

Case Studies in Emergency Medicine
LEARNing Rounds: Learn, Evaluate, Adopt, Right Now
- © 2020
- Colin G. Kaide 0 ,
- Christopher E. San Miguel 1
Wexner Medical Center, Ohio State University, Columbus, USA
You can also search for this editor in PubMed Google Scholar
- Discusses physiology, pathophysiology, diagnosis, and treatment of each disease
- Presented in an easy-to-read, bulleted format with many images
- Includes not only the usual cases that present to the ED but also “can’t miss” very specific cases
105k Accesses
3 Citations
5 Altmetric
This is a preview of subscription content, log in via an institution to check access.
Access this book
- Available as EPUB and PDF
- Read on any device
- Instant download
- Own it forever
- Compact, lightweight edition
- Dispatched in 3 to 5 business days
- Free shipping worldwide - see info
Tax calculation will be finalised at checkout
Other ways to access
Licence this eBook for your library
Institutional subscriptions
About this book
This book contains a variety of medical case studies from actual patients presenting to the emergency department. It includes not only typical cases that present to the ED but also less common, yet very important cases that one can't afford to miss.
Using a concise, easy-to-read, bulleted format, the book helps readers to learn, evaluate, adopt new practices, right now (LEARN). Emergency Medicine Case Studies - LEARNing Rounds: Learn, Evaluate, Adopt, Right Now is an essential resource for a variety of emergency medicine clinicians including experienced physicians, residents, physician assistants, nurse practitioners, nurses, and medical students rotating in the emergency department. Finally, this book can be used as a basis for small group discussions, especially in emergency medicine training programs.
Similar content being viewed by others

