
An official website of the United States government
Here’s how you know
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.

Food Safety and Inspection Service
- News & Events
- Food Safety
- Science & Data

Foodborne Illness and Disease
What is foodborne illness.
Foodborne illness is a preventable public health challenge that causes an estimated 48 million illnesses and 3,000 deaths each year in the United States. It is an illness that comes from eating contaminated food. The onset of symptoms may occur within minutes to weeks and often presents itself as flu-like symptoms, as the ill person may experience symptoms such as nausea, vomiting, diarrhea, or fever. Because the symptoms are often flu-like, many people may not recognize that the illness is caused by harmful bacteria or other pathogens in food.
Everyone is at risk for getting a foodborne illness. However, some people are at greater risk for experiencing a more serious illness or even death should they get a foodborne illness. Those at greater risk are infants, young children, pregnant women and their unborn babies, older adults, and people with weakened immune systems (such as those with HIV/AIDS, cancer, diabetes, kidney disease, and transplant patients.) Some people may become ill after ingesting only a few harmful bacteria; others may remain symptom free after ingesting thousands.
How Do Bacteria Get in Food?
Microorganisms may be present on food products when you purchase them. For example, plastic-wrapped boneless chicken breasts and ground meat were once part of live chickens or cattle. Raw meat, poultry, seafood, and eggs are not sterile. Neither is fresh produce such as lettuce, tomatoes, sprouts, and melons.
Thousands of types of bacteria are naturally present in our environment. Microorganisms that cause disease are called pathogens. When certain pathogens enter the food supply, they can cause foodborne illness. Not all bacteria cause disease in humans. For example, some bacteria are used beneficially in making cheese and yogurt.
Foods, including safely cooked and ready-to-eat foods, can become cross-contaminated with pathogens transferred from raw egg products and raw meat, poultry, and seafood products and their juices, other contaminated products, or from food handlers with poor personal hygiene. Most cases of foodborne illness can be prevented with proper cooking or processing of food to destroy pathogens.
Learn more about Pathogens
The Danger Zone
Bacteria multiply rapidly between 40 °F and 140 °F. To keep food out of this "Danger Zone," keep cold food cold and hot food hot .
- Store food in the refrigerator (40 °F or below) or freezer (0 °F or below).
- Cook all raw beef, pork, lamb and veal steaks, chops, and roasts to a minimum internal temperature of 145 °F as measured with a food thermometer before removing meat from the heat source. For safety and quality, allow meat to rest for at least three minutes before carving or consuming. For reasons of personal preference, consumers may choose to cook meat to higher temperatures.
- Cook all raw ground beef, pork, lamb, and veal to an internal temperature of 160 °F as measured with a food thermometer.
- Cook all poultry to a safe minimum internal temperature of 165 °F as measured with a food thermometer.
- Maintain hot cooked food at 140 °F or above.
- When reheating cooked food, reheat to 165 °F.
Learn more about food safety.
In Case of Foodborne Illness
Follow these general guidelines:
- Preserve the evidence. If a portion of the suspect food is available, wrap it securely, mark "DANGER" and freeze it. Save all the packaging materials, such as cans or cartons. Write down the food type, the date, other identifying marks on the package, the time consumed, and when the onset of symptoms occurred. Save any identical unopened products.
- Seek treatment as necessary. If the victim is in an "at risk" group, seek medical care immediately. Likewise, if symptoms persist or are severe (such as bloody diarrhea, excessive nausea and vomiting, or high temperature), call your doctor.
- Call the local health department if the suspect food was served at a large gathering, from a restaurant or other food service facility, or if it is a commercial product.
- Call the USDA Meat and Poultry Hotline at 1-888-MPHotline (1-888-674-6854) if the suspect food is a USDA-inspected product and you have all the packaging.
What Are Foodborne Pathogens?
There are different bacteria and pathogens that can cause foodborne illness.
Public Health Partners
Resources for sharing information or reporting foodborne illness.
Outbreaks: Response & Prevention
FSIS collaborates with CDC, FDA and APHIS for response and prevention efforts.
Foodborne Bacteria Table
Featured factsheets & resources.

