collecting data from input data sources, and combining them. Two critical stages are performed in machine learning and deep learning: pre-processing the vast input and improving the model. The second phase involves effectively testing the learning model and resembling the answer. Oh et al. ( 2019 ) offered a technique for demonstrating the end-to-end learning of four binary classification problems using a volumetric convolutional neural network form. The trials are performed on the ADNI database, and the results indicated that the suggested technique obtained an accuracy of 86.60% and a precision of 73.95%, respectively. Raza et al. ( 2019 ) proposed a unique AI-based examination and observation of Alzheimer’s disorder. The analysis results appeared at 82% improvement in contrast with notable existing procedures.

Alzheimer’s disease detection using artificial intelligence techniques (Subasi 2020 )
Additionally, above 95% precision is accomplished to order the exercises of everyday living, which are very reassuring regarding checking the action profile of the subject. Lodha et al. ( 2018 ) used a machine-learning algorithm to process the data obtained by neuroimaging technologies to detect Alzheimer’s in its primitive stage. It uses various algorithms like support vector machine (SVM), gradient boosting, K-nearest neighbour, Random forest, a neural network that shows the accuracy rate 97.56, 97.25, 95.00, 97.86, 98.36, respectively. Lei et al. ( 2020 ) state that to evaluate Alzheimer’s ailment, a clinical score forecast using neuroimaging data is incredibly profitable since it can adequately reveal the sickness status. The proposed structure comprises three sections: determination dependent on joint learning, highlight encoding dependent on profound polynomial arrange and amass learning for relapse through help vector relapse technique. Jo et al. ( 2019 ) performed the deep learning approach and neuroimaging data for the analytical classification of Alzheimer’s disease. Autoencoder for feature selection formed accuracy up to 98.8% and 83.7% for guessing conversion from mild cognitive impairment, a prodromal stage of Alzheimer’s disease.
A deep neural network uses neuroimaging data without pre-processing for feature collection that yields accuracies up to 96.0% for Alzheimer’s disease categorization and 84.2% for the medical council of India conversion problems (Oomman et al. 2018 ). Chen et al. ( 2017 ) hypothesized the combination of diffusivity and kurtosis in diffusion kurtosis imaging to increase the capacity of diffusion kurtosis imaging in detecting Alzheimer’s disease. The method was applied on the 53 subjects, including 27 Alzheimer’s patients, which provides an accuracy of 96.23%. Janghel et al. ( 2020 ) used a convolution neural network to improve classification accuracy. They demonstrated a deep learning technique for identifying Alzheimer’s disease using data from the Alzheimer’s disease neuroimaging initiative database, which included magnetic resonance imaging and positron emission tomography scan pictures of Alzheimer’s patients, as well as an image of a healthy individual. The experiment attained an average classification accuracy of 99.95% for the magnetic resonance imaging dataset and 73.46% for the positron emission tomography scan dataset. Balaji et al. ( 2020 ) presented the gait classification system based on machine learning to help the clinician diagnose the stage of Parkinson’s disease. They used four supervised machine learning algorithms: decision tree, support vector machine, ensemble classifier, and Bayes’ classifier, which are used for statistical and kinematic analysis that predict the severity of Parkinson’s disease.
Diagnosis of cancer disease
Artificial Intelligence methods can affect several facets of cancer therapy, including drug discovery, drug development, and the clinical validation of these drugs. Pradhan et al. ( 2020 ) evaluated several machine learning algorithms which are flexible for lung cancer recognition correlated with the internet of things. They reviewed various papers to predict different diseases using a machine learning algorithm. They also identified and depicted various research directions based on the existing methodologies. Memon et al. ( 2019 ) proposed an AI calculation-based symptomatic framework which adequately grouped the threatening and favorable individuals in the climate of the internet of things. They tried the proposed strategy on the Wisconsin Diagnostic Breast Cancer. They exhibited that the recursive element determination calculation chose the best subset of highlights and the classifier support vector machine that accomplished high order precision of 99% and affectability 98%, and Matthew’s coefficient is 99%. Das et al. ( 2019 ) proposed another framework called the watershed Gaussian-based profound learning method to depict the malignant growth injury in processed tomography pictures of the liver. They took a test of 225 pictures which are used to build up the proposed model. Yue et al. ( 2018 ) reviewed the machine learning techniques that include artificial neural networks, support vector machines, decision trees, and k-nearest neighbor for disease diagnosis. The author has investigated the breast cancer-related applications and applied them to the Wisconsin breast cancer database. Han et al. ( 2020 ) focused on the research and user-friendly design of an intelligent recommendation model for cancer patients’ rehabilitation schemes. Their prediction also achieved up to 92%. Rodrigues et al. ( 2020 ) proposed utilizing the move learning approach and profound learning approach in an IoT framework to help the specialists analyse common skin sores, average nevi, and melanoma. This investigation utilized two datasets: the first gave by the International Skin Imaging Collaboration at the worldwide Biomedical Imaging Symposium. The DenseNet201 extraction model, joined with the K nearest neighbor classifier, accomplished an exactness of 96.805% for the International Society for Bioluminescence and Chemiluminescence - International Standard Industrial Classification dataset. Huang et al. ( 2020 ) reviewed the literature on the application of artificial intelligence for cancer diagnosis and prognosis and demonstrated how these methods were advancing the field. Kather et al. ( 2019 ) used deep learning to mine clinically helpful information from histology. It can also predict the survival and molecular alternations in gastrointestinal and liver cancer. Also, these methods could be used as an inexpensive biomarker only if the pathology workflows are used. Kohlberger et al. ( 2019 ) built up a convolution neural organization to restrict and measure the seriousness of out-of-fold districts on digitized slides. On contrasting it and pathologist-reviewed center quality, ConvFocus accomplished Spearman rank coefficients of 0.81 and 0.94 on two scanners and replicated the typical designs from stack checking. Tschandl et al. ( 2019 ) build an image-based artificial intelligence for skin cancer diagnosis to address the effects of varied representations of clinical expertise and multiple clinical workflows. They also found that excellent quality artificial intelligence-based clinical decision-making support improved diagnostic accuracy over earlier artificial intelligence or physicians. It is observed that the least experienced clinicians gain the most from AI-based support. Chambi et al. ( 2019 ) worked on the volumetric Optical coherence tomography datasets acquired from resected cerebrum tissue example of 21 patients with glioma tumours of various stages. They were marked as either non-destructive or limo-invaded based on histopathology assessment of the tissue examples. Unlabelled Optical coherence tomography pictures from the other nine patients were utilized as the approval dataset to evaluate the strategy discovery execution. Chen et al. ( 2019a , b ) proposed a cost-effective technique, i.e., ARM (augmented reality microscope), that overlays artificial intelligence-based information onto the current view of the model in real-time, enabling a flawless combination of artificial intelligence into routine workflows. They even anticipated that the segmented reality microscope would remove the barrier to using AI considered to enhance the accuracy and efficiency of cancer analysis.
Diabetes detection
Diabetes Mellitus, also known as diabetes, is the leading cause of high blood sugar. AI is cost-effective to reduce the ophthalmic complications and preventable blindness associated with diabetes. This section covers the study of various researchers that worked on detecting diabetes in patients (Chaki et al. 2020 ). Kaur and Kumari ( 2018 ) used machine learning models on Pima Indian diabetes dataset to see patterns with risk factors with the help of the R data manipulation tool. They also analyse d five predictive models using the R data manipulation tool and support vector machine learning algorithm: linear kernel support vector machine, multifactor dimensionality reduction, and radial basis function.
As shown in Fig. 5 , blood glucose prediction has been categorized in three different parts: physiology-based, information-driven, and hybrid-based. Woldaregy et al. ( 2019 ) developed a compact guide in machine learning and a hybrid system that focused on predicting the blood glucose level in type 1 diabetes. They mentioned various machine learning methods crucial to regulating an artificial pancreas, decision support system, blood glucose alarm applications. They had also portrayed the knowledge about the blood glucose predictor that gave information to track and predict blood glucose levels as many factors could affect the blood glucose levels like BMI, stress, illness, medications, amount of sleep, etc. Thus blood glucose prediction provides the forecasting of an individual’s blood glucose level based on the past and current history of the patient to give an alarm to delay any complications. Chaki et al. ( 2020 ) provided detailed information to detect diabetes mellitus and self-management techniques to prove its importance to the scientists that work in this area. They also analyse d and diagnosed diabetes mellitus via its dataset, pre-processing techniques, feature extraction methods, machine learning algorithms, classification, etc. Mercaldo et al. ( 2017 ) proposed a method to classify diabetes-affected patients using a set of characteristics selected by a world health organization and obtained the precision value and recall value 0.770 and 0.775, respectively, with the help of the Hoeffding tree algorithm. Mujumdar et al. ( 2019 ) proposed the model for prediction, classification of diabetes, and external factors like glucose, body mass index, insulin, age, etc. They also analyse d that classification accuracy proved to be much more efficient with the new dataset than their used dataset. Kavakiotis et al. ( 2017 ) conducted a systematic review regarding the machine learning applications, data mining techniques, and tools used in the diabetes field to showcase the prediction and diagnosis of diabetes, its complications, and genetic conditions and situation, including the physical condition care management. After the in-depth search, it had been found that supervised learning methods characterized 85%, and the rest, 15%, were characterized by unsupervised learning methods. Aggarwal et al. ( 2020 ) demonstrated the non-linear heart rate variability in the prediction of diabetes using an artificial neural network and support vector machine. The author computed 526 datasets and obtained the classification accuracy of 90.5% with a support vector machine. Besides that, they evaluated thirteen non-linear heart rate variability parameters for the training and testing of artificial neural networks. Lukmanto et al. ( 2015 ) worked on many diabetes mellitus patients to provide an advantage for researchers to fight against it. Their main objective was to leverage fuzzy support vector machine and F-score feature selection to classify and detect diabetes mellitus. The methodology is applied to the Pima Indian Diabetes dataset, where they got an accuracy of 89.02% to predict the diabetes mellitus patients. Wang et al. ( 2017 ) proposed a weighted rank support vector machine to overcome the imbalanced problem seen during the daily dose system of drugs, leading to poor prediction results. They also employed the area under the curve (AUC) to show the model’s effectiveness and improved the average precision of their proposed algorithm. Carter et al. ( 2018 ) showcased the performance of 46 different machine learning models compared on re-sampled trained and tested data. The model obtained the area under the curve of 0.73 of training data and 0.90 of tested data. Nazir et al. ( 2019 ) proposed a technique to minutely detect the diabetic retinopathy’s different stages via tetragonal local octa pattern features that are further classified by extreme machine learning. For classifying periodic heart rate variability signals and diabetes, Swapna et al. ( 2018 ) presented a deep learning architecture. The authors used long short term memory, a convolution neural network, to extract the dynamic features of heart rate variability. They achieved an accuracy of 95.7% on using electrocardiography signals along with the support vector machine classification.

Blood glucose prediction approaches (Woldaregy et al. 2019 )
Diagnose chronic diseases
Researchers have shown that artificial intelligence helps in the streamlining care of chronic diseases. Therefore, various machine learning algorithms are developed to identify patients at higher risk of chronic disease. The other techniques based on AI are stated below (Jain et al. 2018 ).
Jain et al. ( 2018 ) presented a survey to showcase feature choice and arrangement methods to analyse and anticipate the constant illnesses. They utilized dimensionality decrease strategies to improve the presentation of AI calculation. To put it plainly, they introduced different component determination techniques and their inalienable points of interest and impediments. He et al. ( 2019 ) proposed a kernel-based structure for training the chronic illness detector to forecast and track the disease’s progression. Their approach was based on an enhanced version of a structured output support vector machine for longitudinal data processing. Tang et al. ( 2020 ) utilized deep residual networks to identify chronic obstructive pulmonary disease automatically. After gathering data from the PanCad project, which includes ex-smokers and current smokers at high risk of lung cancer, the residual network was trained to diagnose chronic obstructive pulmonary disease using computed topography scans. Additionally, they ran three rounds of cross-validation on it. With the help of three-fold cross-validation, the experiment had an area under the curve of 0.889. Ma et al. ( 2020 ) proposed the heterogeneous changed artificial neural organization to identify, divide, and determine persistent renal disappointment utilizing the web of medical things stage. The proposed strategy was named uphold vector machine and multilayer perceptron alongside the back engendering calculation. They used ultrasound images and later performed segmentation in that image. Especially in Kidney segmentation, it performed very well by achieving high results. Aldhyani et al. ( 2020 ) proposed the system that was used to increase the accuracy in detecting chronic disease by using machine learning algorithms. The machine learning methods such as Naïve Bayes, support vector machine, K nearest neighbour, and random forest were presented and compared. They also used a rough k-means algorithm to figure out the ambiguity in chronic disease to improve its performance. The Naïve Bayes method and RKM achieved an accuracy of 80.55% for diabetic disease, the support vector machine achieved 100% accuracy for kidney disease, and the support vector machine achieved 97.53% for cancer disease. Chui and Alhalabi ( 2017 ) reviewed the chronic disease diagnosis in smart health care. They provide a summarized view of optimization algorithms and machine learning algorithms. The authors also gave information regarding Alzheimer’s disease, dementia, tuberculosis, etc., followed by the challenges during the deployment phase of the disease diagnosis. Nam et al. ( 2019 ) introduced the internet of things and digital biomarkers and their relationships to artificial intelligence and other current trends. They have also discussed the role of artificial intelligence in the internet of things for chronic disease detection. Battineni et al. ( 2020 ) reviewed the applications of predictive models of machine learning to diagnose chronic disease. After going through 453 papers, they selected only 22 studies from where it was concluded that there were no standard methods that would determine the best approach in real-time clinical practice. The commonly used algorithms were support vector machine, logistic regression, etc. Wang et al. ( 2018 ) analyse d chronic kidney disease using machine learning techniques based on chronic kidney disease dataset and performed ten-fold cross-validation testing. The dataset had been pre-processed for completing and normalizing the missing data. They achieved the detection accuracy of 99% and were further tested using four patient data samples to predict the disease. Kim et al. ( 2019 ) indicated the constant sicknesses in singular patients that utilized a character repetitive neural organization to regard the information in each class as a word, mainly when an enormous bit of its information esteem is absent. They applied the Char-recurrent neural network to characterize the Korea National Health and Nutrition Examination Survey cases. They indicated the aftereffects of higher precision for the Char-recurrent neural network than for the customary multilayer perceptron model. Ani et al. ( 2017 ) proposed a patient monitoring system for stroke-affected people that reduced future recurrence by alarming the doctor and provided the data analytics and decision-making based on the patient’s real-time health parameters. That helped the doctors in systematic diagnosis followed by tailored treatment of the disease.