Slow Cookers and Food Safety

Cleanliness Helps Prevent Foodborne Illness

Leftovers and Food Safety
Start your search, popular topics.
- Patient Care & Health Information
- Diseases & Conditions
- Food poisoning
Food poisoning, a type of foodborne illness, is a sickness people get from something they ate or drank. The causes are germs or other harmful things in the food or beverage.
Symptoms of food poisoning often include upset stomach, diarrhea and vomiting. Symptoms usually start within hours or several days of eating the food. Most people have mild illness and get better without treatment.
Sometimes food poisoning causes severe illness or complications.
Products & Services
- A Book: Mayo Clinic Book of Home Remedies
Symptoms vary depending on what is causing the illness. They may begin within a few hours or a few weeks depending on the cause.
Common symptoms are:
- Upset stomach.
- Diarrhea with bloody stools.
- Stomach pain and cramps.
Less often food poisoning affects the nervous system and can cause severe disease. Symptoms may include:
- Blurred or double vision.
- Loss of movement in limbs.
- Problems with swallowing.
- Tingling or numbness of skin.
- Changes in sound of the voice.
When to see a doctor
Infants and children.
Vomiting and diarrhea can quickly cause low levels of body fluids, also called dehydration, in infants and children. This can cause serious illness in infants.
Call your child's health care provider if your child's symptoms include vomiting and diarrhea and any of the following:
- Unusual changes in behavior or thinking.
- Excessive thirst.
- Little or no urination.
- Diarrhea that lasts more than a day.
- Vomiting often.
- Stools that have blood or pus.
- Stools that are black or tarry.
- Severe pain in the stomach or rectum.
- Any fever in children under 2 years of age.
- Fever of 102 degrees Fahrenheit (38.9 degrees Celsius) or higher in older children.
- History of other medical problems.
Adults should see a health care provider or get emergency care if the following occur:
- Nervous system symptoms, such as blurry vision, muscle weakness and tingling of skin.
- Changes in thinking or behavior.
- Fever of 103 degrees Fahrenheit (39.4 degrees Celsius).
- Diarrhea that lasts more than three days.
- Symptoms of dehydration — excessive thirst, dry mouth, little or no urination, severe weakness, dizziness, or lightheadedness.
There is a problem with information submitted for this request. Review/update the information highlighted below and resubmit the form.
From Mayo Clinic to your inbox
Sign up for free and stay up to date on research advancements, health tips, current health topics, and expertise on managing health. Click here for an email preview.
Error Email field is required
Error Include a valid email address
To provide you with the most relevant and helpful information, and understand which information is beneficial, we may combine your email and website usage information with other information we have about you. If you are a Mayo Clinic patient, this could include protected health information. If we combine this information with your protected health information, we will treat all of that information as protected health information and will only use or disclose that information as set forth in our notice of privacy practices. You may opt-out of email communications at any time by clicking on the unsubscribe link in the e-mail.
Thank you for subscribing!
You'll soon start receiving the latest Mayo Clinic health information you requested in your inbox.
Sorry something went wrong with your subscription
Please, try again in a couple of minutes
Many germs or harmful things, called contaminants, can cause foodborne illnesses. Food or drink that carries a contaminant is called "contaminated." Food can be contaminated with any of the following:
- Parasites that can live in the intestines.
- Poisons, also called toxins.
- Bacteria that carry or make toxins.
- Molds that make toxins.
Understanding terms
The term "food poisoning" is commonly used to describe all foodborne illnesses. A health care provider might use these terms to be more specific:
- "Foodborne illnesses" means all illnesses from any contaminated food or beverage.
- "Food poisoning" means illness specifically from a toxin in food. Food poisoning is a type of foodborne illness.
How food becomes contaminated
Food can be contaminated at any point from the farm or fishery to the table. The problem can begin during growing, harvesting or catching, processing, storing, shipping, or preparing.
Food can be contaminated any place it's handled, including the home, because of:
- Poor handwashing. Feces that remains on the hands after using the toilet can contaminate food. Other contaminants can be transferred from hands during food preparation or food serving.
- Not disinfecting cooking or eating areas. Unwashed knives, cutting boards or other kitchen tools can spread contaminants.
- Improper storage. Food left out for too long at room temperature can become contaminated. Food stored in the refrigerator for too long can spoil. Also, food stored in a refrigerator or freezer that is too warm can spoil.
Common causes
The following table shows common causes of foodborne illnesses, the time from exposure to the beginning of symptoms and common sources of contamination.
Other sources
Bacteria that cause foodborne illnesses can also be found in swimming pools, lakes, ponds, rivers and seawater. Also, some bacteria, such as E. coli, may be spread by exposure to animals carrying the disease.
Risk factors
Anyone can get food poisoning. Some people are more likely to get sick or have more-serious disease or complications. These people include:
- Infants and children.
- Pregnant people.
- Older adults.
- People with weakened immune systems due to another disease or treatments.
Complications
In most healthy adults, complications are uncommon. They can include the following.
Dehydration
The most common complication is dehydration. This a severe loss of water and salts and minerals. Both vomiting and diarrhea can cause dehydration.
Most healthy adults can drink enough fluids to prevent dehydration. Children, older adults, and people with weakened immune systems or other illnesses may not be able to replace the fluids they've lost. They are more likely to become dehydrated.
People who become dehydrated may need to get fluids directly into the bloodstream at the hospital. Severe dehydration can cause organ damage, other severe disease and death if not treated.
Complications of systemic disease
Some contaminants can cause more widespread disease in the body, also called systemic disease or infection. This is more common in people who are older, have weakened immune systems or other medical conditions. Systemic infections from foodborne bacteria may cause:
- Blood clots in the kidneys. E. coli can result in blood clots that block the kidneys' filtering system. This condition, called hemolytic uremic syndrome, results in the sudden failure of the kidneys to filter waste from the blood. Less often, other bacteria or viruses may cause this condition.
- Bacteria in the bloodstream. Bacteria in the blood can cause disease in the blood itself or spread disease to other parts of the body.
- Meningitis. Meningitis is inflammation that may damage the membranes and fluid surrounding the brain and spinal cord.
- Sepsis. Sepsis is an overreaction of the immune system to systemic disease that damages the body's own tissues.
Pregnancy complications
Illness from the listeria bacteria during pregnancy can result in:
- Miscarriage or stillbirth.
- Sepsis in the newborn.
- Meningitis in the newborn.
Rare complications
Rare complications include conditions that may develop after food poisoning, including:
- Arthritis. Arthritis is swelling, tenderness or pain in joints.
- Irritable bowel syndrome. Irritable bowel syndrome is a lifelong condition of the intestines that causes pain, cramping and irregular bowel movements.
- Guillain-Barre syndrome. Guillain-Barre syndrome is an immune system attack on nerves that can result in tingling, numbness and loss of muscle control.
- Breathing difficulties. Rarely, botulism can damage nerves that control the muscles involved in breathing.
To prevent food poisoning at home:
- Handwashing. Wash your hands with soap and water for at least 20 seconds. Do this after using the toilet, before eating, and before and after handling food.
- Wash fruits and vegetables. Rinse fruits and vegetables under running water before eating, peeling or preparing.
- Wash kitchen utensils thoroughly. Wash cutting boards, knives and other utensils with soapy water after contact with raw meats or unwashed fruits and vegetables.
- Don't eat raw or undercooked meat or fish. Use a meat thermometer to make sure meat is cooked enough. Cook whole meats and fish to at least 145 F (63 C) and let rest for at least three minutes. Cook ground meat to at least 160 F (71 C). Cook whole and ground poultry to at least 165 F (74 C).
- Refrigerate or freeze leftovers. Put leftovers in covered containers in the refrigerator right after your meal. Leftovers can be kept for 3 to 4 days in the refrigerator. If you don't think you'll eat them within four days, freeze them right away.
- Cook leftovers safely. You can safely thaw frozen food three ways. You can microwave it. You can move it to the refrigerator to thaw overnight. Or you can put the frozen food in a leakproof container and put it in cold water on the counter. Reheat leftovers until the internal temperature reaches 165 degrees Fahrenheit (74 degrees Celsius).
- Throw it out when in doubt. If you aren't sure if a food has been prepared, served or stored safely, discard it. Even if it looks and smells fine, it may not be safe to eat.
- Throw out moldy food. Throw out any baked foods with mold. Throw out moldy soft fruits and vegetables, such as tomatoes, berries or peaches. And throw away any nuts or nut products with mold. You can trim away mold from firm foods with low moisture, such as carrots, bell peppers and hard cheeses. Cut away at least 1 inch (2.5 centimeters) around the moldy part of the food.
- Clean your refrigerator. Clean the inside of the refrigerator every few months. Make a cleaning solution of 1 tablespoon (15 milliliters) of baking soda and 1 quart (0.9 liters) of water. Clean visible mold in the refrigerator or on the door seals. Use a solution of 1 tablespoon (15 milliliters) of bleach in 1 quart (0.9 liters) of water.
Safety for at-risk people
Food poisoning is especially serious during pregnancies and for young children, older adults and people with weakened immune systems. These illnesses may be life-threatening. These individuals should avoid the following foods:
- Raw or undercooked meat, poultry, fish, and shellfish.
- Raw or undercooked eggs or foods that may contain them, such as cookie dough and homemade ice cream.
- Raw sprouts, such as alfalfa, bean, clover and radish sprouts.
- Unpasteurized juices and ciders.
- Unpasteurized milk and milk products.
- Soft cheeses, such as feta, brie and Camembert; blue-veined cheese; and unpasteurized cheese.
- Refrigerated pates and meat spreads.
- Uncooked hot dogs, luncheon meats and deli meats.
- Foodborne germs and illnesses. U.S. Centers for Disease Control and Prevention. https://www.cdc.gov/foodsafety/foodborne-germs.html. Accessed Nov. 7, 2022.
- Definition & facts of food poisoning. National Institute of Diabetes and Digestive and Kidney Diseases. https://www.niddk.nih.gov/health-information/digestive-diseases/food-poisoning/definition-facts. Accessed Nov. 7, 2022.
- Symptoms & causes of food poisoning. National Institute of Diabetes and Digestive and Kidney Diseases. https://www.niddk.nih.gov/health-information/digestive-diseases/food-poisoning/symptoms-causes. Accessed Nov. 7, 2022.
- LaRocque R. Causes of acute infectious diarrhea and other foodborne illnesses in resource-rich settings. https://www.uptodate.com/contents/search. Accessed Nov. 7, 2022.
- Bennett JE, et al. Mandell, Douglas, and Bennett's Principles and Practice of Infectious Diseases. 9th ed. Elsevier; 2020. https://www.clinicalkey.com. Accessed Nov. 7, 2022.
- Schmitt BD. Pediatric Telephone Protocols: Office Version. 17th ed. American Academy of Pediatrics; 2021.
- Fever. American College of Emergency Physicians. https://www.emergencyphysicians.org/article/know-when-to-go/fever. Accessed Nov. 30, 2022.
- Bacteria and viruses. FoodSafety.gov. U.S. Department of Health and Human Services. https://www.foodsafety.gov/food-poisoning/bacteria-and-viruses. Accessed Nov. 16, 2022.
- Kellerman RD, et al. Foodborne illnesses. In: Conn's Current Therapy 2022. Elsevier; 2022. https://www.clinicalkey.com. Accessed Nov. 13, 2022.
- Goldman L, et al., eds. Giardiasis. Goldman-Cecil Medicine. 26th ed. Elsevier; 2020. https://www.clinicalkey.com. Accessed Nov. 13, 2022.
- Diagnosis of food poisoning. National Institute of Diabetes and Digestive and Kidney Diseases. https://www.niddk.nih.gov/health-information/digestive-diseases/food-poisoning/diagnosis. Accessed Nov. 7, 2022.
- LaRocque R. Approach to the adult with acute diarrhea in resource-rich settings. https://www.uptodate.com/contents/search. Accessed Nov. 7, 2022.
- Treatment for food poisoning. National Institute of Diabetes and Digestive and Kidney Diseases. https://www.niddk.nih.gov/health-information/digestive-diseases/food-poisoning/treatment. Accessed Nov. 7, 2022.
- Eating, diet and nutrition for food poisoning. National Institute of Diabetes and Digestive and Kidney Diseases. https://www.niddk.nih.gov/health-information/digestive-diseases/food-poisoning/eating-diet-nutrition. Accessed Nov. 20, 2022.
- Four steps to food safety: Clean, separate, cook, chill. U.S. Centers for Disease Control and Prevention. https://www.cdc.gov/foodsafety/keep-food-safe.html. Accessed Nov. 7, 2022.
- Leftovers and food safety. U.S. Department of Agriculture. https://www.fsis.usda.gov/food-safety/safe-food-handling-and-preparation/food-safety-basics/leftovers-and-food-safety. Accessed Nov. 20, 2022.
- Foods that can cause food poisoning. U.S. Centers for Disease Control and Prevention. https://www.cdc.gov/foodsafety/foods-linked-illness.html. Accessed Nov. 20, 2022.
- Molds on food: Are they dangerous? Food Safety and Inspection Service. U.S. Department of Agriculture. https://www.fsis.usda.gov/food-safety/safe-food-handling-and-preparation/food-safety-basics/molds-food-are-they-dangerous Accessed Dec. 1, 2022.
News from Mayo Clinic
- Mayo Clinic Minute: Tips for safer picnics May 26, 2023, 03:00 p.m. CDT
- Mayo Clinic Minute: Does one moldy berry spoil the whole bunch? March 09, 2023, 03:30 p.m. CDT
- Mayo Clinic Minute: Food recalls and sickness July 11, 2022, 04:00 p.m. CDT
- Symptoms & causes
- Diagnosis & treatment
Mayo Clinic does not endorse companies or products. Advertising revenue supports our not-for-profit mission.
- Opportunities
Mayo Clinic Press
Check out these best-sellers and special offers on books and newsletters from Mayo Clinic Press .
- Mayo Clinic on Incontinence - Mayo Clinic Press Mayo Clinic on Incontinence
- The Essential Diabetes Book - Mayo Clinic Press The Essential Diabetes Book
- Mayo Clinic on Hearing and Balance - Mayo Clinic Press Mayo Clinic on Hearing and Balance
- FREE Mayo Clinic Diet Assessment - Mayo Clinic Press FREE Mayo Clinic Diet Assessment
- Mayo Clinic Health Letter - FREE book - Mayo Clinic Press Mayo Clinic Health Letter - FREE book
Your gift holds great power – donate today!
Make your tax-deductible gift and be a part of the cutting-edge research and care that's changing medicine.
- Skip to main content
- Skip to FDA Search
- Skip to in this section menu
- Skip to footer links

The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you're on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
U.S. Food and Drug Administration
- Search
- Menu
- Recalls, Outbreaks & Emergencies
- Outbreaks of Foodborne Illness
Investigations of Foodborne Illness Outbreaks