Heart disease diagnosis
Researchers suggest that artificial intelligence can predict the possible periods of death for heart disease patients. Thus multiple algorithms have been used to predict the heart rate severity along with its diagnosis. Escamila et al. ( 2019 ) proposed a dimensionality decrease strategy to discover the highlights of coronary illness utilizing the highlight determination procedure. The dataset used was the UCIrvine artificial intelligence vault called coronary illness which contains 74 highlights. The most remarkable precision was accomplished by the chi-square and head segment investigation alongside the irregular woods classifier. Tuli et al. ( 2019 ) proposed a Health fog framework to integrate deep learning in edge computing devices and incorporate it into the real-life application of heart detecting disease. They consisted of the hardware and software components, including body area sensor network, gateway, fogbus module, data filtering, pre-processing, resource manager, deep learning module, and ensembling module. The health fog model was an internet of things-based fog enabled model that can help effectively manage the data of heart patients and diagnose it to identify the heart rate severity.
George et al. ( 2018 ) aimed to describe the obstacles Indian nurses face in becoming active and valued members of the cardiovascular healthcare team as cardiovascular disease imposed substantial and increasing physical, psychological, societal, and financial burdens. As shown in Fig. 6 , there are numerous possible facts for health intelligent mediations to support helping cardiovascular health and decreasing hazard for cardiovascular disease. So the focus has started on the inhibition of cardiovascular disease and, more importantly, on the advancement of cardiovascular health. Several findings revealed that depression is connected with inferior cardiovascular health between adults without cardiovascular disease.

Cardiovascular health promotion and disease prevention (George et al. 2018 )
Haq et al. ( 2018 ) created a system based on machine learning to diagnose the cardiac disease guess using its dataset and worked on seven prominent feature learning-based algorithms. It was also observed that the machine learning-based decision support system assisted the doctors in diagnosing the heart patients effectively. Khan and Member ( 2020 ) proposed a framework to estimate the cardio disease using a customized deep convolution network for categorizing the fetched sensor information into the usual and unusual state. Their results demonstrated that if there would be the utmost amount of records, the multi-task cascaded convolution neural network achieved an accuracy of 98.2%. Ahmed ( 2017 ) explained the architecture for heart rate and other techniques to understand using machine learning algorithms such as K nearest neighbour classification to predict the heart attack during collecting heart rate datasets. The author also mentioned the six data types predicting heart attack in three different levels (Patel 2016 ). The dataset used consists of 303 instances and 76 attributes. They worked on a technique that could reduce the number of deaths from heart diseases. They compared various decision tree algorithms to present the heart disease diagnosis using Waikato Environment for Knowledge Analysis. They aimed to fetch the hidden patterns by using data mining techniques linked to heart disease to predict its presence. Saranya et al. ( 2019 ) proposed a cloud-based approach based on sensors for an automated disease predictive system to calculate various parameters of patients like blood pressure, heartbeat rate, and temperature. As per their knowledge, this method could reduce the time complexity of the doctor and patient in providing medical treatment quickly. The best part was that anyone could access it from anywhere. Isravel et al. ( 2020 ) presented a pre-processing approach that might enhance the accuracy in identifying the electrocardiographic signals. They evaluated the classification using different classifying algorithms such as K nearest neighbour, Naïve Bayes, and Decision tree to detect normal and irregular heartbeat sounds. Also, after trying, it was discovered that pre-processing approach increased the performance of classifying algorithms. The devices utilized for IoT set up were the LM35 sensor, Pulse sensor, AD8232 electrocardiographic sensor, and Arduino Uno. Thai et al. ( 2017 ) proposed a new lightweight method to remove the noise from electrocardiographic signals to perform minute diagnosis and prediction. Initially, they worked on the Sequential Recursive algorithm for the transformation of signals into digital format. The same was sent to the Discrete Wavelet Transform algorithm to detect the peaks in the data for removing the noises. Then features were extracted from the electrocardiographic dataset from Massachusetts Institute of Technology-Beth Israel Hospital to perform diagnosis and prediction and remove the redundant features using Fishers Linear Discriminant. Nashif et al. ( 2018 ) proposed a cloud-based heart disease prediction system for detecting heart disease using machine learning models derived from Java Based Open Access Data Mining Platform, Waikato Environment for Knowledge Analysis. They got an accuracy level of 97.53% using a support vector machine with 97.50% sensitivity and 94.94% specificity. They used an efficient software tool that trained the large dataset and compared multiple machine learning techniques. The smartphone used to detect and predict heart disease based on the information acquired from the patients. Hardware components are used to monitor the system continuously. Babu et al. ( 2019 ) aimed to determine whether the heart attack could occur using hereditary or not. Thus to work on it, initially, they collected and compared the previous data of parents with their child dataset to find the prediction and accurate values. It could help them to determine how healthy the child is. The authors used different parameters to show the dependent and independent parameters to find whether the person gets a heart attack.
Tuberculosis disease detection
AI is placed as an answer for aid in the battle against tuberculosis. Computerized reasoning applications in indicative radiology might have the option to give precise methods for recognizing the infections for low pay countries. Romero et al. ( 2020 ) performed the classification tree analysis to reveal the associations between predictors of tuberculosis in England. They worked on the American Public Health Association data ranging from demographic herd properties and tuberculosis variables using Sam Tuberculosis management. They used a machine-learning algorithm, performed data preparation, data reduction, and data analysis, and finally got the results. Horvath et al. ( 2020 ) performed the automatic scanning and analysis on 531 slides of tuberculosis, out of which 56 were from the positive specimen. They also validated a scanning and analysis system to combine fully automated microscopy using deep learning analysis. Their proposed system achieved the highest sensitivity by detecting 40 out of 56 positive slides. Sathitratanacheewin et al. ( 2020 ) developed a convolution neural network model using tuberculosis. They used a specified chest X-ray dataset taken from the national library of medical Shenzhen no. 3 hospitals and did its testing with a non-tuberculosis chest X-ray dataset taken from the national institute of health care and center. The deep convolution neural network model achieved the region of curve area under the curve by 0.9845 and 0.8502 for detecting tuberculosis and the specificity 82% and sensitivity of 72%. Bahadur et al. ( 2020 ) proposed an automatic technique to detect the abnormal chest X-ray images that contained at least one pathology such as infiltration, fibrosis, pleural effusion, etc., because of tuberculosis. This technique is based on a hierarchical structure for extracting the feature where feature sets are used in two hierarchy levels to group healthy and unhealthy people. The authors used 800 chest X-ray images taken from two public datasets named Montgomery and Shenzhen. López-Úbeda et al. ( 2020 ) explored the machine learning methods to detect tuberculosis in Spanish radiology reports. They also mentioned the deep learning classification algorithms with the purpose of its evaluation and comparison and to carry such a task. The authors have used the data of 5947 radiology reports collected from high-tech media. Ullah et al. ( 2020 ) presented the study of Raman Spectroscopy and machine learning based on principal component analysis and hierarchical component analysis to analyse tuberculosis either in positive form or negative form. They also showed Raman results which indicated the irregularities in the blood composition collected from tuberculosis-negative patients. Panicker et al. ( 2018 ) introduced the programmed technique for the location of tuberculosis bacilli from tiny smear pictures. They performed picture binarization and grouping of distinguished districts utilizing convolution neural organization. They did an assessment utilizing 22 sputum smear minuscule pictures. The results demonstrated 97.13% review, 78.4% accuracy, 86.76% F-score for predicting tuberculosis. Lai et al. ( 2020 ) compared the artificial neural network outcomes, support vector machine, and random forest while diagnosing anti-tuberculosis drugs on Taipei Medical University Wanfang Hospital patients. They selected the features via univariate risk factor analysis and literature evaluation. The authors achieved the specificity by 90.4% and sensitivity of 80%. Gao et al. ( 2019 ) investigated the applications of computed topography pulmonary images to detect tuberculosis at five levels of severity. They proposed a deep Res Net to predict the severity scores and analyse the high severity probability. They also calculate overall severity probability, separate probabilities of both high severity and low severity forces. Singh et al. ( 2020 ) worked to discover tuberculosis sores in the lungs. They proposed a computerized recognition strategy utilizing a profound learning technique known as Antialiased Convolution Neural Network proposed by Richard Zhang. Their dataset included 3D computed topography pictures, which were cut into 2D pictures. They applied division on each cutting picture utilizing UNet and Link net design.
Stroke and cerebrovascular disease detection
AI can analyse and detect stroke signs in medical images as if the system suspects a stroke in the patient. It immediately gives the signal to the patient or doctor. Researchers have proposed various methodologies to showcase the impact of AI in stroke and cerebrovascular detection (Singh et al. 2009 ). O’Connell et al. ( 2017 ) assessed the diagnostic capability and temporal stability for the detection of stroke. They observed the mostly identical patterns between the stroke patients and controls across the ten patients. They achieved the specificity and sensitivity of 90% across the research. Labovitz et al. ( 2017 ) stated the use of AI for daily monitoring of patients for the identification and medication. They achieved the improvement by 50%on plasma drug concentration levels. Abedi et al. ( 2020 ) also presented a framework to build up the decision support system using an artificial neural network, which improved patient care and outcome. Singh et al. ( 2009 ) compared the different methods to predict stroke on the cardiovascular health study dataset. They also used the decision tree algorithm for the feature selection process, principal component analysis to reduce the classification algorithm’s dimension, and a backpropagation neural network. Biswas et al. ( 2020 ) introduced an AI-based system for the location and estimation of carotid plaque as carotid intima-media thickness for the same and solid atherosclerotic carotid divider discovery and plaque estimations.
Hypertension disease detection
Researchers have found that AI has been able to diagnose hypertension by taking input data from blood pressure, demographics, etc. Krittanawong et al. ( 2018 ) summarized the review about the recent computer science and medical field advancements. They also illustrated the innovative approach of artificial intelligence to predict the early stages of hypertension. They also stated that AI plays a vital role in investigating the risk factors for hypertension. However, on the side, it has also been restricted by researchers because of its limitations in designing, etc. Arsalan et al. ( 2019 ) conducted the experiments using three publicly available datasets as digitized retinal imagery for vessel extraction (DRIVE), structured analysis of retina (STARE) for hypertension detection. They achieved the accuracy for all datasets with sensitivity, specificity, area under the curve, and accuracy of 80.22%, 98.1%, 98.2%, 96.55%, respectively. Kanegae et al. ( 2020 ) used machine learning techniques to validate the prediction of risk for new-onset hypertension. They used data in a split form for the model construction and development and validation to test its performance. The models they used were XGBoost and ensemble, in which the XGBoost model was considered the best predictor because it was systolic blood pressure nature during cardio ankle vascular. Figure 7 shows the structure of heart during its normal phase as well as in hypertension phase. When the human heart is in hypertension phase, its pulmonary arteries gets constricted because of which the right ventricle did not get the blood in to the lungs.

Pulmonary hypertension (Kanegae et al. 2020 )
Koshimizu et al. ( 2020 ) has also described artificial intelligence in pulse the executives, which was utilized to foresee the chance of circulatory strain utilizing enormous scope information. The authors also focused on the measure that was used to control blood pressure using an artificial neural network. In a nutshell, they were trying to prove that an artificial neural network is beneficial for high blood pressure organization and can also use it to create medical confirmation for the realistic organization of hypertension. Mueller et al. ( 2020 ) stated that using artificial analytic tools to the large dataset based on hypertension would generate questionable results and would also miss treatments and the potential targets. The author also stated that the vision of hypertension would be challenging to achieve and doubtlessly not happen in the future. Chaikijuraja et al. ( 2020 ) also noted the merits of using artificial intelligence to detect hypertension as artificial intelligence can recognize hypertension’s risk factors and phenotypes.
Moreover, it is used to interpret data from randomized trials that contained blood pressure targets associated with cardio vascular outcomes. Kiely et al. ( 2019 ) investigated the prescient model dependent on the medical care assets that could be sued to screen huge populaces to distinguish the patients at great danger of pneumonic blood vessel hypertension. They took the information of 709 patients from 2008 to 2016 with pneumonic blood vessel hypertension and contrasted it and separated associate of 2,812,458 who was delegated non-aspiratory blood vessel hypertension just as the prescient model was created and approved by utilizing cross approval. Kwon et al. ( 2020 ) did the past group learning of information taken on or after successive diseased people from two health care sectors to predict pulmonary hypertension using electrocardiography with the help of artificial intelligence. Sakr et al. ( 2018 ) assessed and analyse d AI strategies, such as Logit Boost, Bayesian Network Classifier, locally weighted Naïve Bayes, counterfeit neural organization, Support Vector Machine, and Random Tree Forest foresee the people to recognize hypertension. Thus, AI provides insights for hypertension healthcare and implements prescient, customized, and pre-emptive methodologies in clinical practice.
Skin disease diagnosis
Researchers have developed an AI system that can precisely group cutaneous skin problems and fill in as an auxiliary instrument to improve the demonstrative exactness of clinicians. Chakraborty et al. ( 2017 ) proposed a neural-based location technique for various skin disorders. They utilized two infected skin pictures named Basel Cell Carcinoma and Skin Angioma. Non-overwhelming arranging hereditary calculation is used to prepare the counterfeit neural organization, contrasted with the neural network particle swarm optimization classifier and neural network Caesarean Section classifier. Zaar et al. ( 2020 ) collected the clinical images of skin disease from the department of Dermatology at the Sahlgrenska University, where artificial intelligence algorithms had been used for the classification, thereby achieving the diagnosis accuracy by 56.4% for the top five suggested diseases. Kumar et al. ( 2019 ) used a dual-stage approach that combined computer vision and machine learning to evaluate and recognize skin diseases. During training and testing of the diseases, the method produced an accuracy of up to 95%. Kolkur et al. ( 2018 ) developed a system that identified skin disease based on input symptoms. They collected the data of the symptoms of ten skin diseases and got 90% above accuracy.