Note: Not all recalls and alerts result in an outbreak of foodborne illness . Check recent Food Recalls and Safety Alerts .
The following is a list of outbreak and adverse event investigations primarily being managed by FDA’s CORE Response Teams . The investigations are in a variety of stages, meaning that some have limited information, while others may be near completion. If you think you have symptoms of foodborne illness, talk to your healthcare provider and public health officials to provide them with details of what you ate before becoming sick. This often aids in helping solve emerging or ongoing outbreaks.
A public health advisory will be issued for investigations that have resulted in specific, actionable steps for consumers to take to protect themselves. Please direct your attention to those pages for the most up to date information on the investigation and for consumer protection information.
Outbreak and adverse event investigations that do not result in specific, actionable steps for consumers may or may not conclusively identify a source or reveal any contributing factors. Adverse event investigations rely on self-reported data. Although these reports may name a particular product, FDA will only indicate a product category in the table and will not publicly name a specific product until there is sufficient evidence to implicate that product as a cause of illnesses or adverse events. If a cause and/or contributing factors are identified that could inform future prevention, FDA commits to providing a summary of those findings.
- There are no updates for this week’s table.
Active Investigations
Closed investigations, 2024 investigations, 2023 investigations, 2022 investigations, 2021 investigations.
1 This cluster represents a subset of the total number of domestically-acquired cases of cyclosporiasis cases in the U.S.
2 Based on CDC’s epidemiological investigation of two large multistate outbreaks of cyclosporiasis , ill people reported eating a variety of leafy greens before becoming sick. For both investigations, CDC, FDA, and state and local partners conducted epidemiologic and traceback investigations and collected and analyzed product and environmental samples. All samples collected were reported as negative for Cyclospora . Due to the lack of additional detail in the epidemiological data and the absence of supporting evidence collected from traceback and sample collection, FDA could not identify a specific product as the source of either outbreak.
2020 Investigations
Related links.
CDC Investigations
FSIS Investigations
Table Definitions
Date Posted : Date the investigation is posted to the table. This happens once CORE begins to actively coordinate an investigation. In collaboration with federal and state partners, CORE initiates response activities to control the outbreak or adverse events.
Reference Number : This number is assigned to incidents that CORE is working on. Each foodborne illness investigation on the table will have a unique reference number and this is provided to help users of this table differentiate between investigations. Those reference numbers beginning with an “E” have carried over from an older numbering system that will not be used by CORE in the future.
Pathogen or Cause of Illness : A bacterium, virus, other microorganism, toxin, or other contaminant that can cause disease.
Product(s) Linked to Illnesses (if any) : During an outbreak or adverse event investigation, the FDA and CDC, along with state and local authorities collect and analyze three types of information: epidemiological information, laboratory analyses of food and/or samples taken from food production environments, and traceback investigation findings. Each outbreak or adverse event is unique and the information available to investigators varies from outbreak to outbreak – however, through rigorous analysis of the information collected, investigators are often able to identify a likely or confirmed food source of an outbreak or adverse events. Additionally, adverse event investigations rely on self-reported data, which may not include all necessary information to fully investigate the product or event. It is important to note that before a specific food is linked to an outbreak or adverse events, the investigation of a commodity or a specific food by the FDA, CDC and state and local partners does not mean that the food is the cause of an outbreak or adverse events. In many cases the investigation is also looking to rule out specific foods even as it identifies the particular suspect. If there is evidence that a specific food is linked to illnesses, it will be reflected here and health authorities will warn the public about that food.
Total Case Count : Updated weekly. For outbreak investigations, the case count is provided to the FDA by the CDC. Case counts are dynamic and the exact number of illnesses constantly changes during an investigation. This number is provided in order to provide an estimate of the size of an outbreak each week. In the case of adverse event investigations, FDA will provide the number of adverse events that have been self-reported by consumers to FDA consumer complaint coordinators and the CFSAN Adverse Event Reporting System (CAERS), which could include duplicate reports. More formalized data will be published in CDC Investigation Notices or in FDA and CDC advisories, should they be posted.
Investigation Status : Communicates whether this outbreak is still under investigation by CORE or the investigational activities have ended. Options for this column would be either “Active” or “Closed”. At times an FDA investigation may be active after an outbreak has ended.
Outbreak/Event Status : Communicates whether this outbreak or series of adverse event reports is ongoing or has ended.
Recall Initiated : A recall occurs when a firm takes a product off the market because there is reason to believe that it may cause consumers to become ill. In some situations, FDA may request the company recall a potentially contaminated food. In other situations, FDA may issue a mandatory recall if there is a reasonable probability that the food is adulterated under certain FDA authorities, and that the food could cause serious illnesses or death.
FDA Traceback Initiated : Used to identify the source and distribution of the implicated food and remove the contaminated product from the marketplace, to distinguish between two or more implicated food products, and to determine potential routes and/or sources of contamination in order to help prevent future illnesses. For additional information, see How the FDA Uses Traceback to Respond to Foodborne Illness Outbreaks .
FDA Inspection Initiated : An official examination by FDA of the operational processes of a facility to determine its compliance with federal law, which may include, among other things, record and sample collection. Activities reported on the table are limited to those conducted by FDA; however, state and local partners work in coordination with FDA and may also conduct inspectional activities. Additional information on the different types of inspections conducted by FDA can be found on the FDA website .
FDA Sampling Initiated : Collection of samples for the presence or absence of a pathogen in a food or in the environment surrounding the food. Samples reported on the table include those collected by the FDA or state collected samples that are analyzed by the FDA. Significant sample findings are reviewed by FDA and are reported in Public Health Advisories .
Who to Contact if you Have Symptoms of Foodborne Illness
Consumers who have symptoms of foodborne illness should contact their health care provider to report their symptoms and receive care.
To report a complaint or adverse event (illness or serious allergic reaction), you have three choices:
- Call an FDA Consumer Complaint Coordinator if you wish to speak directly to a person about your problem.
- Complete an electronic Voluntary MedWatch form online.
- Complete a paper Voluntary MedWatch form that can be mailed to FDA.
Visit www.fda.gov/fcic for additional consumer and industry assistance.
Get email updates delivered to your inbox.
Get regular FDA email updates delivered on this topic to your inbox.
- Here’s how you know
U.S. DEPARTMENT OF AGRICULTURE
Have a Question? AskUSDA
We’re here to help you find what you’re looking for.
What causes most foodborne illnesses?
Dec 15, 2023 • knowledge, information, related information, related articles.
- Does mayonnaise cause foodborne illness?
- What is the difference between foodborne illness and food poisoning?
- What is the difference between food poisoning and foodborne illness?
- How many foodborne illnesses occur each year?
- What is foodborne illness?
Trending Articles
- How long can you keep hard cooked eggs?
- What are cooking times for chicken?
- How long can meat and poultry remain in the refrigerator, once thawed?
- How long can you store eggs in the refrigerator?
- To what temperature should I cook pork?
Accessibility Statement
Non-Discrimination Statement
Information Quality
Privacy Policy
New Farmers
Disaster Resource Center

May 18, 2024
What Is Pasteurization, and How Does It Keep Milk Safe?
The pasteurization process was invented in the 1860s and continues to keep people safe from a range of foodborne illnesses
By Kerry E. Kaylegian & The Conversation US

Jacobs Stock Photography Ltd/Getty Images
Recent reports that the H5N1 avian flu virus has been found in cow’s milk have raised questions about whether the U.S. milk supply is safe to drink. According to the federal Food and Drug Administration, the answer is yes, as long as the milk is pasteurized .
Nonetheless, raw (unpasteurized) milk sales are up , despite health experts’ warning that raw milk could contain high levels of the virus , along with many other pathogens.

On supporting science journalism
If you're enjoying this article, consider supporting our award-winning journalism by subscribing . By purchasing a subscription you are helping to ensure the future of impactful stories about the discoveries and ideas shaping our world today.
As an extension food scientist in a state where raw milk sales are legal , I provide technical support to help processors produce high-quality, safe dairy foods. I also like to help people understand the confusing world of pasteurization methods on their milk labels, and why experts strongly discourage consuming raw milk and products made from it.
What can make milk unsafe
Dairy products, like many foods, have inherent risks that can cause a variety of illnesses and even death. Our milk comes from animals that graze outdoors and live in barns. Milk is picked up from the farm in tanker trucks and delivered to the processing plant. These environments offer numerous opportunities for contamination by pathogens that cause illness and organisms that make food spoil.
For example, listeria monocytogenes comes from environmental sources like soil and water. Mild infections with listeriosis cause flu-like symptoms. More serious cases are, unfortunately, too common and can cause miscarriages in pregnant women and even death in extreme cases .
Other pathogens commonly associated with dairy animals and raw milk include E. coli , which can cause severe gastrointestinal infections and may lead to kidney damage; Campylobacter , the most common cause of diarrheal illness in the U.S.; and Salmonella , which cause abdominal pain, diarrhea and other symptoms.
Keeping beverages safe with heat
In the 1860s, French microbiologist Louis Pasteur discovered that heating wine and beer killed the organisms that caused spoilage, which then was a significant problem in France.
This heating process, which became known as pasteurization, was adopted in the U.S. prior to World War II, at a time when milk was responsible for 25% of all U.S. outbreaks of foodborne illnesses . In 1973, the federal government required that all milk sold across state lines in the U.S. had to be pasteurized, and in 1987, it banned interstate sales of raw milk .
Pasteurization heats every particle of a food to a specific temperature for a continuous length of time in order to kill the most heat-resistant pathogen associated with that product. Different organisms have different responses to heat, so controlled scientific studies are required to determine what length of time at a given temperature will kill a specific organism.
Since 1924, pasteurization in the U.S. has been guided by the Grade “A” Pasteurized Milk Ordinance , a federal guidance document that is updated every two years to reflect current science and has been adopted by all 50 states . Pasteurization equipment in the U.S. must meet stringent requirements that include sanitary design, safety controls and material standards.
Pasteurization methods
Dairy processors can choose among several different types of pasteurization. When executed properly, all of these methods produce the same result: pathogen-free milk. Processors may treat milk beyond minimum times or temperatures to provide an extra margin of safety, or to reduce bacteria that can cause milk to spoil, thus increasing the product’s shelf life.
Vat pasteurizers , also known as batch pasteurizers, often are used by smaller-scale processors who handle limited volumes. The milk is pumped into a temperature-controlled tank with a stirrer, heated to a minimum of 145 degrees Fahrenheit (63 Celsius) and held there continuously for 30 minutes. Then it is cooled and pumped out of the vat.
The most common method used for commercial milk is high-temperature short-time pasteurization , which can treat large volumes of milk. The milk is pumped through a series of thin plates at high speed to reach a minimum temperature of 161 F (71 C). Then it travels through a holding tube for 15 seconds, and the temperature is checked automatically for safety and cooled.
The most complex and expensive systems are ultra-pasteurizers and ultra-high-temperature pasteurizers , which pasteurize milk in just a few seconds at temperatures above 285 F (140 C). This approach destroys many spoilage organisms, giving the milk a significantly longer shelf life than with other methods, although sometimes products made this way have more of a “cooked” flavor.
Ultra-high-temperature products are processed in a sterile environment and packaged in sterile packaging, such as lined cartons and pouches. They can be shelf-stable for up to a year before they are opened. Ultra-high-temperature packaging makes taking milk to school for lunch safe for kids every day.
Avian flu in milk
The detection of avian flu virus fragments in milk is a new challenge for the dairy industry. Scientists do not have a full picture of the risks to humans but are learning.
Research so far has shown that virus particles end up in the milk of infected cows, but that pasteurization will inactivate the virus . However, the FDA is advising consumers not to drink raw milk because there is limited information about whether it may transmit avian flu .
The agency also is urging producers not to manufacture or sell raw milk or raw milk products, including cheese, made with milk from cows showing symptoms of illness.
It’s never a good time to get a foodborne illness, and this is the beginning of ice cream season . At a time when avian flu is showing up in new species and scientists are still learning about how it is transmitted, I agree with the FDA that raw milk poses risks not worth taking.
This article was originally published on The Conversation . Read the original article .
- Open access
- Published: 17 May 2024
Antibiotic susceptibility patterns and trends of the gram-negative bacteria isolated from the patients in the emergency departments in China: results of SMART 2016–2019
- Ying Fu 1 , 2 ,
- Feng Zhao 1 , 2 ,
- Jie Lin 1 , 2 ,
- Pengcheng Li 3 &
- Yunsong Yu 4 , 5 , 6
BMC Infectious Diseases volume 24 , Article number: 501 ( 2024 ) Cite this article
88 Accesses
8 Altmetric
Metrics details
The study aims were to evaluate the species distribution and antimicrobial resistance profile of Gram-negative pathogens isolated from specimens of intra-abdominal infections (IAI), urinary tract infections (UTI), respiratory tract infections (RTI), and blood stream infections (BSI) in emergency departments (EDs) in China.
From 2016 to 2019, 656 isolates were collected from 18 hospitals across China. Minimum inhibitory concentrations were determined by CLSI broth microdilution and interpreted according to CLSI M100 (2021) guidelines. In addition, organ-specific weighted incidence antibiograms (OSWIAs) were constructed.
Escherichia coli ( E. coli ) and Klebsiella pneumoniae ( K. pneumoniae ) were the most common pathogens isolated from BSI, IAI and UTI, accounting for 80% of the Gram-negative clinical isolates, while Pseudomonas aeruginosa ( P. aeruginosa ) was mainly isolated from RTI. E. coli showed < 10% resistance rates to amikacin, colistin, ertapenem, imipenem, meropenem and piperacillin/tazobactam. K. pneumoniae exhibited low resistance rates only to colistin (6.4%) and amikacin (17.5%) with resistance rates of 25–29% to carbapenems. P. aeruginosa exhibited low resistance rates only to amikacin (13.4%), colistin (11.6%), and tobramycin (10.8%) with over 30% resistance to all traditional antipseudomonal antimicrobials including ceftazidime, cefepime, carbapenems and levofloxacin. OSWIAs were different at different infection sites. Among them, the susceptibility of RTI to conventional antibiotics was lower than for IAI, UTI or BSI.
Conclusions
Gram-negative bacteria collected from Chinese EDs exhibited high resistance to commonly used antibiotics. Susceptibilities were organ specific for different infection sites, knowledge which will be useful for guiding empirical therapies in the clinic.
Peer Review reports
Antimicrobials are frequently used in emergency departments (EDs) in China and a study noted that the proportion of emergency patients treated with antibiotics was as high as 39.31 to 43.45% from 2016 to 2019 [ 1 ]. Antibiotic stewardship in EDs should avoid administration of broad-spectrum antibiotics, shorten their use times, as well as minimizing their unnecessary use [ 2 ]. However, as patients presenting to EDs are often in an acute state, physicians have to make decisions in a very short time frame and they prescribe antibiotics empirically. For critically ill infected patients, guidelines recommend to start antibiotic treatment in the first hour of recognition [ 3 ], which means that it is frequently impossible to get microbiology results to guide the choice of antimicrobial therapy. In order to support the choice of empiric antibiotic treatments, consensus guidelines as well as local antibiotic drug susceptibility detection and various antimicrobial surveillance programs have been introduced in China [ 4 , 5 ].
One approach to individualized empiric antibiotic therapy is the Weighted-Incidence Syndromic Combination Antibiogram, which is comprised of information about the likelihood a treatment regimen will be effective for all relevant organisms for a given infection based on existing large datasets [ 6 , 7 , 8 ]. A similar approach is the organ-specific weighted incidence antibiogram (OSWIA), which estimates probable susceptibilities of organ specific isolates to specific antibiotics [ 9 ]. The Study for Monitoring Antimicrobial Resistance Trends (SMART) global surveillance program monitors in vitro susceptibilities of clinical Gram-negative bacilli to antimicrobial agents obtained from blood stream infections (BSI), intra-abdominal infections (IAI), urinary tract infections (UTI) and respiratory tract infections (RTI). The purpose of the present study was to determine the prevalence and susceptibilities of various bacteria to conventional antibiotics in patients attending Chinese EDs through a retrospective analysis of the SMART data collected from 2016 to 2019 and to determine differences of organ distributions between the infecting bacterial strains.
In this study, the patient informed consent was waived and authorized by the Ethics Committee of Sir Run Run Shaw Hospital, Zhejiang University School of Medicine (Approval Number: 20210811-33).
All bacterial isolates were collected from discarded clinical specimens of hospitalized patients with BSI, IAI, UTI and RTI between 2016 and 2019 who were admitted to the EDs of 18 hospitals across China (Supplementary Table 1 ). The IAI specimen is derived from tissues or organs within the abdominal cavity, including the stomach, intestines, liver, spleen, pancreas, kidneys that have been infected by pathogens, resulting in infectious diseases [ 10 ]. RTI refers to an infection of the tissues in the respiratory system by pathogens such as viruses, bacteria, or fungi. RTI specimens from the respiratory tract included nasal and throat swabs, sputum samples, bronchoalveolar lavage fluid, respiratory secretions, and others [ 11 ]. Identification of isolates was initially made by each hospital laboratory and then the specimens were sent for laboratory re-identification using MALDI-TOF/MS (Bruker Daltonics, USA). Any duplicate isolates collected from the same patient were excluded from the data analysis.
Antimicrobial susceptibility testing
Testing was carried out in the Peking Union Medical College Hospital clinical microbiology laboratory using the Trek Diagnostic System (Thermo Fisher Scientific). Clinical isolates and reference strains were detected using the microbroth dilution method. Minimum inhibitory concentrations (MICs) were determined with reference to the antimicrobial breakpoint of the CLSI M100 (2021) [ 12 ]. The antibiotics tested were amikacin (AMK), cefepime (FEP), ceftazidime (CAZ), aztreonam (ATM), ceftriaxone (CRO), colistin (COL), ertapenem (ETP), levofloxacin (LVX), cefoxitin (FOX), imipenem (IPM), tobramycin (TOB), meropenem (MEM) and piperacillin–tazobactam (TZP).
Definition of antimicrobial-resistant strains