Liver disease detection
Researchers have found that AI can treat liver disease at its early diagnosis to work on its endurance and heal rate. Abdar et al. ( 2018 ) showed that efficient early liver disease recognition through Multilayer Perceptron Neural Network calculation depends on different choice tree calculations, such as chi-square programmed communication indicator and characterization, and relapse tree with boosting strategy. Their technique had the option to analyse and characterize the liver malady proficiently. Khaled et al. ( 2018 ) introduced an artificial neural network for the diagnosis of hepatitis virus. Protein and Histology is utilized as an info variable for the fake neural organization model, and it also showed the correct prediction of diagnosis by 93%. Spann et al. ( 2020 ) provided the strengths of machine learning tools and their potential as machine learning is applied to liver disease research, including clinical, molecular, demographic, pathological, and radiological data. Nahar and Ara ( 2018 ) explored the early guess of liver ailment using various decision tree techniques. The choice tree methods utilized were J48, Licensed Massage Therapist, Random Forest, Random Tree, REP tree, Decision Stump, and Hoeffding Trees. Their primary purpose was to calculate and compare the performances of various decision tree techniques. Farokhzad et al. ( 2016 ) used fuzzy logic for diagnosing liver sickness. Using this method, where they had two triangular membership and Gussy membership functions, they reached 79–83% accuracy.
Comparative analysis
In addition to the above mentioned reported work, the comparative analysis illustrated in Table 4 showcase the detailed information such as type of dataset, techniques, and the predicted outcomes regarding the work done by the researchers on different diseases, which in return helped the author to look for the best technique for detecting or diagnosing any particular disease.
Comparative analysis for different disease detection
From Table 4 , we can observe that AI techniques have proven to be the best for detecting diseases with improved results. AI uses machine and deep learning models that work upon training and testing data sets so that the system can see the disease and diagnose it early. In the AI-based model, we initially need to train human beings to remember the data and provide accurate results. However, it also deals with the problem. Suppose the training data produced the incorrect analysis of disease because of insufficient information, which artificial intelligence cannot factor. As a result, it will become a horrible condition for the patients as AI cannot assure us whether the prediction regarding disease detection is accurate.
On assaying the accuracy of algorithms in diagnosing the disease, deep learning classifiers have dominated over machine learning models in the field of disease diagnosis. Deep learning models have proved to be best in terms of scalp disease by 99%, Alzheimer disease by 96%, thyroid disease by 99%, 96% in skin disease, 99.37% in case of Arrhythmia disease, 95.7% in diabetic disease, while as machine learning models achieved 89% in diabetic disease, 88.67% in tuberculosis, 86.84% in Alzheimer disease, etc.
We have presented recently published research studies that employed AI-based Learning techniques for diagnosing the disease in the current review. This study highlights research on disease diagnosis prediction and predicting the post-operative life expectancy of diseased patients using AI-based learning techniques.
Investigation 1 : Why do we need AI?
We know that AI is the simulation of human processes by machines (computer systems) and that this simulation includes learning, reasoning, and self-correction. We require AI since the amount of labour we must perform is rising daily. As a result, it’s a good idea to automate regular tasks. It conserves the organization’s staff and also boosts production (Vasal et al. 2020 ).
In terms of the healthcare industry, AI in health refers to a set of diverse technologies that enable robots to detect, comprehend, act, and learn1 to execute administrative and clinical healthcare activities. AI has the potential to transform healthcare by addressing some of the industry’s most pressing issues. For example, AI can result in improved patient outcomes and increased productivity and efficiency in care delivery (Gouda et al. 2020 ). It can also enhance healthcare practitioners’ daily lives by spending more time caring for patients, therefore increasing staff morale and retention. In addition, it may potentially help bring life-saving medicines to market more quickly. Figure 8 shows the significance of AI in the medical field.

Importance of artificial intelligence in healthcare
Investigation 2 : Why is AI important, and how is it used to analyse the disease?
The emergence of new diseases remains a critical parameter in human health and society. Hence, the advances in AI allow for rapid processing and analysis of such massive and complex data. It recommends the correct decision for over ten different diseases (as mentioned in the literature) with at least 98% accuracy.
Doctors use technologies such as computed tomography scan or magnetic resonance imaging to produce a detailed 3D map of the area that needs to be diagnosed. Later, AI technology analyse s the system-generated image using machine and deep learning models to spot the diseased area’s features in seconds. As shown in the framework section, an artificial intelligence model using machine and deep learning algorithms is initially trained with the help of a particular disease dataset (Owasis et al. 2019 ). The dataset is then pre-processed using data cleaning and transformation techniques so that the disease symptoms in the form of feature vectors can be extracted and further diagnosed.
Suppose doctors do not use AI techniques. In that case, it will cause a delay in treating the patients as it is tough to interpret the scanned image manually, and it also takes a considerable amount of time. But, on the other hand, it shows that an AI technique helps the patients and helps the doctors save the patient’s life by treating them as early as possible (Luo et al. 2019 ).
Investigation 3 : What is the impact of AI in medical diagnosis?
Due to advancements in computer power, learning algorithms, and the availability of massive datasets (big data) derived from medical records and wearable health monitors. The best part of implementing AI in healthcare is that it helps to enhance various areas, including illness detection, disease classification, decision-making processes, giving optimal treatment choices, and ultimately, helping people live longer. In terms of disease diagnosis, AI has been used to enhance medical diagnosis (Chen et al. 2019a , b ). For example, the technology, which is currently in use in China, may detect hazardous tumors and nodules in patients with lung cancer, allowing physicians to provide an early diagnosis rather than sending tissue samples to a lab for testing, allowing for earlier treatment (Keenan et al. 2020 ). Figure 9 illustrates the influence of artificial intelligence and other approaches.

Comparison between AI and other techniques
Investigation 4 : Which AI-based algorithm is used in disease diagnosis?
Disease detection algorithms driven by AI demonstrated to be an effective tool for identifying undiagnosed patients with under-diagnosed, uncoded, and rare diseases. Therefore, AI models for disease detection have an ample opportunity to drive earlier diagnosis for patients in need and guide pharmaceutical companies with highly advanced, targeted diagnostics to help these patients get correctly diagnosed and treated earlier in their disease journey (Keenan et al. 2020 ). The research work mentioned in the literature has covered both machine and deep learning models for diagnosing the diseases such as cancer, diabetes, chronic, heart disease, alzheimer, stroke and cerebrovascular, hypertension, skin, and liver disease. Machine learning models, Random Forest Classifier, Logistic Regression, Fuzzy logics, Gradient Boosting Machines, Decision Tree, K nearest neighbour (KNN), and Support vector machines (SVM) are primarily used in literature. Among deep learning models, Convolutional Neural Networks (CNN) have been used most commonly for disease diagnosis. In addition, faster Recurrent Convolution Neural Network, Multilayer Perceptron, Long Short Term Memory (LSTM) have also been used extensively in the literature. Figure 10 displays the usage of AI-based prediction models in the literature.

Artificial intelligence-based prediction models
Investigation 5 : What are the challenges faced by the researchers while using AI models in several disease diagnosis?
Although AI-based techniques have marked their significance in disease diagnosis, there are still many challenges faced by the researchers that need to be addressed.
- i. Limited Data size The most common challenge faced by most of the studies was insufficient data to train the model. A small sample size implies a smaller training set which does not authenticate the efficiency of the proposed approaches. On the other hand, good sample size can train the model better than the limited one (Rajalakshmi et al. 2018 ).
- ii. High dimensionality Another data-related issue faced in cancer research is high dimensionality. High dimensionality is referred to a vast number of features as compared to cases. However, multiple dimensionality reduction techniques are available to deal with this issue (Bibault et al. 2020 ).
- iii. Efficient feature selection technique Many studies have achieved exceptional prediction outcomes. However, a computationally effective feature selection method is required to eradicate the data cleaning procedures while generating high disease prediction accuracy (Koshimizu et al. 2020 ).
- iv. Model Generalizability A shift in research towards improving the generalizability of the model is required. Most of the studies have proposed a prediction model that is validated on a single site. There is a need to validate the models on multiple sites that can help improve the model’s generalizability (Fukuda et al. 2019 ).
- v. Clinical Implementation AI-based models have proved their dominance in medical research; still, the practical implementation of the models in the clinics is not incorporated. These models need to be validated in a clinical setting to assist the medical practitioner in affirming the diagnosis verdicts (Huang et al. 2020 ).
Investigation 6 : How artificial intelligence-based techniques are helping doctors in diagnosing diseases?
AI improves the lives of patients, physicians, and hospital managers by doing activities usually performed by people but in a fraction of the time and the expense. For example, AI assists physicians in making suggestions by evaluating vast amounts of healthcare data such as electronic health records, symptom data, and physician reports to improve health outcomes and eventually save the patient’s life (Kohlberger et al. 2019 ). Additionally, this data aids in the improvement and acceleration of decision-making while diagnosing and treating patients’ illnesses using artificial intelligence-based approaches. Not only that, AI assists physicians in detecting diseases by utilizing complicated algorithms, hundreds of biomarkers, imaging findings from millions of patients, aggregated published clinical studies, and thousands of physicians’ notes to improve the accuracy of diagnosis.
Conclusion and future scope
When it comes to disease diagnosis, accuracy is critical for planning, effective treatment and ensuring the well-being of patients. AI is a vast and diverse realm of data, algorithms, analytics, deep learning, neural networks, and insights that is constantly expanding and adapting to the needs of the healthcare industry and its patients. According to the findings of this study, AI approaches in the healthcare system, particularly for illness detection, are essential. Aiming at illuminating how machine and deep learning techniques work in various disease diagnosis areas, the current study has been divided into several sections that cover the diagnosis of alzheimer’s, cancer, diabetes, chronic diseases, heart disease, stroke and cerebrovascular disease, hypertension, skin disease, and liver disease. The introduction and contribution were covered in the first section, followed by an evaluation of the quality of the work and an examination of AI approaches and applications. Later, various illness symptoms and diagnostic difficulties, a paradigm for AI in disease detection models, and various AI applications in healthcare were discussed. The reported work on multiple diseases and the comparative analysis of different techniques with the used dataset as well as the results of an applied machine and deep learning methods in terms of multiple parameters such as accuracy, sensitivity, specificity, an area under the curve, and F-score has also been portrayed. Finally, the work that assisted researchers in determining the most effective method for detecting illnesses is finished, as in future scope. In a nutshell, medical experts better understand how AI may be used for illness diagnosis, leading to more appropriate proposals for the future development of AI based techniques.
Contrary to considerable advancements over the past several years, the area of accurate clinical diagnostics faces numerous obstacles that must be resolved and improved constantly to treat emerging illnesses and diseases effectively. Even healthcare professionals recognize the barriers that must be overcome before sickness may be detected in conjunction with artificial intelligence. Even doctors do not entirely rely on AI-based approaches at this time since they are unclear of their ability to anticipate illnesses and associated symptoms. Thus much work is required to train the AI-based systems so that there will be an increase in the accuracy to predict the methods for diagnosing diseases. Hence, in the future, AI-based research should be conducted by keeping the flaw mentioned earlier in consideration to provide a mutually beneficial relationship between AI and clinicians. In addition to this, a decentralized federated learning model should also be applied to create a single training model for disease datasets at remote places for the early diagnosis of diseases.
Acknowledgements
This research work was supported by Sejong University research fund. Yogesh Kumar and Muhammad Fazal Ijaz contributed equally to this work and are first co-authors.
Declarations
The authors declare that they have no conflict of interest.
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
This article does not contain any studies with the animals performed by any of the authors.
Informed consent was obtained from all individual participants included in the study.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Yogesh Kumar, Email: [email protected] .
Apeksha Koul, Email: moc.liamg@9oluokahskepa .
Ruchi Singla, Email: moc.oohay@algnisihcur .
Muhammad Fazal Ijaz, Email: rk.ca.gnojes@lazaf .