Carbapenem resistance of Escherichia coli ( E. coli ) and Klebsiella pneumoniae ( K. pneumoniae ) refers to resistance to any of IPM, MEM or ETP. Carbapenem-resistant Pseudomonas aeruginosa ( P. aeruginosa ) was defined as resistance to IPM or MEM.
Quinolone resistance to E. coli, K. pneumoniae and P. aeruginosa was defined as resistance to LVX.
Third generation cephalosporin resistance to E. coli and K. pneumoniae was defined as resistance to any CRO or CAZ, and the strains susceptible or intermediate to carbapenems (IPM, MEM or ETP). P. aeruginosa resistant to third-generation cephalosporin was defined as resistance to CAZ (CAZ-resistant PA) and the strains susceptible or intermediate to carbapenems (IPM, MEM).
OSWIA calculation
Data were retrospectively analyzed to establish the distribution of bacteria in various organs for BSI, IAI, UTI and RTI. OSWIA values were determined as previously described [ 9 ].
Patient characteristics and specimen source
Between January 01, 2016 and December 31, 2019, a total of 656 isolated were obtained from ED patients. The patient characteristics are detailed in Table 1 . The patients average age was 60.6 years (range: 1–101), comprising 388 males and 268 females. Most infections were hospital-acquired (HA) (58.1%), while 249 (38.0%) were community-acquired (CA) and for 26 data were not applicable. The isolates included 210 strains from IAI collected during surgery from the peritoneal fluid, appendix, abscesses, pancreas, gall bladder, liver and stomach. A total of 122 strains from BSI, 112 strains from UTI mainly from the urine, and 208 strains from RTI taken from bronchoalveolar lavage, endotracheal aspirate, thoracentesis or sputum were identified, as well as 4 strains from unconfirmed organs.
Distribution of Gram-negative bacteria obtained from BSI, IAI, UTI and RTI
Enterobacterales were the most common Gram-negative bacilli isolated from emergency patients with BSI, IAI and UTI (Fig. 1 ). E. coli accounted for 48.4% in BSI, 58.6% in IAI and 72.3% in UTI, while K. pneumoniae accounted for 24.6%, 21.4% and 11.6%, respectively and other Enterobacterales were much less common than E. coli and K. pneumoniae . The pathogen distribution in RTI was distinctly different from the other three infection types, with P. aeruginosa and K. pneumoniae being the most common species each accounting for about 40% of the Gram-negative pathogens. Since the composition ratio of Gram-negative bacteria was different at different infection sites (Fig. 1 , Supplementary Table 2 ) the varying patterns between infected organs should be considered when prescribing empirical treatments.
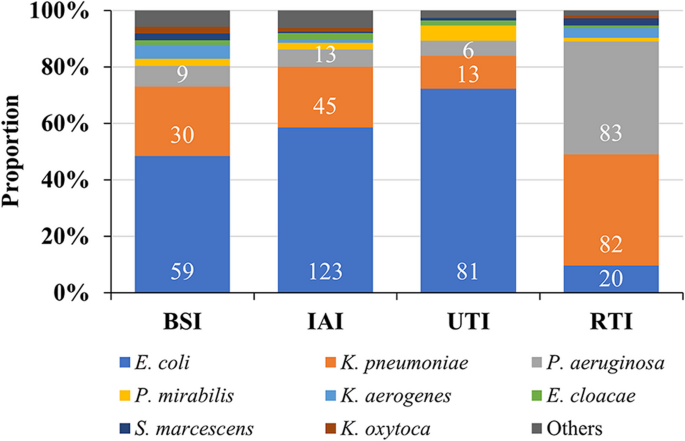
Distribution of Gram-negative bacilli in BSI, IAI, UTI and RTI. Abbreviations: BSI, blood steam infection; IAI, intra-abdominal infection; UTI, urinary tract infection
Distribution of Gram-negative bacteria from 2016 to 2019
The distribution of Gram-negative pathogens was stable between 2016 and 2019, with E. coli , K. pneumoniae and P. aeruginosa being the top 3 species, accounting for more than 80% of the clinical isolates (Fig. 2 , Supplementary Table 3 ).
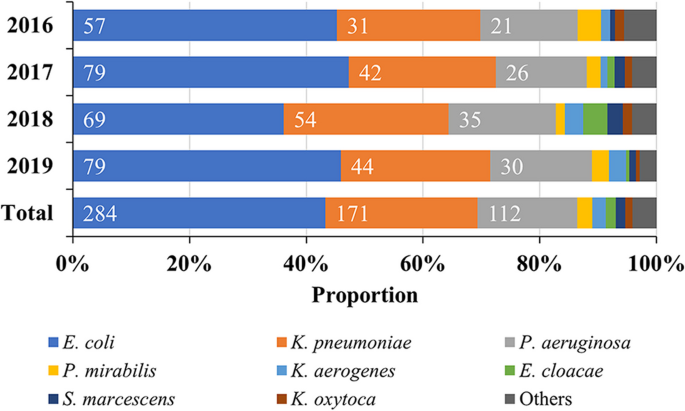
Composition ratio of Gram-negative bacteria in EDs from 2016 to 2019. Abbreviation: ED, emergency department.
Distribution of Gram-negative bacteria in different age groups of patients
Among the strains collected, regardless of the organ of origin, the predominant species were P. aeruginosa, E. coli and K. pneumoniae . However, the composition ratio of the main bacterial groups were different in infection sites within age groups (Fig. 3 a-d) and were generally different especially in the age group ≤ 39 years (Fig. 3 e, Supplementary Table 4 ).
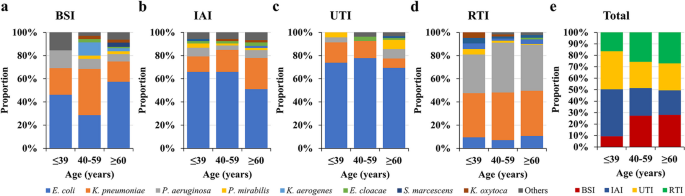
Comparison of the composition ratio of microbiota in different infected organs and age groups. Abbreviations: BSI, blood steam infection; IAI, intra-abdominal infection; RTI, respiratory tract infection; UTI, urinary tract infection.
Monitoring of drug susceptibility
Drug resistance rate monitoring of major gram-negative bacteria from 2016 to 2019.
E. coli exhibited < 10% resistance to AMK, COL, ETP, IPM, MEM and TZP, with the exception in 2016 to TZP, but generally TZP resistance rates were reduced between 2016 and 2019. Otherwise, resistance rates were more than 30%, with the exception of FOX (16.2%). K. pneumoniae exhibited < 20% resistance only to AMK and 6.4% to COL between 2016 and 2019. P. aeruginosa only exhibited low resistant rates of 13.4% to AMK, 11.6% to COL and 10.8% to TOB from 2016 to 2019 (Table 2 ).
Detection rate and drug susceptibility of specific antibiotic-resistant bacteria from 2016 to 2019
Isolation of carbapenem-resistant, quinolone-resistant or third-generation cephalosporin-resistant e. coli, k. pneumoniae and p. aeruginosa.
In isolates, the carbapenem-resistant E. coli and P. aeruginosa showed an overall downward trend. However, the rate of detection of carbapenem-resistant E. coli was relatively low, being only 1.3% in 2019, while for carbapenem-resistant P. aeruginosa in 2019 it was 30.0% and for carbapenem-resistant K. pneumoniae strains in 2019, 34.1%, the rate being higher than in 2018 (18.5%). The rate of detection of quinolone-resistant E. coli or K. pneumoniae showed a decreasing trend in the four years studied, being 55.7% in 2019 for the detection of quinolone-resistant E. coli and 36.4% for K. pneumoniae . The detection rate of quinolone-resistant P. aeruginosa was 26.7% in 2019 and lower than in 2018 (42.9%). The detection rates of third-generation cephalosporin-resistant E. coli and K. pneumoniae as well as P. aeruginosa showed an irregular trend from 2016 to 2019, being between 44.3%–63.2% and 9.1%–24.1% as well as 2.9%–15.4%, respectively throughout the years. Compared to E. coli, there were only few numbers of third-generation cephalosporin-resistant K. pneumoniae and P. aeruginosa isolates found between 2016 and 2019 (Fig. 4 , Supplementary Table 5 ).
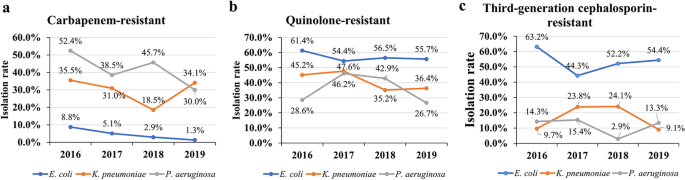
Isolation (detection) rate of carbapenem-resistant, quinolone-resistant, third-generation cephalosporin-resistant E. coli , K. pneumoniae and P. aeruginosa from 2016 to 2019
Specific drug resistance rates (%) of strains to antibiotics from 2016 to 2019
For E. coli , the resistance rate of carbapenem-resistant E. coli to AMK was 33.3%, and to the other antibiotics tested were > 60%, apart from COL (25.0%). Quinolone-resistant E. coli exhibited the lowest resistance rates to AMK (4.3%), ETP (5.6%), IPM (5.0%) and MEM (5.6%). The resistance rates of third-generation cephalosporin-resistant E. coli was 2.0% to AMK and 0% to ETP, IPM and MEM.
Carbapenem-resistant K. pneumoniae were 57.1% resistant to AMK and quinolone-resistant K. pneumoniae were 42.0% resistant to AMK, with low resistance rates only found to COL (8.2% and 10.1%), respectively. Third-generation cephalosporin-resistant K. pneumoniae was 6.7% resistant to AMK and 0% to ETP, IPM and MEM.
For carbapenem-resistant P. aeruginosa , the drug resistance to AMK was 30.4%, for TOB 28.0% and for COL (10.9%). For quinolone-resistant P. aeruginosa, only resistance rates to AMK (24.4%) and TOB (26.1%) as well as COL (9.8%) remained low. Third-generation cephalosporins resistant P. aeruginosa, showed low resistance rates of 0% to AMK, IPM, MEM and TOB (Table 3 ).
Antimicrobial susceptibility monitoring during empiric treatment of different infection sites and organs
In the weighted susceptibility assessment of different infection sites, it was found that the susceptibility of the same antibacterial drug at different organs and infection sites was different. For example, AMK, TOB, ETP, IPM and MEM were the antibiotics with > 90% susceptibility for BSI, but only AMK and MEM were > 90% effective antibiotics against IAI. High-susceptibility to antibiotics in UTI included AMK, TOB and MEM (all > 90%), and except for AMK, COL and TOB, the susceptibility to other antibiotics at the site of RTI infections was < 80% (Fig. 5 , Supplementary Table 6 ).
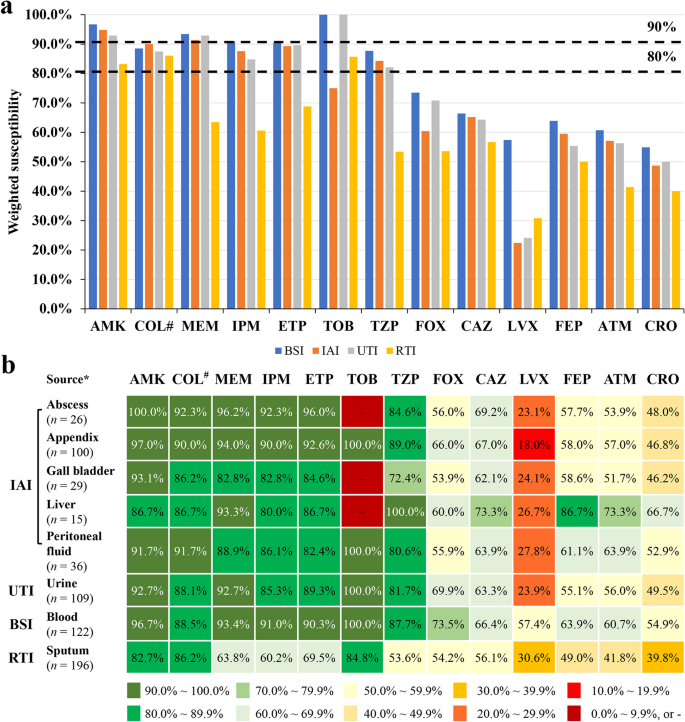
Organ distribution related susceptibilities. a Differences in susceptibility of antibiotics at different infection sites. b Differences in weighted drug susceptibilities of antibiotics at different organs and infection sites. Note: *only sites from which more than 10 pathogenic bacteria were collected have been included; #, intermediate rate was shown for COL; -, no detection. Abbreviations: AMK, amikacin; ATM, aztreonam; BSI, blood steam infections; CAZ, ceftazidime; CRO, ceftriaxone; ETP, ertapenem; FEP, cefepime; FOX, cefoxitin; IAI, intra-abdominal infections; IPM, imipenem; LVX, levofloxacin; MEM, meropenem; RTI, respiratory tract infections; TOB, tobramycin; TZP, piperacillin/tazobactam; UTI, urinary tract infections
This study analyzed Chinese data from the global SMART surveilance program and found that the most frequently isolated Gram-negative bacteria were Enterobacterales , a finding similar to previous results from SMART studies and the China Antimicrobial Surveillance Network (CHINET) [ 13 , 14 ]. Enterobacterales are of particular concern given their ability to develop and spread resistance to penicillins, cephalosporins, carbapenems and quinolones [ 12 , 15 , 16 ]. As these are the most commonly used antibiotics in hospitals, such resistance would leave physicians with very limited treatment options. The vast majority of the pathogens were E. coli , K. pneumoniae and P. aeruginosa (86.4%), with resistance rates for cephalosporins in the range of 31.0%–57.0% and for ATM 44.0%–45.5%, indicating a high rate of ESBL-producing strains [ 17 ], which underlines the global health problem of cephalosporin resistance [ 18 ]. Previous SMART surveilence results found ESBL rates of 46.3%–49.1% for E. coli and 25.6%–26.8% for K. pneumoniae [ 13 ]. In the 2021 CHINET surveillance, resistance to third-generation cephalosporins was detected in 55.6% of E. coli and 43.8% of K. pneumoniae , also indicating the high ESBL prevalence in China [ 14 ]. The resistance rates for the fluoroquinolone LVX (36.6%–56.7%) were in a similar range to cephalosporins in this study, which might reflect the overuse of fluoroquinolones, especially since the development of cephalosporin-resistance [ 19 , 20 ]. They were similar to the rates reported by the 2021 CHINET surveillance of LVX resistance detected as 53.6% for E. coli and 28.3% for K. pneumoniae isolates [ 14 ]. One approach to overcome cephalosporin resistance is the use of combination of a β-lactam and a β-lactamase inhibitor [ 21 ], such as tazobactam, which led to essentially reduced resistance rates of about 10% for otherwise cephalosporin-resistant E. coli and K. pneumoniae in the present study. Of concern is the rising resistance rate of K. pneumoniae to carbapenems , which reached25%–29% in the present study and was similar to the rate of about 25% found in the 2021 CHINET surveillance study [ 14 ].
Resistance rates for COL were generally low, but susceptibility breakpoints have been abolished in recent CLSI guidelines. Treatments with COL should be applied with maximum renally adjusted doses, since the previous MIC of 2 μg/mL could not be achieved in 50% of patients with normal renal functions and acute kidney injury occurs frequently with conventional doses. Recommendations include strongly preferred alternative drugs for active or combination treatments [ 22 , 23 ]. Also, TOB is not commonly used in China, which might explain the low resistance rates found in the present study.
P. aeruginosa was the third most common pathogen detected and the most common Gram-negative pathogen found in RTI. It exhibited > 30% resistance to traditional antipesudomoas antibiotics, including CAZ, FEP, TZP, IPM, MEM and LVX. These results are similar to those reported in a recent SMART study that investigated P. seudomonas resistance to antibiotics in China [ 24 ].
This present survey included only isolates collected in EDs, since patients admitted to EDs are frequently candidates for urgent empiric antibiotic treatment, which should be administered according to the site of infection and the clinical severity of symptoms [ 25 ]. The characteristics of infected patients and physicians' routine treatments in the ED differed compared to other departments. This is because the infected site may initially not be clearly defined, patients cannot be observed for a long period of time, and etiological evidence is rarely available; doctors and nurses in EDs also have a very heavy workload. It is therefore convenient to use drugs which only need administration once a day to ED patients, including ETP once a day, AMK intramuscular injection, as well as LVX once a day, which can be sequenced simultaneously.
In order to offer guidelines for chosing an empiric treatment, organ specific therapy based on pathogen distribution differences and their antibiotic resistance variations have been developed [ 6 , 8 ]. Of these, OSIWA was first applied for HA and CA infections of different intra-abdominal organs [ 9 ]. In the present study, we expanded the evaluation of OSIWA for the empirical treatment of IAI also to UTI, BSI and RTI. When considering the distribution of pathogens at a single infection site – for example E. coli caused more than 50% of all IAI and more than 60% of all UTI – whereas for RTI infections E. coli was the pathogen in < 15% of all cases (Fig. 3 ). The OSIWA shown in Fig 5 indicate the probabilities of successful empiric drug treatment for single infections sites. For RTI and IAI the choice of empirical antibiotics with expected efficacy was limited, but for UTI and BSI more antibiotics are available.
Limitations of the present survey were the relatively low sample numbers since only isolates from EDs have been included, which have had an influence on the resistance patterns reported and combination treatments with β-lactams, aminoglycoside and fluoroquinolone were not considered. In addition, since in the SMART data collection detailed data regarding resistance mechanisms are not included, susceptibility test results only can infer the mechanism of ESBL production in cephalosporin but not in carbapenem resistance.
The pathogens isolated from BSI, IAI, UTI and RTI between 2016 and 2019 in Chinese EDs were mainly E. coli, K. pneumoniae and P. aeruginosa ,but therewere considerable resistance pattern differences as well as organ distributions between the bacterial strains. OSIWA determinations led to organ specific antibiotic drug effectiveness patterns, which should help to guide the choice of suitable empirical antibiotic treatments, especially for urgent infected cases in EDs.
Availability of data and materials
The SMART database is not public and is only accessible to SMART investigators, but the data that support the findings of this study are directly available from MSD China or from the corresponding author Yunsong Yu upon reasonable request and with permission of MSD China.
Abbreviations
blood stream infections
community acquired
ceftazidime
China Antimicrobial Surveillance Network
ceftriaxone
emergency departments
hospital acquired
intra-abdominal infections
levofloxacin
minimum inhibitory concentrations
organ-specific weighted incidence antibiograms
respiratory tract infections.
Study for Monitoring Antimicrobial Resistance Trends
piperacillin–tazobactam
urinary tract infections
Zhu Y, Qiao Y, Dai R, Hu X, Li X. Trends and patterns of antibiotics use in China’s Urban tertiary hospitals, 2016-19. Front Pharmacol. 2021;12:757309.
Article CAS PubMed PubMed Central Google Scholar
Luyt C-E, Bréchot N, Trouillet J-L, Chastre J. Antibiotic stewardship in the intensive care unit. Crit Care. 2014;18(5):480.
Article PubMed PubMed Central Google Scholar
Evans L, Rhodes A, Alhazzani W, Antonelli M, Coopersmith CM, French C, et al. Surviving sepsis campaign: international guidelines for management of sepsis and septic shock 2021. Crit Care Med. 2021;49(11):e1063-1143.
Article PubMed Google Scholar
Hay SI, Rao PC, Dolecek C, Day NPJ, Stergachis A, Lopez AD, et al. Measuring and mapping the global burden of antimicrobial resistance. BMC Med. 2018;16(1):78.
Schnall J, Rajkhowa A, Ikuta K, Rao P, Moore CE. Surveillance and monitoring of antimicrobial resistance: limitations and lessons from the GRAM project. BMC Med. 2019;17(1):176.
Randhawa V, Sarwar S, Walker S, Elligsen M, Palmay L, Daneman N. Weighted-incidence syndromic combination antibiograms to guide empiric treatment of critical care infections: a retrospective cohort study. Crit Care. 2014;18(3):R112.
Cook A, Sharland M, Yau Y, Group* P, Bielicki J. Improving empiric antibiotic prescribing in pediatric bloodstream infections: a potential application of weighted-incidence syndromic combination antibiograms (WISCA). Expert Rev Anti Infect Ther. 2022;20(3):445–56.
Article CAS PubMed Google Scholar
Hebert C, Ridgway J, Vekhter B, Brown EC, Weber SG, Robicsek A. Demonstration of the weighted-incidence syndromic combination antibiogram: an empiric prescribing decision aid. Infect Control Hosp Epidemiol. 2012;33(4):381–8.
Liu L, Ni Y. Antimicrobial susceptibilities of specific syndromes created with organ-specific weighted incidence antibiograms (OSWIA) in patients with intra-abdominal infections. BMC Infect Dis. 2018;18(1):584.
Chinese Society of Surgical Infection and Intensive Care, Chinese Society of Surgery, Chinese Medical Association. Chinese College of Gastrointestinal Fistula Surgeons, Chinese College of Surgeons, Chinese Medical Doctor Association. Chinese guideline for the diagnosis and management of intra-abdominal infection (2019 edition). Chin J Practical Surg. 2020;40(1):1–16.
Google Scholar
Chinese Medical Association. Clinical Guidelines: Respiratory diseases. Beijing: People’s Medical Publishing House; 2009. p. 174.
Nordmann P, Poirel L. Emergence of plasmid-mediated resistance to quinolones in enterobacteriaceae. J Antimicrob Chemother. 2005;56(3):463–9.
Zhang H, Johnson A, Zhang G, Yang Y, Zhang J, Li D, et al. Susceptibilities of Gram-negative bacilli from hospital- and community-acquired intra-abdominal and urinary tract infections: a 2016–2017 update of the Chinese SMART study. Infect Drug Resist. 2019;12:905–14.
Fupin HU, Yan GUO, Demei ZHU, Fu W, Xiaofei J, Yingchun XU, et al. CHINET surveillance of antimicrobial resistance among the bacterial isolates in 2021. Chin J Infect Chemother. 2022;22(5):521–30.
Ma J, Song X, Li M, Yu Z, Cheng W, Yu Z, et al. Global spread of carbapenem-resistant Enterobacteriaceae: Epidemiological features, resistance mechanisms, detection and therapy. Microbiol Res. 2023;266:127249.
De Angelis G, Del Giacomo P, Posteraro B, Sanguinetti M, Tumbarello M. Molecular mechanisms, epidemiology, and clinical importance of beta-lactam resistance in enterobacteriaceae. Int J Mol Sci. 2020;21(14):5090.
Rawat D, Nair D. Extended-spectrum β-lactamases in gram negative bacteria. J Glob Infect Dis. 2010;2(3):263–74.
Pana ZD, Zaoutis T. Treatment of extended-spectrum β-lactamase-producing Enterobacteriaceae (ESBLs) infections: what have we learned until now? F1000Res.2018;7:F1000 Faculty Rev-1347.
Ezelarab HAA, Abbas SH, Hassan HA, Abuo-Rahma GEA. Recent updates of fluoroquinolones as antibacterial agents. Arch Pharm (Weinheim). 2018;351(9):e1800141.
Hou J, Long X, Wang X, Li L, Mao D, Luo Y, et al. Global trend of antimicrobial resistance in common bacterial pathogens in response to antibiotic consumption. J Hazard Mater. 2023;442:130042.
Yahav D, Giske CG, Grāmatniece A, Abodakpi H, Tam VH, Leibovici L. New β-Lactam-β-Lactamase Inhibitor Combinations. Clin Microbiol Rev. 2020;34(1);e00115.
Satlin MJ, Lewis JS, Weinstein MP, Patel J, Humphries RM, Kahlmeter G, et al. Clinical and laboratory standards institute and European committee on antimicrobial susceptibility testing position statements on polymyxin b and colistin clinical breakpoints. Clin Infect Dis. 2020;71(9):e523-529.
CAS PubMed Google Scholar
Tsuji BT, Pogue JM, Zavascki AP, Paul M, Daikos GL, Forrest A, et al. International consensus guidelines for the optimal use of the polymyxins: endorsed by the American College of Clinical Pharmacy (ACCP), European Society of Clinical Microbiology and Infectious Diseases (ESCMID), Infectious Diseases Society of America (IDSA), International Society for Anti-infective Pharmacology (ISAP), Society of Critical Care Medicine (SCCM), and Society of Infectious Diseases Pharmacists (SIDP). Pharmacotherapy. 2019;39(1):10–39.
Croche Santander B, Campos Alonso E, Sanchez Carrion A, Marcos Fuentes L, Diaz Flores I, Vargas JC, et al. [Appropriateness of antibiotic prescribing in paediatric patients in a hospital emergency department]. Pediatr (Engl Ed). 2018;88(5):259–65.
Kollef MH, Shorr AF, Bassetti M, Timsit J-F, Micek ST, Michelson AP, et al. Timing of antibiotic therapy in the ICU. Crit Care. 2021;25(1):360.
Download references
Acknowledgements
The authors thank Shanghai BIOMED Science Technology Co., Ltd (Shanghai, China) for providing editorial assistance and MSD China for their financial support.
This study was sponsored by funding from Merck Sharp & Dohme LLC, a subsidiary of Merck & Co., Inc., Rahway, New Jersey, USA. The funding body was involved in the study design, analysis and interpretation of data, as well as the decision to submit the article for publication.
Author information
Authors and affiliations.
Department of Clinical Laboratory, Sir Run Run Shaw Hospital, School of Medicine, Zhejiang University, 310016, Hangzhou, Zhejiang Province, China
Ying Fu, Feng Zhao & Jie Lin
Key Laboratory of Precision Medicine in Diagnosis and Monitoring Research of Zhejiang Province, 310016, Hangzhou, Zhejiang Province, China
MRL Global Medical Affairs, MSD China, 200233, Shanghai, China
Pengcheng Li
Department of Infectious Diseases, Sir Run Run Shaw Hospital, School of Medicine, Zhejiang University, 310016, Hangzhou, Zhejiang Province, China
Key Laboratory of Microbial Technology and Bioinformatics of Zhejiang Province, 310012, Hangzhou, Zhejiang Province, China
Regional Medical Center for National Institute of Respiratory Diseases, Sir Run Run Shaw Hospital, School of Medicine, Zhejiang University, 310016, Hangzhou, Zhejiang Province, China
You can also search for this author in PubMed Google Scholar
Contributions
All authors made substantial contributions to the conception and design of the study, acquisition of data, or analysis and interpretation of data, took part in drafting the manuscript or critically revising it for important intellectual content, agreed to submit it to the current journal, gave final approval of the version to be published and agreed to be accountable for all aspects of the work.
Corresponding author
Correspondence to Yunsong Yu .
Ethics declarations
Ethical approval and consent to participate, consent for publication.
Not applicable.
Competing interests
Pengcheng Li is an employee of MSD China. All other authors declare no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Supplementary material 1., rights and permissions.
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Fu, Y., Zhao, F., Lin, J. et al. Antibiotic susceptibility patterns and trends of the gram-negative bacteria isolated from the patients in the emergency departments in China: results of SMART 2016–2019. BMC Infect Dis 24 , 501 (2024). https://doi.org/10.1186/s12879-024-09294-0
Download citation
Received : 14 December 2023
Accepted : 05 April 2024
Published : 17 May 2024
DOI : https://doi.org/10.1186/s12879-024-09294-0
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Antibiogram
- Cephalosporin
- Antibiotic-Resistance
BMC Infectious Diseases
ISSN: 1471-2334
- Submission enquiries: [email protected]
- General enquiries: [email protected]
A .gov website belongs to an official government organization in the United States.
A lock ( ) or https:// means you've safely connected to the .gov website. Share sensitive information only on official, secure websites.
- Risk Factors
- Four Steps to Food Safety
- Educational Materials and Videos
- Foods That Can Cause Food Poisoning
- Information for Healthcare Professionals
- Restaurant Food Safety
- About Norovirus
Food Safety