- Abdar M, Yen N, Hung J. Improving the diagnosis of liver disease using multilayer perceptron neural network and boosted decision tree. J Med Biol Eng. 2018; 38 :953–965. doi: 10.1007/s40846-017-0360-z. [ CrossRef ] [ Google Scholar ]
- Abedi V, Khan A, Chaudhary D, Misra D, Avula V, Mathrawala D, Kraus C, Marshall KA, Chaudhary N, Li X, Schirmer CM, Scalzo F, Li J, Zand R. Using artificial intelligence for improving stroke diagnosis in emergency departments: a practical framework. Ther Adv Neurol Disord. 2020 doi: 10.1177/1756286420938962. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Aggarwal Y, Das J, Mazumder PM, Kumar R, Sinha RK. Heart rate variability features from nonlinear cardiac dynamics in identification of diabetes using artificial neural network and support vector machine. Integr Med Res. 2020 doi: 10.1016/j.bbe.2020.05.001. [ CrossRef ] [ Google Scholar ]
- Ahmed F. An Internet of Things (IoT) application for predicting the quantity of future heart attack patients. J Comput Appl. 2017; 164 :36–40. doi: 10.5120/ijca2017913773. [ CrossRef ] [ Google Scholar ]
- Aldhyani THH, Alshebami AS, Alzahrani MY. Soft clustering for enhancing the diagnosis of chronic diseases over machine learning algorithms. J Healthc Eng. 2020 doi: 10.1155/2020/4984967. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Alfian G, Syafrudin M, Ijaz MF, Syaekhoni MA, Fitriyani NL, Rhee J. A personalized healthcare monitoring system for diabetic patients by utilizing BLE-based sensors and real-time data processing. Sensors. 2018; 18 (7):2183. doi: 10.3390/s18072183. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Ali M, Tengnah J, Sooklall R. A predictive model for hypertension diagnosis using machine learning techniques. Telemed Technol. 2019 doi: 10.1016/B978-0-12-816948-3.00009-X. [ CrossRef ] [ Google Scholar ]
- Ani R, Krishna S, Anju N, Aslam MS, Deepa OS (2017) IoT based patient monitoring and diagnostic prediction tool using ensemble classifier. In: 2017 International conference on advances in computing, communications and informatics (ICACCI), pp 1588–1593. 10.1109/ICACCI.2017.8126068
- Ansari S, Shafi I, Ansari A, Ahmad J, Shah S. Diagnosis of liver disease induced by hepatitis virus using artificial neural network. IEEE Int Multitopic. 2011 doi: 10.1109/INMIC.2011.6151515. [ CrossRef ] [ Google Scholar ]
- Arsalan M, Owasis M, Mahmood T, Cho S, Park K. Aiding the diagnosis of diabetic and hypertensive retinopathy using artificial intelligence based semantic segmentation. J Clin Med. 2019; 8 :1446. doi: 10.3390/jcm8091446. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Babu BS, Likhitha V, Narendra I, Harika G. Prediction and detection of heart attack using machine learning and internet of things. J Comput Sci. 2019; 4 :105–108. [ Google Scholar ]
- Bahadur T, Verma K, Kumar B, Jain D, Singh S. Automatic detection of Alzheimer related abnormalities in chest X-ray images using hierarchical feature extraction scheme. Expert Syst Appl. 2020; 158 :113514. doi: 10.1016/j.eswa.2020.113514. [ CrossRef ] [ Google Scholar ]
- Balaji E, Brindha D, Balakrishnan R. Supervised machine learning based gait classification system for early detection and stage classification of Parkinson’s disease. Appl Soft Comput J. 2020; 94 :106494. doi: 10.1016/j.asoc.2020.106494. [ CrossRef ] [ Google Scholar ]
- Battineni G, Sagaro GG, Chinatalapudi N, Amenta F. Applications of machine learning predictive models in the chronic disease diagnosis. J Personal Med. 2020 doi: 10.3390/jpm10020021. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Behera R, Bala P, Dhir A. The emerging role of cognitive computing in healthcare: a systematic literature review. J Med Inform. 2019; 129 :154–166. doi: 10.1016/j.ijmedinf.2019.04.024. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Bhatt V, Pal V (2019) An intelligent system for diagnosing thyroid disease in pregnant ladies through artificial neural network. In: Conference on advances in engineering science management and technology, pp 1–10. 10.2139/ssrn.3382654
- Bibault J, Xing L. Screening for chronic obstructive pulmonary disease with artificial intelligence. Lancet Digit Health. 2020; 2 :e216–e217. doi: 10.1016/S2589-7500(20)30076-5. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Biswas M, Saba L, Suri H, Lard J, Suri S, Miner M, et al. Two stage artificial intelligence model for jointly measurement of atherosclerotic wall thickness and plaque burden in carotid ultrasound. Comput Biol Med. 2020; 123 :103847. doi: 10.1016/j.compbiomed.2020.103847. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Carter JA, Long CS, Smith BP, Smith TL, Donati GL. PT US CR. Expert Syst Appl. 2018 doi: 10.1016/j.eswa.2018.08.002. [ CrossRef ] [ Google Scholar ]
- Chaikijurajai T, Laffin L, Tang W. Artificial intelligence and hypertension: recent advances and future outlook. Am J Hypertens. 2020; 33 :967–974. doi: 10.1093/ajh/hpaa102. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Chaki J, Ganesh ST, Cidham SK, Theertan SA. Machine learning and artificial intelligence based diabetes mellitus detection and self-management: a systematic review. J King Saud Univ Comput Inf Sci. 2020 doi: 10.1016/j.jksuci.2020.06.013. [ CrossRef ] [ Google Scholar ]
- Chakraborty S, Mali K, Chatterjee S, Banerjee S, Roy K et al (2017) Detetction of skin disease using metaheurisrtic supported artificial neural networks. In: Industrial automation and electromechanical engineering conference, pp 224–229. 10.1109/IEMECON.2017.8079594
- Chambi R, Kut C, Jimenez J, Jo J. AI assisted in situ detection of human glioma infiltration using a novel computational method for optical coherence tomography. Clin Cancer Res. 2019; 25 :6329–6338. doi: 10.1158/1078-0432.CCR-19-0854. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Chang W, Chen L, Wang W. Development and experimental evaluation of machine learning techniques for an intelligent hairy scalp detection system. Appl Sci. 2018; 8 :853. doi: 10.3390/app8060853. [ CrossRef ] [ Google Scholar ]
- Chatterjee A, Parikh N, Diaz I, Merkler A. Modeling the impact of inter hospital transfer network design on stroke outcomes in a large city. Stroke. 2018; 49 :370–376. doi: 10.1161/STROKEAHA.117.018166. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Chen Y, Sha M, Zhao X, Ma J, Ni H, Gao W, Ming D. Automated detection of pathologic white matter alterations in Alzheimer’s disease using combined diffusivity and kurtosis method. Psychiatry Res Neuroimaging. 2017; 264 :35–45. doi: 10.1016/j.pscychresns.2017.04.004. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Chen J, Remulla D, Nguyen J, Aastha D, Liu Y, Dasgupta P. Current status of artificial intelligence applications in urology and their potential to influence clinical practice. BJU Int. 2019; 124 :567–577. doi: 10.1111/bju.14852. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Chen P, Gadepalli K, MacDonald R, Liu Y, Dean J. An augmented reality microscope with real time artificial intelligence integration for cancer diagnosis. Nat Med. 2019; 25 :1453–1457. doi: 10.1038/s41591-019-0539-7. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Chuang C. Case based reasoning support for liver disease diagnosis. Artif Intell. 2011; 53 :15–23. doi: 10.1016/j.artmed.2011.06.002. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Chui KT, Alhalabi W. Disease diagnosis in smart healthcare: innovation. Technol Appl. 2017 doi: 10.3390/su9122309. [ CrossRef ] [ Google Scholar ]
- Chui CS, Lee NP, Adeoye J, Thomson P, Choi S-W. Machine learning and treatment outcome prediction for oral cancer. J Oral Pathol Med. 2020; 49 :977–985. doi: 10.1111/jop.13089. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Connell GCO, Chantler PD, Barr TL. Stroke-associated pattern of gene expression previously identified by machine-learning is diagnostically robust in an independent patient population. Genomics Data. 2017; 14 :47–52. doi: 10.1016/j.gdata.2017.08.006. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Dabowsa N, Amaitik N, Maatuk A, Shadi A (2017) A hybrid intelligent system for skin disease diagnosis. In: Conference on engineering and technology, pp 1–6. 10.1109/ICEngTechnol.2017.8308157
- Damiani G, Grossi E, Berti E, Conic R, Radhakrishna U, Linder D, Bragazzi N, Pacifico A, Piccino R. Artificial neural network allow response prediction in squamous cell carcinoma of the scalp treated with radio therapy. J Eur Acad Dermatol Venerel. 2020; 34 :1369–1373. doi: 10.1111/jdv.16210. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Das A, Acharya UR, Panda SS, Sabut S. Deep learning based liver cancer detection using watershed transform and Gaussian mixture model techniques. Cogn Syst Res. 2019; 54 :165–175. doi: 10.1016/j.cogsys.2018.12.009. [ CrossRef ] [ Google Scholar ]
- Escamilla G, Hassani A, Andres E. A comparison of machine learning techniques to predict the risk of heart failure. Mach Learn Paradig. 2019; 1 :9–26. doi: 10.1007/978-3-030-15628-2_2. [ CrossRef ] [ Google Scholar ]
- Farokhzad M, Ebrahimi L. A novel adapter neuro fuzzy inference system for the diagnosis of liver disease. J Acad Res Comput Eng. 2016; 1 :61–66. [ Google Scholar ]
- Fujita S, Hagiwara A, Otuska Y, Hori M, Kumamaru K, Andica C, et al. Deep learning approach for generating MRA images from 3D qunatitative synthetic MRI without additional scans. Invest Radiol. 2020; 55 :249–256. doi: 10.1097/RLI.0000000000000628. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Fukuda M, Inamoto K, Shibata N, Ariji Y, Kutsana S. Evaluation of an artificial system for detecting vertical root fracture on panoramic radiography. Oral Radiol. 2019; 36 :1–7. [ PubMed ] [ Google Scholar ]
- Gao XW, James-Reynolds C, Currie E. Analysis of Alzheimer severity levels from CT pulmonary images based on enhanced residual deep learning architecture. Healthc Technol. 2019 doi: 10.1016/j.neucom.2018.12.086. [ CrossRef ] [ Google Scholar ]
- George A, Badagabettu S, Berra K, George L, Kamath V, Thimmappa L. Prevention of cardiovascular disease in India. Clin Prev Cardiol. 2018; 7 :72–77. doi: 10.4013/JCPC.JCPC_31_17. [ CrossRef ] [ Google Scholar ]
- Gonsalves AH, Singh G, Thabtah F, Mohammad R. Prediction of coronary heart disease using machine learning: an experimental analysis. ACM Digit Libr. 2019 doi: 10.1145/3342999.3343015. [ CrossRef ] [ Google Scholar ]
- Gouda W, Yasin R. COVID-19 disease: CT pneumonia analysis prototype by using artificial intelligence, predicting the disease severity. J Radiol Nucl Med. 2020; 51 :196. doi: 10.1186/s43055-020-00309-9. [ CrossRef ] [ Google Scholar ]
- Gupta N, Verma R, Belho E. Bone scan and SPEC/CT scan in SAPHO syndrome. J Soc Nucl Med. 2019; 34 :349. doi: 10.4103/ijnm.IJNM_139_19. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Han Y, Han Z, Wu J, Yu Y, Gao S, Hua D, Yang A. Artificial intelligence recommendation system of cancer rehabilitation scheme based on IoT technology. IEEE Access. 2020; 8 :44924–44935. doi: 10.1109/ACCESS.2020.2978078. [ CrossRef ] [ Google Scholar ]
- Haq AU, Li JP, Memon MH, Nazir S, Sun R. A hybrid intelligent system framework for the prediction of heart disease using machine learning algorithms. Mob Inf Syst. 2018; 8 :1–21. doi: 10.1155/2018/3860146. [ CrossRef ] [ Google Scholar ]
- He K, Huang S, Qian X. Early detection and risk assessment for chronic disease with irregular longitudinal data analysis. J Biomed Inform. 2019; 96 :103231. doi: 10.1016/j.jbi.2019.103231. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Horvath L, Burchkhardt I, Mannsperger S, Last K, et al. Machine assisted interperation of auramine stains substantially increases through put and senstivity of micrscopic Alzheimer diagnosis. Alzheimer. 2020; 125 :101993. doi: 10.1016/j.tube.2020.101993. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Hosseinzadeh M, Ahmed O, Ghafour M, Safara F, Ali S, Vo B, Chiang H. A multiple multi layer perceptron neural network with an adaptive learning algorithm for thyroid disease diagnosis in the internet of medical things. J Supercomput. 2020 doi: 10.1007/s11227-020-03404-w. [ CrossRef ] [ Google Scholar ]
- Huang S, Yang J, Fong S, Zhao F. Artificial intelligence in cancer diagnosis and prognosis. Cancer Lett. 2020; 471 :61–71. doi: 10.1016/j.canlet.2019.12.007. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Ijaz MF, Alfian G, Syafrudin M, Rhee J. Hybrid prediction model for type 2 diabetes and hypertension using DBSCAN-based outlier detection, synthetic minority over sampling technique (SMOTE), and random forest. Appl Sci. 2018; 8 (8):1325. doi: 10.3390/app8081325. [ CrossRef ] [ Google Scholar ]
- Ijaz MF, Attique M, Son Y. Data-driven cervical cancer prediction model with outlier detection and over-sampling methods. Sensors. 2020; 20 (10):2809. doi: 10.3390/s20102809. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Isravel DP, Silas SVPD. Improved heart disease diagnostic IoT model using machine learning techniques. Neuroscience. 2020; 9 :4442–4446. [ Google Scholar ]
- Jain D, Singh V. Feature selection and classification systems for chronic disease prediction: a review. Egypt Inform J. 2018; 19 :179–189. doi: 10.1016/j.eij.2018.03.002. [ CrossRef ] [ Google Scholar ]
- Janghel RR, Rathore YK. Deep convolution neural network based system for early diagnosis of Alzheimer’s disease. Irbm. 2020; 1 :1–10. doi: 10.1016/j.irbm.2020.06.006. [ CrossRef ] [ Google Scholar ]