About Four Steps to Food Safety
Featured content

People at Increased Risk for Food Poisoning

Symptoms of Food Poisoning

CDC and Food Safety
More food safety content

Safer Food Choices

Safer Food Choices for Pregnant People

Safer Food Choices for Children Under 5 Years Old

Safer Food Choices for Adults 65 Years or Older

Safer Food Choices for People With Weakened Immune Systems
Get information from CDC on preventing food poisoning, food poisoning symptoms, foodborne disease outbreaks, and recalled food.
For Everyone
Health care providers.
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- Can J Infect Dis
- v.14(5); Sep-Oct 2003
Food safety and foodborne disease in 21st century homes
Over the past decade there has been a growing recognition of the involvement of the home in several public health and hygiene issues. Perhaps the best understood of these issues is the role of the home in the transmission and acquisition of foodborne disease. The incidence of foodborne disease is increasing globally. Although foodborne disease data collection systems often miss the mass of home-based outbreaks of sporadic infection, it is now accepted that many cases of foodborne illness occur as a result of improper food handling and preparation by consumers in their own kitchens. Some of the most compelling evidence has come from the international data on Salmonella species and Campylobacter species infections.
By its very nature, the home is a multifunctional setting and this directly impacts upon the need for better food safety in the home. In particular, the growing population of elderly and other immnocompromised individuals living at home who are likely to be more vulnerable to the impact of foodborne disease is an important aspect to consider. In addition, some developed nations are currently undergoing a dramatic shift in healthcare delivery, resulting in millions of patients nursed at home. Other aspects of the home that are unique in terms of food safety are the use of the home as a daycare centre for preschool age children, the presence of domestic animals in the home and the use of the domestic kitchen for small-scale commercial catering operations. At the global level, domestic food safety issues for the 21st century include the continued globalization of the food supply, the impact of international travel and tourism, and the impact of foodborne disease on developing nations.
A number of countries have launched national campaigns to reduce the burden of foodborne disease, including alerting consumers to the need to practice food safety at home. Home hygiene practice and consumer hygiene products are being refined and targeted to areas of risk, including preventing the onward transmission of foodborne illness via the inanimate environment. It has been said that food safety in the home is the last line of defense against foodborne disease, and it is likely that this will remain true for the global population in the foreseeable future.
THE INCIDENCE OF FOODBORNE DISEASE
There are many indicators that point to the fact that the incidence of foodborne disease is increasing globally, and is a substantial cause of morbidity and mortality worldwide. For industrialized countries in general, it has been estimated that up to one-third of the population suffer a foodborne illness each year ( 1 ). In the United States, foodborne diseases cause an estimated 76 million episodes of illness annually ( 2 ). Although the vast majority of cases are mild, a significant number of deaths do occur and the high levels of acute infections and chronic sequelae lead to billions of dollars in medical costs and lost productivity ( 3 ).
It can be assumed that the prevalence of foodborne disease in the developing world is even higher ( 4 ), although it is difficult to obtain the data that would support this assumption. While it has long been considered that most cases of diarrhea in developing countries are waterborne, Kaferstein ( 5 ) has recently stated that it is a grave mistake to ignore the role of contaminated food and that there is an urgent need to integrate food safety, along with water and sanitation programs, as an essential strategy to prevent diarrhea. A recent study of campylobacteriosis in developing countries ( 6 ) gave an insight into the prevalence of Campylobacter species, which is the most commonly isolated bacterial pathogen from children under two years of age suffering from diarrhea. Isolation rates for children under five years of age were estimated to be between 40,000 per 100,000 and 60,000 per 100,000, compared with 300 per 100,000 in developed countries. The study found that the major sources of human infection were food and environmental contamination and a survey of retail poultry sold in Bangkok and Nairobi ( 6 ) found Campylobacter species contamination rates of between 40% and 77%. Coker et al ( 6 ) reported that this disease is projected to remain one of the top ten isolated bacterial pathogens globally in 2020. Campylobacteriosis is considered to be a greater burden in the developing world, partly because Campylobacter species-associated diarrhea and bacteremia occur in HIV/AIDS patients.
THE ROLE OF THE HOME IN FOODBORNE DISEASE
Although foodborne disease data collection systems often miss the mass of home-based outbreaks of sporadic infection, it is now widely accepted that many cases of foodborne illness occur as a result of improper food handling and preparation by consumers in their own kitchens, as shown in a review of studies from both Europe and North America ( 7 ). In addition, a study of Escherichia coli O157 outbreaks in the United States ( 8 ) found that 80% of suspect hamburgers were prepared and eaten at home. In Australia, approximately 90% of Salmonella species infections are generally thought to be associated with nonmanufactured foods and the home ( 9 ). Data available from Canada covering 1996 and 1997 has identified the home as the most common exposure setting for cases of Salmonella species, Campylobacter species and pathogenic E coli infection ( 10 ).
There are a number of factors which are likely to contribute to outbreaks of foodborne illness in the home, including a raw food supply that is frequently contaminated, a lack of awareness among the general public, mistakes in food handling and food preparation at home and the deliberate consumption of raw and undercooked foods of animal origin, often described as 'risky eating behaviour' ( 4 ).
Raw foods, including meat and poultry, raw eggs, fish and shellfish, and fruits and vegetables, should all be considered as potential entry sources of foodborne pathogens into the home. The list of infectious agents that have been introduced into the home via food includes species of Salmonella, Camylobacter, Listeria and E coli O157 ( 11 ).
The human and animal occupants of the home can also serve as sources of foodborne pathogens. Humans and animals can both serve as symptomatic and nonsymptomatic carriers and also as postsymptomatic excreters. Pathogens can be transferred from various sources to inanimate contact surfaces in the home or directly to other foods or human occupants via transient carriage on the hands. Foodborne agents that have been introduced into the home via humans include species of Salmonella, Shigella sonnei, Staphylococcus aureus , rotavirus and hepatitis A virus ( 11 ).
The four most common mistakes in handling and preparing food at home are the inappropriate storage of food (including inadequate refrigeration, the failure to attain a required cooking and/or reheating temperature), any actions that result in cross-contamination, and the presence of an infected food handler. In a study of 101 home-based outbreaks ( 12 ), it was determined that inappropriate food storage and cross-contamination were the most prevalent mistakes, accounting for 50% and 28% of reported causative factors, respectively.
FACTORS THAT IMPACT FOOD SAFETY INSIDE THE 21 st CENTURY HOME
In order to understand the challenges to food safety in the home, it is worthwhile to consider the relevant elements that comprise a typical modern-day home in this early part of the 21 st century. It is also worth noting that in many parts of the world, the home is in fact a multifunctional setting comprising many activities that may have an impact on the need for, and practice of, food safety.
First and foremost, the home is a residence containing occupants of mixed ages and health statuses. In many parts of the world the numbers of immunocompromised individuals living in the community is on the increase and, amongst other things, these people are often at a higher risk for the acquisition of foodborne disease as well as for a more severe disease outcome. In the United States, the population of immunocompromised individuals is estimated at more than 30 million people ( 13 ). In many countries of the developed world, the elderly population is the fastest growing segment of the population, as for example in the United Kingdom, where there are currently nine million senior citizens, most of them living at home ( 14 ). For the developing world, one only has to consider the impact of the AIDS epidemic and the numbers of people living with HIV/AIDS to get some measure of the size of the immunocompromised populations in these areas ( 15 ).
With a dramatic shift in healthcare delivery, the home in the United States is increasingly playing a role as an extension to, or replacement for, traditional in-hospital care. It is estimated that eight million patients are now nursed at home, with 66% of them being over 65 years old ( 16 ). Again, this puts a renewed emphasis on the need for food safety in the home, much as might be expected if these patients were being cared for within the hospital.
Another growing home-based activity that may impact food safety in the home is the presence of young children in home-based daycare. In the United States, 75% of under-five-year-olds are currently enrolled in daycare ( 17 ), representing 13 million preschoolers and six million infants. Much of this child care is home-based, with 25% of all children cared for by relatives and 5% by in-home caregivers. There are many reports of outbreaks of infectious diseases, including diarrhea, in children's day care settings ( 18 ) and the potential for infection to spread within the home via food is inevitably increased in these situations. In addition, small and/or unlicensed home-based daycare settings are less likely to have outbreaks reported and investigated, and may, therefore, miss advice and information about the importance of appropriate food safety practices.
In addition to its human occupants, the home is frequently shelter to a number of pets, ranging from mundane varieties to the exotic, and many zoonoses, including some that can cause foodborne infections, can be acquired from both. Salmonella species and other enteropathogens have long been recognized in association with domestic pets, such as cats and dogs ( 19 ). Household cats and dogs may also serve as reservoirs for species of Campylobacter and, thus, are potential sources of infection (20). Exotic pets may also serve as a source of enteropathogens into the home ( 21 ). More than 50% of homes in the English-speaking world have cats and dogs ( 14 ), with 14 million cats and dogs in the United Kingdom, 60 million in the United States and an estimated 17.8 million household pets in Australia, with three in every five Australian households containing at least one pet ( 22 ). The role of household pets in the acquisition of Salmonella species infections by infants was described by Schutze et al ( 23 ). It was found that infants in this study were probably more likely to have acquired infections by direct contact with inanimate surfaces, such as floors, that had been contaminated by household pets, than by the consumption of contaminated foods.
Finally, when considering the question of food safety in the home, we usually think of food that is prepared and served to the home occupants. However, we should also consider that the home kitchen may also be used for small home-based business operations that prepare food for catered functions outside of the home, as well as for bake sales, school and church picnics, etc. In all of these examples, food prepared at home is served to a wider community. These catering activities are usually unregulated, often take place in kitchens with inadequate facilities and equipment, and are carried out by people who may not have taken a training course in food safety. A study of home-based catering operations in the in the United Kingdom noted that food was stored inappropriately in the home kitchen on 50% of occasions ( 12 ).
GLOBAL IMPACTS ON FOOD SAFETY IN THE HOME
There are also a number of global factors that have an impact on food safety inside the 21 st century home. In particular, the globalization of the food supply impacts homes all over the world.
World meat consumption is expected to double between 1983 and 2020, to 300 million metric tons, and most of this increase will occur in developing countries ( 24 ). The impact on food safety for homes in these countries may be significant, considering that meat processing may not be well regulated, home kitchens may not be equipped for storage and preparation of raw meats and the population may not be familiar with the general food safety guidelines for meat storage and preparation, especially where the consumption of large quantities of meat protein is a new phenomenon. The aforementioned study on campylobacteriosis in the developing world ( 6 ) indicates the potential magnitude of the problem surrounding poultry production.
Import statistics indicate that more than 50% of fresh vegetables in the developed world marketplace are imported from developing countries ( 25 ), prompting food safety experts to quip that consumers only have to travel as far as the local foodmarket and home again to experience 'traveller's diarrhea'.
International travel and tourism to countries with poor standards of food hygiene may also impact the home. Globally, 1.6 billion people travel by air each year ( 26 ). Rapid air travel means that people who have contracted gastroenteric infections may carry these agents back into their homes, with the potential for further spread within the family and the immediate community, both directly by person-to-person contact and indirectly by cross-contamination into the food prepared at home. The potential for this type of transmission is seen in a World Health Organization report ( 27 ) that states that 64% of tourists exiting Thailand in 1995 were suffering from diarrhea.
IMPROVING FOOD SAFETY IN THE 21 st CENTURY HOME
It has been said that there are three major lines of defense against foodborne disease ( 4 ). The first aims at improving the hygienic quality of raw foodstuffs; the second utilizes food processing technologies such as pasteurization and irradiation, and employs hazard analysis and critical control point (HACCP) concepts; and the third line of defense concerns the education of all food handlers, including home-based food handlers. There are a number of national campaigns, for example the Canadian Partnership for Consumer Food Safety Education in Canada ( 28 ), the Partnership for Food Safety Education in the United States ( 29 ), the Food Standards Agency in the United Kingdom ( 30 ), and international campaigns, such as the World Health Organization's Food Safety Program ( 31 , that aim to inform and educate the general public about the need to better understand and practice food safety in the home. These campaigns are comprehensive and address real concerns, but inevitably tend to be web and print media-based and, in this respect, they are a passive form of information transfer and are likely to be taken up only by that segment of the population that is actively searching for information. In many countries, the subject of food safety was traditionally taught as a part of the home economics curriculum in schools, but in recent years the teaching of home economics has largely disappeared from many national education programs and, as a result, food safety is not taught. In addition, changes in family structure, changes in family meal practices and changes in women's roles in the home and workplace have resulted in a breakdown in the transfer of information about safe food practices within the family. With increasing concern in many countries about the levels of foodborne disease and the huge national economic burden associated with these levels, the introduction of mandatory food safety education programs across schools should be considered as a means of actively educating and engaging the population in a basic health issue.
In practical terms, food safety education and information is increasingly incorporating the targeted hygiene approach developed and described by the International Hygiene Forum in their Guidelines for prevention of infection and cross infection in the domestic environment ( 32 ). Targeted hygiene is a risk-based approach to hygiene practice in the home, similar to the HACCP approach so widely used in the commercial food sector. Targeted hygiene assesses the relative need for a hygiene intervention based upon the source of pathogens into the home, the potential routes of transfer of pathogens within the home and the likely risk posed by the transfer of these agents to a family member. Recommendations can then be given for safe and effective hygiene procedures aimed at eliminating pathogens from those surfaces that present a risk, thereby reducing the risk of pathogen transfer to other sites and surfaces.
Foodborne disease will continue to be a matter of major concern around the world in the foreseeable future, despite some important national successes at reducing the levels of certain pathogens in foods resulting from better farm practices, food processing regulations, etc. Therefore, it has to be concluded that the 21 st century home will also continue to remain the last line of defense against foodborne pathogens. Public education is seen as a key factor in improving food safety practices in the home. The benefits of food hygiene education would include not only a reduction in the occurrence of foodborne illness at home, but also a population better prepared to meet the needs of the food industry and food service sectors of local and national economies.

IMAGES
VIDEO
COMMENTS
"Food-borne Disease Prevention and Risk Assessment" is a Special Issue of the International Journal of Environmental Research and Public Health on understanding how food-borne disease is still a global threat to health today and to be able to target strategies to reduce its prevalence. Despite decades of government and industry interventions, food-borne disease remains unexpectedly high in ...
Before that he was in the Bureau of Microbial Hazards, Health Products and Food Branch, Health Canada, Ottawa where he was a research scientist for 33 years working on methods development for pathogens in foods, foodborne disease investigation and reporting, costs and surveillance of disease, illnesses caused by seafood toxins, and risk ...
Illnesses, hospitalizations, and death research estimates related to foodborne illness in the United States including findings on Salmonella, Toxoplasma, Listeria, Campylobacter, E. coli O157, Clostridium perfringens, and norovirus. Estimates of burden of illness are designed to give the most accurate picture yet of which foodborne bacteria, viruses, microbes (pathogens) are causing the most ...
Foodborne diseases are reflected in several targets of Sustainable Developmental Goal 3 and are a priority area within the Organization's work. Activities include research and independent scientific assessments of food-related hazards, foodborne disease awareness programs, and helping to promote food safety through national health-care programs.
These estimates are known as the attribution of foodborne illness. By estimating the burden of foodborne illness and attributing illnesses to specific food sources, CDC, regulatory agencies, industry, consumer groups, and others can better target prevention measures and improve food safety in the United States.
Diarrhea, dark urine, jaundice, and flu-like symptoms, i.e., fever, headache, nausea, and abdominal pain. Variable, 2 weeks-3 months. Raw produce, contaminated drinking water, uncooked foods and ...
Around the world unsafe food is known to cause more than 200 acute and chronic diseases. In 2015, WHO published the first-ever estimates of global burden of foodborne diseases, which indicated that the 31 hazards examined were responsible for 600 million cases of foodborne diseases in 2010, resulting in 33 million disability-adjusted life years (DALYs), including 420 000 deaths worldwide.
The 2016 FSS is the seventh wave of a repeated cross-sectional survey conducted by the U.S. Food and Drug Administration in collaboration with the U.S. Department of Agriculture. The goal of the ...
Perspectives in Foodborne Illness. This article provides a historical framework on food safety for more contemporary details to rest on, focusing primarily on the past 100 years or so (with a touch of ancient history) as particular issues that affect how the safety of the food we eat have been appreciated, have evolved or at times have been ...
Foodborne diseases are an important public health burden in the United States. First, we estimate that 31 of the most important known agents of foodborne disease found in foods consumed in the United States each year cause 9.4 million illnesses, 55,961 hospitalizations, and 1,351 deaths. Second, not all agents of foodborne disease are known or ...
Introduction. Foodborne diseases (FBD) still cause a substantial public health, economic and social burden worldwide. Recognizing the need to measure the burden and distribution of FBD and encourage evidence-informed policies, in 2015 the World Health Organization (WHO) reported the first estimates of global and regional disease burden due to 31 foodborne hazards [1].
Outbreaks of Foodborne Illness. When two or more people get the same illness from the same contaminated food or drink, the event is called a foodborne illness outbreak. FDA investigates outbreaks ...
From 2013 to 2018, the economic burden of illnesses stemming from 15 foodborne pathogens in the United States rose $2 billion to $17.6 billion when adjusted for inflation and income growth. The biggest factor was in the cost of preventing deaths, a calculation that takes into account how much people are willing to reduce the risk of death from a particular illness.
Foodborne illness investigations are multi-faceted, multidisciplinary undertakings that involve collecting and analyzing data from a variety of sources. Epidemiologic, laboratory, and environmental evidence help guide the short-term response and long-term preventive actions of public health organizations working to minimize or prevent further ...
Foodborne Bacteria Table. Contaminated water, raw or unpasteurized milk, and raw or undercooked meat, poultry, or shellfish. Diarrhea (sometimes bloody), cramping, abdominal pain, and fever that appear 2 to 5 days after eating; may last 7 days. May spread to bloodstream and cause a life- threatening infection.
Food poisoning, a type of foodborne illness, is a sickness people get from something they ate or drank. The causes are germs or other harmful things in the food or beverage. Symptoms of food poisoning often include upset stomach, diarrhea and vomiting. Symptoms usually start within hours or several days of eating the food.
Help Solve! Last Reviewed: April 30, 2024. Source: Centers for Disease Control and Prevention, National Center for Emerging and Zoonotic Infectious Diseases (NCEZID), Division of Foodborne, Waterborne, and Environmental Diseases (DFWED) See current foodborne outbreaks and learn how CDC investigates foodborne outbreaks.
Foodborne Illness: Pathogens and Diseases. June 2019. In book: Research Trends in Food Technology and Nutrition Vol-8 (pp.1-20) Chapter: First. Publisher: AkiNik Publications. Authors: Ena Gupta ...
Product (s) Linked to Illnesses (if any): During an outbreak or adverse event investigation, the FDA and CDC, along with state and local authorities collect and analyze three types of information ...
Foodborne pathogens are causing a great number of diseases with significant effects on human health and economy. The characteristics of the most common pathogenic bacteria (Bacillus cereus, Campylobacter jejuni, Clostridium botulinum, Clostridium perfringens, Cronobacter sakazakii, Esherichia coli, Listeria monocytogenes, Salmonella spp., Shigella spp., Staphylococccus aureus, Vibrio spp. and ...
By Coral Beach on May 15, 2024. Research funded in part by the CDC has shown that food irradiation could reduce the number of foodborne outbreaks caused by pathogens. For the project, researchers ...
Dec 15, 2023. Knowledge Article. According to the Centers for Disease Control and Prevention (CDC), the two leading causes of foodborne illness are (1) Eating raw or undercooked foods such as meat, poultry, seafood and eggs; and (2) Allowing food to remain at an unsafe temperature too long -- for example, leaving cooked foods out to cool after ...
Foodborne infection is a major health issue and its impact on global social and economic development remains unknown ().A paper published in the journal Nature estimates 30% of all infections over the last 60 years were Foodborne ().The Centre for Disease Control in the United States estimates that 76 million people per year are affected by Foodborne illness, with 300,000 requiring hospital ...
The pasteurization process was invented in the 1860s and continues to keep people safe from a range of foodborne illnesses. ... Research so far has shown that virus particles end up in the milk ...
The study aims were to evaluate the species distribution and antimicrobial resistance profile of Gram-negative pathogens isolated from specimens of intra-abdominal infections (IAI), urinary tract infections (UTI), respiratory tract infections (RTI), and blood stream infections (BSI) in emergency departments (EDs) in China. From 2016 to 2019, 656 isolates were collected from 18 hospitals across ...
Certain groups are at higher risk for foodborne illness. Apr. 29, 2024. Symptoms of Food Poisoning. Food poisoning symptoms include diarrhea, stomach pain or cramps, nausea, vomiting, and fever. Apr. 29, 2024. CDC and Food Safety. CDC determines prevention measures for foodborne illness and works with partners. May 2, 2024.
At the global level, domestic food safety issues for the 21st century include the continued globalization of the food supply, the impact of international travel and tourism, and the impact of foodborne disease on developing nations. A number of countries have launched national campaigns to reduce the burden of foodborne disease, including ...