- Jo T, Nho K, Saykin AJ. Deep learning in Alzheimer’s disease: diagnostic classification and prognostic prediction using neuroimaging data. Front Aging Neurosci. 2019 doi: 10.3389/fnagi.2019.00220. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Kanegae H, Suzuki K, Fukatani K, Ito T, Kairo K, Beng N. Highly precise risk prediction model for new onset hypertension using artificial neural network techniques. J Clin Hypertens. 2020; 22 :445–450. doi: 10.1111/jch.13759. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Kasasbeh A, Christensen S, Parsons M, Lansberg M, Albers G, Campbell B. Artificial neural network computed tomography perfusion prediction of ischemic core. Stroke. 2019; 50 :1578–1581. doi: 10.1161/STROKEAHA.118.022649. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Katharine E, Oikonomou E, Williams M, Desai M. A novel machine learning derived radiotranscriptomic signature of perivascular fat improves cardiac risk prediction using coronary CT angiography. Eur Heart J. 2019; 40 :3529–3543. doi: 10.1093/eurheartj/ehz592. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Kather J, Pearson A, Halama N, Krause J, Boor P. Deep learning microsatellite instability directly from histology in gastrointestinal cancer. Nat Med. 2019; 25 :1054–1056. doi: 10.1038/s41591-019-0462-y. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Kaur H, Kumari V. Predictive modelling and analytics for diabetes using a machine learning approach. Appl Comput Inform. 2018 doi: 10.1016/j.aci.2018.12.004. [ CrossRef ] [ Google Scholar ]
- Kavakiotis I, Tsave O, Salifoglou A, Maglaveras N, Vlahavas I, Chouvarda I. Machine learning and data mining methods in diabetes research. Comput Struct Biotechnol. 2017; J15 :104–116. doi: 10.1016/j.csbj.2016.12.005. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Keenan T, Clemons T, Domalpally A, Elman M, Havilio M, Agron E, Chew E, Benyamini G. Intelligence detection versus artificial intelligence detection of retinal fluid from OCT: age-related eye disease study 2: 10 year follow on study. Ophthalmology. 2020 doi: 10.1016/j.ophtha.2020.06.038. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Khaled E, Naseer S, Metwally N. Diagnosis of hepatititus virus using arificial neural network. J Acad Pedagog Res. 2018; 2 :1–7. [ Google Scholar ]
- Khan MA, Member S. An IoT framework for heart disease prediction based on MDCNN classifier. IEEE Access. 2020; 8 :34717–34727. doi: 10.1109/ACCESS.2020.2974687. [ CrossRef ] [ Google Scholar ]
- Khan A, Zubair S. An improved multi-modal based machine learning approach for the prognosis of Alzheimer’s disease. J King Saud Univ Comput Inf Sci. 2020 doi: 10.1016/j.jksuci.2020.04.004. [ CrossRef ] [ Google Scholar ]
- Khan A, Khan M, Ahmed F, Mittal M, Goyal L, Hemanth D, Satapathy S. Gastrointestinal diseases segmentation and classification based on duo-deep architectures. Pattern Recognit Lett. 2020; 131 :193–204. doi: 10.1016/j.patrec.2019.12.024. [ CrossRef ] [ Google Scholar ]
- Kiely DG, Doyle O, Drage E, Jenner H, Salvatelli V, Daniels FA, Rigg J, Schmitt C, Samyshkin Y, Lawrie A, Bergemann R. Utilising artificial intelligence to determine patients at risk of a rare disease: idiopathic pulmonary arterial hypertension. Pulm Circ. 2019; 9 :1–9. doi: 10.1177/2045894019890549. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Kim C, Son Y, Youm S. Chronic disease prediction using character-recurrent neural network in the presence of missing information. Appl Sci. 2019; 9 :2170. doi: 10.3390/app9102170. [ CrossRef ] [ Google Scholar ]
- Kohlberger T, Norouzi M, Smith J, Peng L, Hipp J. Artificial intelligence based breast cancer nodal metastasis detection. Arch Pathol Lab Med. 2019; 143 :859–868. doi: 10.5858/arpa.2018-0147-OA. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Kolkur MS, Kalbande DR, Kharkar V. Machine learning approaches to multi-class human skin disease Ddetection. Innov Healthc Tech. 2018; 14 :29–39. [ Google Scholar ]
- Koshimizu H, Kojima H, Okuno Y. Future possibilities for artificial intelligence in the practical management of hypertension. Hypertens Res. 2020; 43 :1327–1337. doi: 10.1038/s41440-020-0498-x. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Krittanawong C, Bomback A, Baber U, Bangalore S, Tang M, Messerli F. Future direction for using artificial intelligence to predict and manage hypertension. Curr Hypertens Rep. 2018; 20 :75. doi: 10.1007/s11906-018-0875-x. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Kumar Y. Computational intelligence for machine learning and healthcare informatics. De Gruyter; 2020. Recent advancement of machine learning and deep learning in the field of healthcare system; pp. 7–98. [ Google Scholar ]
- Kumar Y, Singla R. Federated learning systems for healthcare: perspective and recent progress. In: Rehman MH, Gaber MM, editors. Studies in computational intelligence, vol965. Cham: Springer; 2021. [ Google Scholar ]
- Kumar A, Pal S, Kumar S. Classification of skin disease using ensemble data mining techniques. Asia Pac J Cancer Prev. 2019; 20 :1887–1894. doi: 10.31557/APJCP.2019.20.6.1887. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Kumar Y, Sood K, Kaul S, Vasuja R. Big data analytics in healthcare. Cham: Springer; 2020. pp. 3–21. [ Google Scholar ]
- Kwon J, Jeon H, Kim H, Lim S, Choi R. Comapring the performance of artificial intelligence and conventional diagnosis criteria for detetcting left ventricular hypertrophy using electropcardiography. EP Europace. 2020; 22 :412–419. doi: 10.1093/europace/euz324. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Labovitz D, Shafner L, Gil M, Hanina A, Virmani D. Using artificial intelligence reduce the risk of non adherence in patients on anticoagulation theraphy. Stroke. 2017; 48 :1416–1419. doi: 10.1161/STROKEAHA.116.016281. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Lai N, Shen W, Lee C, Chang J, Hsu M, et al. Comparison of the predictive outcomes for anti-Alzheimer drug-induced hepatotoxicity by different machine learning techniques. Comput Methods Programs Biomed. 2020; 188 :105307. doi: 10.1016/j.cmpb.2019.105307. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Lei B, Yang M, Yang P, Zhou F, Hou W, Zou W, Li X, Wang T, Xiao X, Wang S. Deep and joint learning of longitudinal data for Alzheimer’s disease prediction. Pattern Recognit. 2020; 102 :107247. doi: 10.1016/j.patcog.2020.107247. [ CrossRef ] [ Google Scholar ]
- Lin L, Shenghui Z, Aiguo W, Chen H. A new machine learning method for Alzheimer’s disease. Simul Model Pract Theory. 2019 doi: 10.1016/j.simpat.2019.102023. [ CrossRef ] [ Google Scholar ]
- Ljubic B, Roychoudhury S, Cao XH, Pavlovski M, Obradovic S, Nair R, Glass L, Obradovic Z. Influence of medical domain knowledge on deep learning for Alzheimer’s disease prediction. Comput Methods Programs Biomed. 2020 doi: 10.1016/j.cmpb.2020.105765. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Lodha P, Talele A, Degaonkar K (2018) Diagnosis of Alzheimer’s disease using machine learning. In: Proceedings—2018 4th international conference on computing, communication control and automation, ICCUBEA, pp 1–4
- López-Úbeda P, Díaz-Galiano MC, Martín-Noguerol T, Ureña-López A, Martín-Valdivia M-T, Lunab A. Detection of unexpected findings in radiology reports: a comparative study of machine learning approaches. Expert Syst Appl. 2020 doi: 10.1016/j.eswa.2020.113647. [ CrossRef ] [ Google Scholar ]
- Lukwanto R, Irwansyah E. The early detection of diabetes mellitus using fuzzy hierarchical model. Proc Comput Sci. 2015; 59 :312–319. doi: 10.1016/j.procs.2015.07.571. [ CrossRef ] [ Google Scholar ]
- Luo H, Xu G, Li C, Wu Q, et al. Real time artificial intelligence for detection of upper gastrointestinal cancer by endoscopy: a multicentre, case control, diagnostic study. Lancet Oncol. 2019; 20 :1645–1654. doi: 10.1016/S1470-2045(19)30637-0. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Ma F, Sun T, Liu L, Jing H. Detection and diagnosis of chronic kidney disease using deep learning-based heterogeneous modified artificial neural network. Future Gener Comput Syst. 2020; 111 :17–26. doi: 10.1016/j.future.2020.04.036. [ CrossRef ] [ Google Scholar ]
- Matusoka R, Akazawa H, Kodera S. The drawing of the digital era in the management of hypertension. Hypertens Res. 2020; 43 :1135–1140. doi: 10.1161/HYPERTENSIONAHA.120.14742. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Memon M, Li J, Haq A, Memon M. Breast cancer detection in the Iot health environment using modified recursive feature selection. Wirel Commun Mob. 2019; 2019 :19. [ Google Scholar ]
- Mercaldo F, Nardone V, Santone A, Nardone V, Santone A. Diabetes mellitus affected patients classification diagnosis through machine learning techniques through learning through machine learning techniques. Proc Comput Sci. 2017; 112 :2519–2528. doi: 10.1016/j.procs.2017.08.193. [ CrossRef ] [ Google Scholar ]
- Minaee S, Kafieh R, Sonka M, Yazdani S, Soufi G. Deep-COVID: predicting covid-19 from chest X-ray images using deep transfer learning. Comput Vis Pattern Recognit. 2020; 3 :1–9. doi: 10.1016/j.media.2020.101794. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Momin M, Bhagwat N, Dhiwar A, Devekar N. Smart body monitoring system using IoT and machine learning. J Adv Res Electr Electron Instrum Eng Smart Body Syst Using IoT Mach Learn. 2019; 1 :1–7. doi: 10.15662/IJAREEIE.2019.0805010. [ CrossRef ] [ Google Scholar ]
- Morabito F, Campolo M, Leracitano C, Ebadi J, Bonanno L, Barmanti A, Desalvo S, Barmanti P, Ieracitano C. Deep Convolutional neural Network for classification of mild cognitive impaired and Alzheimer’s disease patients from scalp EEG recordings. Res Technol Soc Ind Levaraging Better Tomorrow. 2016 doi: 10.1109/RTSI.2016.7740576. [ CrossRef ] [ Google Scholar ]
- Mueller FB. AI (Artificial Intelligence) and hypertension research. Telemed Technol. 2020; 70 :1–7. doi: 10.1007/s11906-020-01068-8. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Mujumdar A, Vaidehi V. Diabetes prediction using machine learning. Proc Comput Sci. 2019; 165 :292–299. doi: 10.1016/j.procs.2020.01.047. [ CrossRef ] [ Google Scholar ]
- Musleh M, Alajrami E, Khalil A, Nasser B, Barhoom A, Naser S. Predicting liver patients using artificial neural network. J Acad Inf Syst Res. 2019; 3 :1–11. [ Google Scholar ]
- Nahar N, Ara F. Liver disease detection by using different techniques. Elsevier. 2018; 8 :1–9. doi: 10.5121/ijdkp.2018.8201. [ CrossRef ] [ Google Scholar ]
- Nam KH, Kim DH, Choi BK, Han IH. Internet of Things, digital biomarker, and artificial intelligence in spine: current and future perspectives. Neurospine. 2019; 16 :705–711. doi: 10.14245/ns.1938388.194. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Naser S, Naseer I. Lung cancer detection using artificial neural network. J Eng Inf Syst. 2019; 3 :17–23. [ Google Scholar ]
- Nashif S, Raihan R, Islam R, Imam MH. Heart disease detection by using machine learning algorithms and a real-time cardiovascular health monitoring system. Healthc Technol. 2018; 6 :854–873. doi: 10.4236/wjet.2018.64057. [ CrossRef ] [ Google Scholar ]
- Nasser I, Naser S, et al. Predicting tumor category using artificial neural network. Eng Inf Technol. 2019; 3 :1–7. [ Google Scholar ]
- Nazir T, Irtaza A, Shabbir Z, Javed A, Akram U, Tariq M. Artificial intelligence in medicine diabetic retinopathy detection through novel tetragonal local octa patterns and extreme learning machines. Artif Intell Med. 2019; 99 :101695. doi: 10.1016/j.artmed.2019.07.003. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Nensa F, Demircioglu A, Rischipler C. Artificial intelligence in nuclear medicine. J Nucl Med. 2019; 60 :1–10. doi: 10.2967/jnumed.118.220590. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Nithya A, Ahilan A, Venkatadri N, Ramji D, Palagan A. Kidney disease detection and segmentation using artificial neural network and multi kernel k-means clustering for ultrasound images. Measurement. 2020; 149 :106952. doi: 10.1016/j.measurement.2019.106952. [ CrossRef ] [ Google Scholar ]
- Oh K, Chung YC, Kim KW, Kim WS, Oh IS. Classification and visualization of Alzheimer’s disease using volumetric convolutional neural network and transfer learning. Sci Rep. 2019; 9 :1–16. doi: 10.1038/s41598-019-54548-6. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Oomman R, Kalmady KS, Rajan J, Sabu MK. Automatic detection of alzheimer bacilli from microscopic sputum smear images using deep learning methods. Integr Med Res. 2018; 38 :691–699. doi: 10.1016/j.bbe.2018.05.007. [ CrossRef ] [ Google Scholar ]
- Ostovar A, Chimeh E, Fakoorfard Z. The diagnostic value of CT scans in the process of diagnosing COVID-19 in medical centers. Health Technol Assess Act. 2020; 4 :1–7. [ Google Scholar ]
- Owasis M, Arsalan M, Choi J, Mahmood T, Park K. Artificial intelligence based classification of multiple gastrointestinal diseases using endoscopy videos for clinical diagnosis. J Clin Med. 2019; 8 :786. doi: 10.3390/jcm8070986. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Panicker RO, Kalmady KS, Rajan J, Sabu MK. Automatic detection of tuberculosis bacilli from microscopic sputum smear images using deep learning methods. Biocybern Biomed Eng. 2018; 38 (3):691–699. doi: 10.1016/j.bbe.2018.05.007. [ CrossRef ] [ Google Scholar ]
- Park JH, Cho HE, Kim JH, Wall MM, Stern Y, Lim H, Yoo S, Kim HS, Cha J. Machine learning prediction of incidence of Alzheimer’s disease using large-scale administrative health data. Npj Digit Med. 2020 doi: 10.1038/s41746-020-0256-0. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Patel SB. Heart disease using machine learning and data minig techniques. Health Technol. 2016; 10 :1137–1144. [ Google Scholar ]
- Plawiak P, Ozal Y, Tan R, Acharya U. Arrhythmia detection using deep convolution neural network with long duration ECG signals. Comput Biol Med. 2018; 102 :411–420. doi: 10.1016/j.compbiomed.2018.09.009. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Pradhan K, Chawla P. Medical Internet of things using machine learning algorithms for lung cancer detection. J Manag Anal. 2020 doi: 10.1080/23270012.2020.1811789. [ CrossRef ] [ Google Scholar ]
- Rajalakshmi R, Subashini R, Anjana R, Mohan V. Automated diabetic retinopathy detection in smartphone-based fundus photography using artificial intelligence. Eye. 2018; 32 :1138–1144. doi: 10.1038/s41433-018-0064-9. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Rathod J, Wazhmode V, Sodha A, Bhavathankar P (2018) Diagnosis of skin diseases using convolutional neural network. In: Second international conference on electronics, communication and aerospace technology, pp 1048–1051. 10.1109/ICECA.2018.8474593
- Raza M, Awais M, Ellahi W, Aslam N, Nguyen HX, Le-Minh H. Diagnosis and monitoring of Alzheimer’s patients using classical and deep learning techniques. Expert Syst Appl. 2019; 136 :353–364. doi: 10.1016/j.eswa.2019.06.038. [ CrossRef ] [ Google Scholar ]
- Rodrigues J, Matteo A, Ghosh A, Szantho G, Paton J. Comprehensive characterisation of hypertensive heart disease left ventricular pehnotypes. Heart. 2016; 20 :1671–1679. doi: 10.1136/heartjnl-2016-309576. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Rodrigues DA, Ivo RF, Satapathy SC, Wang S, Hemanth J, Filho PPR. A new approach for classification skin lesion based on transfer learning, deep learning, and IoT system. Pattern Recognit Lett. 2020; 136 :8–15. doi: 10.1016/j.patrec.2020.05.019. [ CrossRef ] [ Google Scholar ]
- Romanini J, Barun L, Martins M, Carrard V. Continuing education activities improve dentists self efficacy to manage oral mucosal lesions and oral cancer. Eur J Dent Educ. 2020; 25 :28–34. [ PubMed ] [ Google Scholar ]
- Romero MP, Chang Y, Brunton LA, Parry J, Prosser A, Upton P, Rees E, Tearne O, Arnold M, Stevens K, Drewe JA. Decision tree machine learning applied to bovine alzheimer risk factors to aid disease control decision making. Prev Vet Med. 2020; 175 :104860. doi: 10.1016/j.prevetmed.2019.104860. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Sabottke C, Spieler B. The effect of image resolution on deep learning in radiography. Radiology. 2020; 2 :e190015. doi: 10.1148/ryai.2019190015. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Sakr S, El Shawi R, Ahmed A, Blaha M, et al. Using machine learning on cardiorespiratory fitness data for predicting hypertension: the henry ford exercise testing project. PLoS One. 2018; 13 :1–18. doi: 10.1371/journal.pone.0195344. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Santroo A, Clemente F, Baioochi C, Bianchi C, Falciani F, Valente S, et al. From near-zero to zero fluoroscopy catheter ablation procedures. J Cardiovasc Electrophys. 2019; 30 :2397–2404. doi: 10.1111/jce.14121. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Saranya E, Maheswaran T. IOT based disease prediction and diagnosis system for healthcare. Healthc Technol. 2019; 7 :232–237. [ Google Scholar ]
- Sarao V, Veritti D, Paolo L. Automated diabetic retinopathy detection with two different retinal imaging devices using artificial intelligence. Graefe’s Arch Clin Exp Opthamol. 2020 doi: 10.1007/s00417-020-04853-y. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Sathitratanacheewin S, Sunanta P, Pongpirul K. Heliyon deep learning for automated classification of Alzheimer-related chest X-ray: dataset distribution shift limits diagnostic performance generalizability. Heliyon. 2020; 6 :e04614. doi: 10.1016/j.heliyon.2020.e04614. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Shabut AM, Hoque M, Lwin KT, Evans BA, Azah N, Abu-hassan KJ, Hossain MA. An intelligent mobile-enabled expert system for alzheimer disease diagnosis in real time. Expert Syst Appl. 2018; 114 :65–77. doi: 10.1016/j.eswa.2018.07.014. [ CrossRef ] [ Google Scholar ]
- Shkolyar E, Jia X, Chnag T, Trivedi D. Augmented bladder tumor detection using deep learning. Eur Urol. 2019; 76 :714–718. doi: 10.1016/j.eururo.2019.08.032. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Singh N, Moody A, Leung G, Ravikumar R, Zhan J, Maggissano R, Gladstone D. Moderate carotid artery stenosis: MR imaging depicted intraplaque hemorrhage predicts risk of cerebovascular ischemic events in asymptomatic men. Radiology. 2009; 252 :502–508. doi: 10.1148/radiol.2522080792. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Singh J, Tripathy A, Garg P, Kumar A. Lung Alzheimer detection using anti-aliased convolutional networks networks. Proc Comput Sci. 2020; 173 :281–290. doi: 10.1016/j.eswa.2018.07.014. [ CrossRef ] [ Google Scholar ]
- Skaane P, Bandos A, Gullien R, Eben E, Ekseth U, Izadi M, Jebsen I, Gur D. Comparison of digital mammography alone and digital mammography plus tomo-sysnthesis in a population based screening program. Radiology. 2013; 267 :47–56. doi: 10.1148/radiol.12121373. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Sloun R, Cohen R, Eldar Y. Deep learning in ultrasound imaging. IEEE. 2019; 108 :11–29. doi: 10.1109/JPROC.2019.2932116. [ CrossRef ] [ Google Scholar ]
- Soundarya S, Sruthi MS, Sathya BS, Kiruthika S, Dhiyaneswaran J. Early detection of Alzheimer disease using gadolinium material. Mater Today Proc. 2020 doi: 10.1016/j.matpr.2020.03.189. [ CrossRef ] [ Google Scholar ]
- Spann A, Yasodhara A, Kang J, Watt K, Wang B, Bhat M, Goldenberg A. Applying machine learning in liver disease and transplantation: a survey. Hepatology. 2020; 71 :1093–1105. doi: 10.1002/hep.31103. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Srinivasu PN, SivaSai JG, Ijaz MF, Bhoi AK, Kim W, Kang JJ. Classification of skin disease using deep learning neural networks with MobileNet V2 and LSTM. Sensors. 2021; 21 (8):2852. doi: 10.3390/s21082852. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Srinivasu PN, Ahmed S, Alhumam A, Kumar AB, Ijaz MF. An AW-HARIS based automated segmentation of human liver using CT images. Comput Mater Contin. 2021; 69 (3):3303–3319. [ Google Scholar ]
- Subasi A. Use of artificial intelligence in Alzheimer’s disease detection. AI Precis Health. 2020 doi: 10.1016/B978-0-12-817133-2.00011-2. [ CrossRef ] [ Google Scholar ]
- Swapna G, Vinayakumar R, Soman KP. Diabetes detection using deep learning algorithms. ICT Express. 2018; 4 :243–246. doi: 10.1016/j.icte.2018.10.005. [ CrossRef ] [ Google Scholar ]
- Tang LYW, Coxson HO, Lam S, Leipsic J, Tam RC, Sin DD. Articles towards large-scale case-finding: training and validation of residual networks for detection of chronic obstructive pulmonary disease using low-dose CT. Lancet Digit Health. 2020; 2 :e259–e267. doi: 10.1016/S2589-7500(20)30064-9. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Tegunov D, Cramer P. Real-time cryo-electron microscopy data preprocessing with warp. Nat Med. 2019; 16 :1146–1152. doi: 10.1038/s41592-019-0580-y. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Thai DT, Minh QT, Phung PH (2017) Toward an IoT-based expert system for heart disease diagnosis. In: Modern artificial intelligence and cognitive science conference, vol 1964, pp 157–164
- Tigga NP, Garg S. Prediction of type 2 diabetes using machine learning prediction of type 2 diabetes using machine learning classification methods classification methods. Proc Comput Sci. 2020; 167 :706–716. doi: 10.1016/j.procs.2020.03.336. [ CrossRef ] [ Google Scholar ]
- TranX B, Latkin A, Lan H, Ho R, Ho C, et al. The current research landscap of the application of artificial intelligence in managing cerebovasclar and heart disease. J Environ Res Public health. 2019; 16 :2699. doi: 10.3390/ijerph16152699. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Tschandl P, Nisa B, Cabo H, Kittler H, Zalaudek I. Expert level diagnosis of non pigmented skin cancer by combined convolution neural networks. Jama Dermatol. 2019; 155 :58–65. doi: 10.1001/jamadermatol.2018.4378. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Tuli S, Basumatary N, Gill SS, Kahani M, Arya RC, Wander GS. HealthFog: an ensemble deep learning based smart healthcare system for automatic diagnosis of heart diseases in integrated IoT and fog computing environments. Future Gener Comput Syst. 2019; 104 :187–200. doi: 10.1016/j.future.2019.10.043. [ CrossRef ] [ Google Scholar ]
- Uehera D, Hayashi Y, Seki Y, Kakizaki S, Horiguchi N, Tojima H, Yamazaki Y, Sato K, Yasuda K, Yamada M, Uraoka T, Kasama K. Non invasive prediction of non alchlolic steatohepatitus in Japanses patiens with morbid obesity by artificial intelligence using rule extraction technology. World J Hepatol. 2018; 10 :934–943. doi: 10.4254/wjh.v10.i12.934. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Ullah R, Khan S, Ishtiaq I, Shahzad S, Ali H, Bilal M. Cost effective and efficient screening of Alzheimer disease with Raman spectroscopy and machine learning algorithms. Photodiagn Photodyn Ther. 2020; 32 :101963. doi: 10.1016/j.pdpdt.2020.101963. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Uysal G, Ozturk M. Hippocampal atrophy based Alzheimer’s disease diagnosis via machine learning methods. J Neurosci Methods. 2020; 337 :1–9. doi: 10.1016/j.jneumeth.2020.108669. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Vasal S, Jain S, Verma A. COVID-AI: an artificial intelligence system to diagnose COVID 19 disease. J Eng Res Technol. 2020; 9 :1–6. [ Google Scholar ]
- Wang Z, Zhang H, Kitai T. Artificial Intelligence in precision cardiovascular medicine. J Am Coll Cardiol. 2017; 69 :2657–2664. doi: 10.1016/j.jacc.2017.03.571. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Wang Z, Chung JW, Jiang X, Cui Y, Wang M, Zheng A. Machine learning-based prediction system for chronic kidney disease using associative classification technique. Int J Eng Technol. 2018; 7 :1161–1167. doi: 10.14419/ijet.v7i4.36.25377. [ CrossRef ] [ Google Scholar ]
- Woldargay A, Arsand E, Botsis T, Mamyinka L. Data driven glucose pattern classification and anomalies detection. J Med Internet Res. 2019; 21 :e11030. doi: 10.2196/11030. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Yadav D, Pal S. Prediction of thyroid disease using decision tree ensemble method. Hum Intell Syst Integr. 2020 doi: 10.1007/s42454-020-00006-y. [ CrossRef ] [ Google Scholar ]
- Yang J, Min B, Kang J. A feasibilty study of LYSO-GAPD detector for DEXA applications. J Instrum. 2020 doi: 10.1088/1748-0221/15/05/P05017. [ CrossRef ] [ Google Scholar ]
- Yue W, Wang Z, Chen H, Payne A, Liu X. Machine learning with applications in breast cancer diagnosis and prognosis. Designs. 2018; 2 :1–17. doi: 10.3390/designs2020013. [ CrossRef ] [ Google Scholar ]
- Zaar O, Larson A, Polesie S, Saleh K, Olives A, et al. Evaluation of the diagnositic accuracy of an online artificial intelligence application for skin disease diagnosis. Acta Derm Venereol. 2020; 100 :1–6. doi: 10.2340/00015555-3624. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Zebene A, Årsand E, Walderhaug S, Albers D, Mamykina L, Botsis T, Hartvigsen G. Data-driven modeling and prediction of blood glucose dynamics: Machine learning applications in type 1 diabetes. Artif Intell Med. 2019; 98 :109–134. doi: 10.1016/j.artmed.2019.07.007. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Zhang R, Simon G, Yu F. Advancing Alzheimer’s research: a review of big data promises. J Med Inform. 2017; 106 :48–56. doi: 10.1016/j.ijmedinf.2017.07.002. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Zhang F, Zhang T, Tian C, Wu Y, Zhou W, Bi B, et al. Radiography of direct drive double shell targets with hard X-rays generated by a short pulse laser. Nucl Fusion. 2019 doi: 10.1088/1741-4326/aafe30. [ CrossRef ] [ Google Scholar ]
- Zhou Z, Yang L, Gao J, Chen X. Structure–relaxivity relationships of magnetic nanoparticles for magnetic resonance imaging. Adv Mater. 2019; 31 :1804567. doi: 10.1002/adma.201804567. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
A systematic review into the assessment of medical apps: motivations, challenges, recommendations and methodological aspect
- Review Paper
- Published: 23 June 2020
- Volume 10 , pages 1045–1061, ( 2020 )
Cite this article
- A. H. Alamoodi ORCID: orcid.org/0000-0003-4393-5570 1 ,
- Salem Garfan 1 ,
- B. B. Zaidan 1 ,
- A. A. Zaidan 1 ,
- Moceheb Lazam Shuwandy 2 ,
- Mussab Alaa 1 ,
- M. A. Alsalem 3 ,
- Ali Mohammed 4 ,
- A. M. Aleesa 5 ,
- O. S. Albahri 1 ,
- Ward Ahmed Al-Hussein 6 &
- O. R. Alobaidi 4
1239 Accesses
28 Citations
5 Altmetric
Explore all metrics
Recent years have shown significantly pervasive interest in mobile applications (hereinafter “apps”). The number and popularity of these apps are dramatically increasing. Even though mobile apps are diverse, countless ones are available through many platforms. Some of these apps are not useful nor do they possess rich content, which benefits end users as expected, especially in medical-related cases. This research aims to review and analyze articles associated with medical app assessment across different platforms. This research also aimed to provide the best practices and identify the academic challenges, motivations and recommendations related with quality assessments. In addition, a methodological approach followed in previous research in this domain was also discussed to give some insights for future comers with what to expect. We systematically searched articles on topics related to medical app assessment. The search was conducted on five major databases, namely, Science Direct, Springer, Web of Science, IEEE Xplore and PubMed from 2009 to September 2019. These indices were considered sufficiently extensive and reliable to cover our scope of the literature. Articles were selected on the basis of our inclusion and exclusion criteria ( n = 72 ). Medical app assessment is considered a major topic which warrants attention. This study emphasizes the current standpoint and opportunities for research in this area and boosts additional efforts towards the understanding of this research field.
This is a preview of subscription content, log in via an institution to check access.
Access this article
Price includes VAT (Russian Federation)
Instant access to the full article PDF.
Rent this article via DeepDyve
Institutional subscriptions
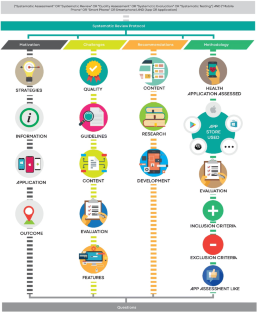
Similar content being viewed by others
Qualitative evaluation of mobile cancer apps with particular attention to the target group, content, and advertising.
Cathleen Böhme, Marc Baron von Osthoff, … Jutta Hübner

Evaluating and selecting mobile health apps: strategies for healthcare providers and healthcare organizations
Edwin D Boudreaux, Molly E Waring, … Sherry Pagoto
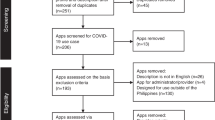
Mobile applications in the Philippines during the COVID-19 pandemic: systematic search, use case mapping, and quality assessment using the Mobile App Rating Scale (MARS)
Aldren Gonzales, Razel Custodio, … Mary Ann Ladia
Holl K, Elberzhager F. Mobile application quality assurance. Adv Comput. 2019;112:1–77 Elsevier.
Google Scholar
Bahadori S, Wainwright TW, Ahmed OH. Smartphone apps for total hip replacement and total knee replacement surgery patients: a systematic review. Disabil Rehabil. 2018:1–6.
Orsini G, Bade D, Lamersdorf W. Context-aware computation offloading for mobile cloud computing: requirements analysis, survey and design guideline. Procedia Comput Sci. 2015;56:10–7.
Beam L, Burrows B, Dobey Z, Poser R, Sopko M. RecycMe: the Ohio State University recycling phone application. 2013.
Ouhbi S, Fernández-Alemán JL, Pozo JR, El Bajta M, Toval A, Idri A. Compliance of blood donation apps with mobile OS usability guidelines. J Med Syst. 2015;39(6):63.
Kim MS, Park JH, Park K-Y. Development and effectiveness of a drug dosage calculation training program using cognitive loading theory based on smartphone application. J Korean Acad Nurs. 2012;42(5):689–98.
Nayebi F, Desharnais J-M, Abran A. The state of the art of mobile application usability evaluation. In 2012 25th IEEE Canadian Conference on Electrical and Computer Engineering (CCECE). IEEE; 2012, p. 1–4.
Chen Z-S, Li R, Chen X, Xu H. A survey study on consumer perception of mobile-commerce applications. Procedia Environ Sci. 2011;11:118–24.
Tang AK. A systematic literature review and analysis on mobile apps in m-commerce: implications for future research. Electron Commer Res Appl. 2019;37:100885.
Darras KE, van Merriënboer JJG, Toom M, Roberson ND, de Bruin ABH, Nicolaou S, et al. Developing the evidence base for M-learning in undergraduate radiology education: identifying learner preferences for Mobile apps. Can Assoc Radiol J. 2019;70(3):320–6.
Albrecht U-V, Hillebrand U, von Jan U. Relevance of trust marks and CE labels in German-language store descriptions of health apps: analysis. JMIR mHealth and uHealth. 2018;6(4):e10394.
Anderson N, Steele J, O'Neill L-A, Harden LA. Pokémon Go: mobile app user guides. Br J Sports Med . 2016;2016:096762.
Ahtinen A, Isomursu M, Huhtala Y, Kaasinen J, Salminen J, Häkkilä J. Tracking outdoor sports–user experience perspective. In: Aarts E, Crowley JL, Ruyter B, Gerhäuser H, Pflaum A, Schmidt J, Wichert R, editors. European Conference on Ambient Intelligence. Berlin: Springer; 2008. p. 192–209.
Lior LN. Writing for interaction: crafting the information experience for web and software apps. Newnes. 2013, Writing Text for Interaction.
Cortimiglia MN, Ghezzi A, Renga F. Mobile applications and their delivery platforms. IT Prof. 2011;13(5):51–6.
Beimborn D, Palitza M. Enterprise app stores for mobile applications-development of a benefits framework. 2013.
Harman M, Jia Y, Zhang Y. App store mining and analysis: MSR for app stores. In Proceedings of the 9th IEEE Working Conference on Mining Software Repositories. IEEE Press; 2012, p. 108–111.
Freier A. App revenue reaches $92.1 billion in 2018 driven by mobile gaming apps. Business Apps. 2018;13(09).
Cheney S, Thompson E. The 2017–2022 app economy forecast: 6 billion devices, $157 billion in spend & more. App Annie. 2018.
Chen J, Cade JE, Allman-Farinelli M. The most popular smartphone apps for weight loss: a quality assessment. JMIR mHealth uHealth. 2015;3(4):e104.
Kim BY, Sharafoddini A, Tran N, Wen EY, Lee J. Consumer mobile apps for potential drug-drug interaction check: systematic review and content analysis using the mobile app rating scale (MARS). JMIR mHealth uHealth. 2018;6(3):e74.
Haskins BL, Lesperance D, Gibbons P, Boudreaux ED. A systematic review of smartphone applications for smoking cessation. Transl Behav Med. 2017;7(2):292–9.
Ali EE, Teo AKS, Goh SXL, Chew L, Yap KY-L. MedAd-AppQ: a quality assessment tool for medication adherence apps on iOS and android platforms. Res Soc Adm Pharm. 2018;14(12):1125–33.
Muntaner-Mas A, Martinez-Nicolas A, Lavie CJ, Blair SN, Ross R, Arena R, et al. A systematic review of fitness apps and their potential clinical and sports utility for objective and remote assessment of cardiorespiratory fitness. Sports Med. 2019;49(4):587–600.
Zhao J, Freeman B, Li M. How do infant feeding apps in China measure up? A Content Quality Assessment. JMIR mHealth uHealth. 2017;5(12):e186.
Weekly T, Walker N, Beck J, Akers S, Weaver M. A review of apps for calming, relaxation, and mindfulness interventions for pediatric palliative care patients. Children . 2018;5(2):16.
Nicholas J, Larsen ME, Proudfoot J, Christensen H. Mobile apps for bipolar disorder: a systematic review of features and content quality. J Med Internet Res. 2015;17(8):e198.
Huckvale K, Car M, Morrison C, Car J. Apps for asthma self-management: a systematic assessment of content and tools. BMC Med. 2012;10(1):144.
Zhang MW, Ho RC, Hawa R, Sockalingam S. Analysis of the information quality of bariatric surgery smartphone applications using the silberg scale. Obes Surg. 2016;26(1):163–8.
Bergeron D, et al. Mobile applications in neurosurgery: a systematic review, quality audit, and survey of Canadian neurosurgery residents. World neurosurg. 2019.
van Galen L, Xu X, Koh M, Thng S, Car J. Eczema apps conformance with clinical guidelines: a systematic assessment of functions, tools and content. Br J Dermatol. 2019.
Larco A, Enríquez F, Luján-Mora S. Review and evaluation of special education iOS Apps using MARS. In 2018 IEEE World Engineering Education Conference (EDUNINE). IEEE; 2018, p. 1–6.
Larco A, Montenegro C, Luján-Mora S, Quality improvement criteria of apps in Spanish for people with disabilities. In 2018 4th International Conference on Information Management (ICIM). IEEE; 2018, p. 260–264.
Alamoodi A, et al. A review of data analysis for early-childhood period: taxonomy, motivations, challenges, recommendation, and methodological aspects. IEEE Access. 2019;7:51069–103.
Burgers C, Brugman BC, Boeynaems A. Systematic literature reviews: four applications for interdisciplinary research. J Pragmat. 2019;145:102–9.
Loureiro SMC, Romero J, Bilro RG. Stakeholder engagement in co-creation processes for innovation: a systematic literature review and case stud. J Bus Res. 2019.
Kushwah S, Dhir A, Sagar M, Gupta B. Determinants of organic food consumption. A systematic literature review on motives and barriers. Appetite. 2019;143:104402.
Daigneault P-M, Jacob S, Ouimet M. Using systematic review methods within a Ph. D. Dissertation in political science: challenges and lessons learned from practice. Int J Soc Res Methodol. 2014;17(3):267–83.
Ain N, Vaia G, DeLone WH, Waheed M. Two decades of research on business intelligence system adoption, utilization and success – a systematic literature review. Decis Support Syst. 2019;125:113113.
Dani VS, Freitas CMDS, Thom LH. Ten years of visualization of business process models: a systematic literature review. Comput Stand Inter. 2019.
Owens OL, Beer JM, Reyes LI, Thomas TL. Systematic review of commercially available mobile phone applications for prostate cancer education. Am J Men’s Health. 2019;13(1):1557988318816912.
Huckvale K, Morrison C, Ouyang J, Ghaghda A, Car J. The evolution of mobile apps for asthma: an updated systematic assessment of content and tools. BMC Med. 2015;13(1):58.
El-Gayar O, Timsina P, Nawar N, Eid W. Mobile applications for diabetes self-management: status and potential. J Diabetes Sci Technol. 2013;7(1):247–62.
Huang Z, Lum E, Jimenez G, Semwal M, Sloot P, Car J. Medication management support in diabetes: a systematic assessment of diabetes self-management apps. BMC Med. 2019;17(1):127.
Dayer L, Heldenbrand S, Anderson P, Gubbins PO, Martin BC. Smartphone medication adherence apps: potential benefits to patients and providers. J Am Pharm Assoc. 2013;53(2):172–81.
Nguyen AD, Baysari MT, Kannangara DRW, Tariq A, Lau AYS, Westbrook JI, et al. Mobile applications to enhance self-management of gout. Int J Med Inform. 2016;94:67–74.
Payo RM, Harris J, Armes J. Prescribing fitness apps for people with cancer: a preliminary assessment of content and quality of commercially available apps. J Cancer Surviv. 2019;13:1–9.
Rusin M, Årsand E, Hartvigsen G. Functionalities and input methods for recording food intake: a systematic review. Int J Med Inform. 2013;82(8):653–64.
Bhattarai P, Newton-John T, Phillips JL. Quality and usability of arthritic pain self-management apps for older adults: a systematic review. Pain Med. 2017;19(3):471–84.
Devan H, Farmery D, Peebles L, Grainger R. Evaluation of self-management support functions in apps for people with persistent pain: systematic review. JMIR mHealth uHealth. 2019;7(2):e13080.
Metelmann B, Metelmann C, Schuffert L, Hahnenkamp K, Brinkrolf P. Medical correctness and user friendliness of available apps for cardiopulmonary resuscitation: systematic search combined with guideline adherence and usability evaluation. JMIR mHealth uHealth. 2018;6(11):e190.
Taki S, Campbell KJ, Russell CG, Elliott R, Laws R, Denney-Wilson E. Infant feeding websites and apps: a systematic assessment of quality and content. Interact J Med Res. 2015;4(3):e18.
Lee H, Sullivan SJ, Schneiders AG, Ahmed OH, Balasundaram AP, Williams D, et al. Smartphone and tablet apps for concussion road warriors (team clinicians): a systematic review for practical users. Br J Sports Med. 2015;49(8):499–505.
Moglia ML, Nguyen HV, Chyjek K, Chen KT, Castaño PM. Evaluation of smartphone menstrual cycle tracking applications using an adapted APPLICATIONS scoring system. Obstet Gynecol. 2016;127(6):1153–60.
Brouard B, Bardo P, Bonnet C, Mounier N, Vignot M, Vignot S. Mobile applications in oncology: is it possible for patients and healthcare professionals to easily identify relevant tools? Ann Med. 2016;48(7):509–15.
Latorre GF, de Fraga R, Seleme MR, Mueller CV, Berghmans B. An ideal e-health system for pelvic floor muscle training adherence: systematic review. Neurourol Urodyn. 2019;38(1):63–80.
Luo D, Wang P, Lu F, Elias J, Sparks JA, Lee YC. Mobile apps for individuals with rheumatoid arthritis: a systematic review. JCR: J Clin Rheumatol. 2019;25(3):133–41.
Sun C, Malcolm JC, Wong B, Shorr R, Doyle M-A. Improving glycemic control in adults and children with type 1 diabetes with the use of smartphone-based mobile applications: a systematic review. Can J Diabetes. 2019;43(1):51–8. e3.
Bry LJ, Chou T, Miguel E, Comer JS. Consumer smartphone apps marketed for child and adolescent anxiety: a systematic review and content analysis. Behav Ther. 2018;49(2):249–61.
Milani P, Coccetta CA, Rabini A, Sciarra T, Massazza G, Ferriero GJP. Mobile smartphone applications for body position measurement in rehabilitation: a review of goniometric tools. PM&R. 2014;6(11):1038–43.
Kalz M, et al. Smartphone apps for cardiopulmonary resuscitation training and real incident support: a mixed-methods evaluation study. J Med Internet Res. 2014;16(3):e89.
Piran P, et al. Medical mobile applications for stroke survivors and caregivers. J Stroke Cerebrovasc Dis. 2019;28(11):104318.
Adam A, Hellig JC, Perera M, Bolton D, Lawrentschuk N. ‘Prostate Cancer risk Calculator’ mobile applications (apps): a systematic review and scoring using the validated user version of the Mobile application rating scale (uMARS). World J Urol. 2018;36(4):565–73.
Schumer H, Amadi C, Joshi A. Evaluating the dietary and nutritional apps in the Google play store. Healthcare Inform Res. 2018;24(1):38–45.
Torous J, Levin ME, Ahern DK, Oser ML. Cognitive behavioral mobile applications: clinical studies, marketplace overview, and research agenda. Cogn Behav Pract. 2017;24(2):215–25.
Anthony Berauk VL, Murugiah MK, Soh YC, Chuan Sheng Y, Wong TW, Ming LC. Mobile health applications for caring of older people: review and comparison. Ther Innov Regul Sci. 2018;52(3):374–82.
Meghani SH, MacKenzie MA, Morgan B, Kang Y, Wasim A, Sayani S. Clinician-targeted mobile apps in palliative care: a systematic review. J Palliat Med. 2017;20(10):1139–47.
Rincon E, Monteiro-Guerra F, Rivera-Romero O, Dorronzoro-Zubiete E, Sanchez-Bocanegra CL, Gabarron E. Mobile phone apps for quality of life and well-being assessment in breast and prostate cancer patients: systematic review. JMIR mHealth uHealth. 2017;5(12):e187.
Chen E, Mangone ER. A systematic review of apps using mobile criteria for adolescent pregnancy prevention (mCAPP). JMIR mHealth uHealth. 2016;4(4):e122.
Alyami M, Giri B, Alyami H, Sundram F. Social anxiety apps: a systematic review and assessment of app descriptors across mobile store platforms. Evid-Based Ment Health. 2017;20(3):65–70.
Park JYE, Li J, Howren A, Tsao NW, De Vera M. Mobile phone apps targeting medication adherence: quality assessment and content analysis of user reviews. JMIR mHealth uHealth. 2019;7(1):e11919.
Byambasuren O, Sanders S, Beller E, Glasziou P. Prescribable mHealth apps identified from an overview of systematic reviews. Digit Med. 2018;1(1):12.
Short CE, Finlay A, Sanders I, Maher C. Development and pilot evaluation of a clinic-based mHealth app referral service to support adult cancer survivors increase their participation in physical activity using publicly available mobile apps. BMC Health Serv Res. 2018;18(1):27.
Bender JL, Yue RYK, To MJ, Deacken L, Jadad AR. A lot of action, but not in the right direction: systematic review and content analysis of smartphone applications for the prevention, detection, and management of cancer. J Med Internet Res. 2013;15(12):e287.
Bychkov D, Young SD. Facing up to nomophobia: a systematic review of mobile phone apps that reduce Smartphone usage. In Big data in engineering applications. Springer; 2018, p. 161–171.
Olivero E, Bert F, Thomas R, Scarmozzino A, Raciti IM, Gualano MR, et al. E-tools for hospital management: an overview of smartphone applications for health professionals. Int J Med Inform. 2019;124:58–67.
Rodríguez AQ, Wägner AM. Mobile phone applications for diabetes management: a systematic review. Endocrinol Diab Nutr. 2019;66(5):330–7.
Reynoldson C, Stones C, Allsop M, Gardner P, Bennett MI, Closs SJ, et al. Assessing the quality and usability of smartphone apps for pain self-management. Pain Med. 2014;15(6):898–909.
Rajani NB, Weth D, Mastellos N, Filippidis FT. Adherence of popular smoking cessation mobile applications to evidence-based guidelines. BMC Public Health. 2019;19(1):743.
Xiao Q, Wang Y, Sun L, Lu S, Wu Y. Current status and quality assessment of cardiovascular diseases related smartphone apps in China. Nurs Inform. 2016;225:1030–1.
Sedrati H, Nejjari C, Chaqsare S, Ghazal H. Mental and physical mobile health apps. Procedia Comput Sci. 2016;100:900–6.
Huckvale K, Prieto JT, Tilney M, Benghozi P-J, Car J. Unaddressed privacy risks in accredited health and wellness apps: a cross-sectional systematic assessment. BMC Med. 2015;13(1):214.
Larco A, Yanez C, Almendáriz V, Luján-Mora S. Thinking about inclusion: Assessment of multiplatform apps for people with disability. In 2018 IEEE Global Engineering Education Conference (EDUCON). IEEE; 2018, pp. 350–354.
Seabrook HJ, Stromer JN, Shevkenek C, Bharwani A, de Grood J, Ghali WA. Medical applications: a database and characterization of apps in Apple iOS and Android platforms. BMC Res Notes. 2014;7(1):573.
Buechi R, et al. Evidence assessing the diagnostic performance of medical smartphone apps: a systematic review and exploratory meta-analysis. BMJ Open. 2017;7(12):e018280.
Mangone ER, Lebrun V, Muessig KE. Mobile phone apps for the prevention of unintended pregnancy: a systematic review and content analysis. JMIR mHealth uHealth. 2016;4(1):e6.
Williams JP, Schroeder D. Popular glucose tracking apps and use of mHealth by Latinos with diabetes. JMIR mHealth uHealth. 2015;3(3):e84.
Con D, De Cruz P. Mobile phone apps for inflammatory bowel disease self-management: a systematic assessment of content and tools. JMIR mHealth uHealth. 2016;4(1):e13.
Linares-Del Rey M, Vela-Desojo L, Cano-de la Cuerda R. Mobile phone applications in Parkinson’s disease: a systematic review. Neurología (English Edition). 2018.
Larsen ME, Nicholas J, Christensen H. A systematic assessment of smartphone tools for suicide prevention. PloS One. 2016;11(4):e0152285.
Huckvale K, Adomaviciute S, Prieto JT, Leow MK-S, Car J. Smartphone apps for calculating insulin dose: a systematic assessment. BMC Med. 2015;13(1):106.
Bachmann DJ, Jamison NK, Martin A, Delgado J, Kman NE. Emergency preparedness and disaster response: there’s an app for that. Prehosp Dis Med. 2015;30(5):486–90.
Bakker D, Kazantzis N, Rickwood D, Rickard N. Mental health smartphone apps: review and evidence-based recommendations for future developments. JMIR Ment Health. 2016;3(1):e7.
Wurzer P, Parvizi D, Lumenta DB, Giretzlehner M, Branski LK, Finnerty CC, et al. Smartphone applications in burns. Burns. 2015;41(5):977–89.
Hayes W, Naziri Q, De Tolla JE, Akamnonu CP, Merola AA, Paulino C. A systematic review of all smart phone applications specifically aimed for use as a scoliosis screening tool. Spine J. 2013;13(9):S38.
Download references
this research is supported by Universiti Pendidikan Sultan Idris under University Research Grant (2017–0310–107-01).
Author information
Authors and affiliations.
Department of Computing, Sultan Idris University of Education (UPSI), Tanjong Malim, Malaysia
A. H. Alamoodi, Salem Garfan, B. B. Zaidan, A. A. Zaidan, Mussab Alaa & O. S. Albahri
Computer Science Department, College of Computer Science and Mathematics, Tikrit University (TU), Tikrit, Iraq
Moceheb Lazam Shuwandy
Department of Management Information System, College of Administration and Economics, University of Mosul, Mosul, Iraq
M. A. Alsalem
Faculty of Engineering and Built Environment, Universiti Kebangaan Malaysia (UKM), Bangi, Selangor, Malaysia
Ali Mohammed & O. R. Alobaidi
Department of Engineering Technology, Universiti Tun Hussein Onn (UTHM), Batu Pahat, Malaysia
A. M. Aleesa
Faculty of Computer Science and Information Technology, University of Malaya (UM), Kuala Lumpur, Malaysia
Ward Ahmed Al-Hussein
You can also search for this author in PubMed Google Scholar
Corresponding author
Correspondence to A. H. Alamoodi .
Ethics declarations
Disclosure of potential conflicts of interest.
The authors declare that they have no conflict of interest.
Research involving human participants and/or animals
This article does not contain any studies with human participants or animals performed by any of the authors.
Conflict of interest
The authors declare that they have no competing of interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
(DOCX 14 kb)
Rights and permissions
Reprints and permissions
About this article
Alamoodi, A.H., Garfan, S., Zaidan, B.B. et al. A systematic review into the assessment of medical apps: motivations, challenges, recommendations and methodological aspect. Health Technol. 10 , 1045–1061 (2020). https://doi.org/10.1007/s12553-020-00451-4
Download citation
Received : 27 April 2020
Accepted : 11 June 2020
Published : 23 June 2020
Issue Date : September 2020
DOI : https://doi.org/10.1007/s12553-020-00451-4
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Apps assessment
- Mobile apps
- Medical apps
- Find a journal
- Publish with us
- Track your research

IMAGES
VIDEO
COMMENTS
In the literature review for each medical condition are sections that describe its prevalence in the U.S. population, effects on the functional abilities needed for safe driving, effects on driving performance, and relationships with motor vehicle crash and violation risk. A
Literature reviews are in great demand in most scientific fields. Their need stems from the ever-increasing output of scientific publications .For example, compared to 1991, in 2008 three, eight, and forty times more papers were indexed in Web of Science on malaria, obesity, and biodiversity, respectively .Given such mountains of papers, scientists cannot be expected to examine in detail every ...
Literature reviews are most commonly performed to help answer a particular question. While you are at medical school, there will usually be some choice regarding the area you are going to review. Once you have identified a subject area for review, the next step is to formulate a specific research question. This is arguably the most important ...
Purpose and Importance of the Literature Review. An understanding of the current literature is critical for all phases of a research study. Lingard 9 recently invoked the "journal-as-conversation" metaphor as a way of understanding how one's research fits into the larger medical education conversation. As she described it: "Imagine yourself joining a conversation at a social event.
Literature reviews play a critical role in scholarship because science remains, first and foremost, a cumulative endeavour (vom Brocke et al., 2009). As in any academic discipline, rigorous knowledge syntheses are becoming indispensable in keeping up with an exponentially growing eHealth literature, assisting practitioners, academics, and graduate students in finding, evaluating, and ...
Doing a Literature Review in Health33 This chapter describes how to undertake a rigorous and thorough review of the literature and is divided into three sections. The first section examines the two main types of review: the narrative and the systematic review. The second section describes some techniques for undertaking a comprehensive search,
Run a few sample database searches to make sure your research question is not too broad or too narrow. If possible, discuss your topic with your professor. 2. Determine the scope of your review. The scope of your review will be determined by your professor during your program. Check your assignment requirements for parameters for the Literature ...
The purpose of the literature review section of a manuscript is not to report what is known about your topic. The purpose is to identify what remains unknown—what academic writing scholar Janet Giltrow has called the 'knowledge deficit'—thus establishing the need for your research study [].In an earlier Writer's Craft instalment, the Problem-Gap-Hook heuristic was introduced as a way ...
Additionally, the assessment and determination of the clinical meaning of fatigue and its multidimensionality may vary by medical condition. Methods: A scoping literature review was conducted to investigate how fatigue is defined and measured, including its dimensions, in non-oncologic medical conditions. The PubMed database was searched using ...
Examples of literature reviews. Step 1 - Search for relevant literature. Step 2 - Evaluate and select sources. Step 3 - Identify themes, debates, and gaps. Step 4 - Outline your literature review's structure. Step 5 - Write your literature review.
This volume focuses on indicators for care of general medical conditions. Each chapter summarizes the results of the literature review for a particular condition, provides RAND staff's recommended indicators based on that review, and notes the level of scientific evidence supporting each indicator along with the relevant citations.
These steps for conducting a systematic literature review are listed below. Also see subpages for more information about: What are Literature Reviews? ... Cook, D. A., & West, C. P. (2012). Conducting systematic reviews in medical education: a stepwise approach. Medical Education, 46(10), 943-952. << Previous: Critical Appraisal Resources ...
Medical conditions can increase drowning risk. No prior study has systematically reviewed the published evidence globally regarding medical conditions and drowning risk for adults. MEDLINE (Ovid), PubMed, EMBASE, Scopus, PsycINFO (ProQuest) and SPORTDiscus databases were searched for original research published between 1 January 2005 and 31 October 2021 that reported adult (≥15 years) fatal ...
conditions as medical conditions that have occurred for at least three months and involve activities of daily living deficits or increased medical needs that are exacerbated for . ... systematic literature review, each article was screened by the three categories established exclusively for this research. The three categories are listed as ...
This effort presents updated research findings describing the effect of medical conditions on driving performance and safety. Researchers conducted a preliminary literature search and discussion with driving safety professionals providing information that was used to select the medical conditions for review: attention deficit hyperactive disorder (ADHD); autism spectrum disorder (ASD ...
A systematic review of the quantitative literature on quality of life in individuals with rare genetic conditions (Cohen and Biesecker 2010), revealed that a large number of quality of life studies focus on disease‐related variables, keeping a bio‐medical model that fails to incorporate the patient‐centered perspective and hence explore ...
Using the National Library of Medicine (NLM) database PubMed, we first identified 18 peer reviewed articles that addressed co-occurring medical conditions in adults with DS. Those conditions discussed in over half of the articles were prioritized for further review. Second, we performed detailed literature searches on these specific conditions.
This literature review relates changes in performance or safety outcome measures for older drivers to their medical conditions or medication use, and associated functional impairments. It was carried out as an initial task in the project, The Effects of Medical Conditions on Driving Performance. Researchers conducted a search of peer-reviewed ...
acute and chronic medical conditions, to reduce hospital readmissions, and to reduce barriers to health care (Biederman et al., 2016; Cornes et al., 2017; Dorney-Smith et al., 2016; Feigal et al., 2014; Klein & Reddy, 2015; ... Medical Respite Literature Review March 2021 www.nimrc.org 7 www.nhchc.org ...
Multimorbidity is defined as the presence of two or more chronic medical conditions in a person, whether physical, mental or long-term infectious diseases. This is especially common in older populations, affecting their quality of life and emotionally impacting their caregivers and family. Technology can allow for monitoring, managing, and motivating older adults in their self-care, as well as ...
Kavakiotis et al. conducted a systematic review regarding the machine learning applications, data mining techniques, and tools used in the diabetes field to showcase the prediction and diagnosis of diabetes, its complications, and genetic conditions and situation, including the physical condition care management. After the in-depth search, it ...
This study is based on systematic review approach or systematic literature review (SLR).This type of review enables a comprehensive understanding of a certain topic of interest or phenomenon, which provides details and important insights for policies and future studies [].SLR is also a structured approach to research synthesis, following a number of pre-determined steps to evaluate the state ...