Everyone Called Him Crazy

How to Deal with a Difficult Patient
What is the prevalence of frequent attendance to emergency departments and what is the impact on emergency department utilisation? A systematic review and meta-analysis
- Case studies in emergency medicine
- Diagnosis in the emergency department
- Emergency medicine case studies
- Physiology and pathophysiology of diseases
- Rare cases in the emergency department
- Treatment in the emergency department
Table of contents (68 chapters)
Front matter, bleeding on anti-xa drugs: “ does all bleeding really stop ”.
- Colin G. Kaide, Kelsey Kauffman
Beta-Blocker Overdose: “You know, the green pill.”
- Katherine H. Buck, Colin G. Kaide
Acute Blast Crisis/Hyperviscosity Syndrome: Blasting Off!
- Colin G. Kaide, Geremiha Emerson
Black Widow Spider Bite: “Can’t We Just Get a Divorce?”
- Annaliese G. Seidel, Colin G. Kaide
Radiology Case 1
- Priyanka Dube, Joshua K. Aalberg
Botulism: “I don’t need to talk, but I do need to swallow!”
- Daniel Z. Adams, Colin G. Kaide
Button Battery Ingestion: The Battery That Is Not as Cute as a Button
- Ashley Larrimore, Justin Carroll
Central Retinal Artery Occlusion with Sudden Vision Loss— “Ay, Ay, My Eye!”
- Bradley M. End, Colin G. Kaide
Cervical Fractures: Who Did Jefferson Bite?
- David Hartnett, Michael Barrie
Radiology Case 2
Cyanide poisoning— “i’m mr. blue…”.
- Jessica A. Everett, Colin G. Kaide, Hannah Hays
ECG Surprise Attack!: de Winter Aches and Pains
- Nicholas S. Fern, Amal Mattu
ECG Surprise Attack!: Chest Pain and the “Forgotten Lead”
Defibrillator malfunction: it’s electric boogie, woogie, woogie.
- Matthew Malone, Ashish Panchal
Radiology Case 3
Difficult airway and omg, there’s blood everywhere: navigating the difficult airway.
- Caitlin Rublee, Michael Barrie
Disseminated Neonatal Herpes Simplex Virus: Simplex Can Be Very Complex!
- Seth Linakis, Maegan Reynolds
Dural Venous Sinus Thrombosis: “ Not My Usual Migraine ”
- Rahul M. Rege, Brooke M. Moungey
Endocarditis: Osler’s Challenge
- Brit Long, Alex Koyfman
Editors and Affiliations
Colin G. Kaide, Christopher E. San Miguel
About the editors
Colin G. Kaide, MD, FACEP, FAAEM
Associate Professor of Emergency Medicine
Wexner Medical Center at the
Ohio State University
Columbus, OH
Christopher E. San Miguel, MD
Assistant Professor of Emergency Medicine
Bibliographic Information
Book Title : Case Studies in Emergency Medicine
Book Subtitle : LEARNing Rounds: Learn, Evaluate, Adopt, Right Now
Editors : Colin G. Kaide, Christopher E. San Miguel
DOI : https://doi.org/10.1007/978-3-030-22445-5
Publisher : Springer Cham
eBook Packages : Medicine , Medicine (R0)
Copyright Information : Springer Nature Switzerland AG 2020
Softcover ISBN : 978-3-030-22444-8 Published: 29 January 2020
eBook ISBN : 978-3-030-22445-5 Published: 14 November 2019
Edition Number : 1
Number of Pages : XXIII, 694
Number of Illustrations : 53 b/w illustrations, 118 illustrations in colour
Topics : Emergency Medicine
- Publish with us
Policies and ethics
- Find a journal
- Track your research
Clinical Practice and Cases in Emergency Medicine
CLINICAL PRACTICE AND CASES IN EMERGENCY MEDICINE INDEXED IN PUBMED AND PUBMED CENTRAL!
Click here for more info
CALL FOR REVIEWERS
Send your CV and letter of interest
Advertising
Click here for advertising opportunities!
- Volume 8, Issue 2, 2024
- Articles in Press
- Volume 8, Issue 1, 2024
- Volume 7, Issue 4, 2023
- Volume 7, Issue 3, 2023
- Volume 7, Issue 2, 2023
- Volume 7, Issue 1, 2023
- Volume 6, Issue 4, 2022
- Volume 6, Issue 3, 2022
- Volume 6, Issue 2, 2022
- Volume 6, Issue 1, 2022
- Volume 5, Issue 4, 2021
- Volume 5, Issue 3, 2021
- Volume 5, Issue 2, 2021
- Volume 5, Issue 1, 2021
- Volume 4, Issue 4, 2020
- Volume 4, Issue 3, 2020
- Volume 4, Issue 2, 2020
- Volume 4, Issue 1, 2020
- Volume 3, Issue 4, 2019
- Volume 3, Issue 3, 2019
- Volume 3, Issue 2, 2019
- Volume 3, Issue 1, 2019
- Volume 2, Issue 4, 2018
- Volume 2, Issue 3, 2018
- Volume 2, Issue 2, 2018
- Volume 2, Issue 1, 2018
- Volume 1, Issue 4, 2017
- Volume 1, Issue 3, 2017
- Volume 1, Issue 2, 2017
- Volume 1, Issue 1, 2017
Clinicopathological Cases from the University of Maryland
54-year-old woman with chest pain.
- Wynne, Zachary R. ;
- Hu, Kami M. ;
- Bontempo, Laura J. ;
- Gatz, J. David
Chest pain is a common presentation to the emergency department (ED) that can be caused by a multitude of etiologies. It can be challenging to differentiate life-threatening conditions from more benign causes. A 54-year-old woman presented to the ED complaining of chest pain with dyspnea in the setting of recent blunt trauma. This case offers a thorough yet practical approach to the diagnostic workup of chest pain with dyspnea in the ED setting. The surprising final diagnosis and case outcome are then revealed.
Case Series
Using point-of-care ultrasonography to diagnose traumatic arthrotomy of the knee: a case series.
- Mullings, Jordan ;
- Ashworth, Henry ;
- Kongkatong, Matthew ;
- Mantuani, Daniel
Case Series: Three patients in their early 20s presented to the ED complaining of knee trauma with wounds in proximity to the joint. Mechanisms of injury included a gunshot wound in one case and blunt trauma (motor vehicle collision and bicycle crash) in two cases. In all three cases TAK was suggested on POCUS examinations by the presence of intra-articular hyperechoic foci consistent with air artifact. All three cases had TAK confirmed by orthopedic evaluation.
Discussion: Ultrasound may have utility in the evaluation of patients presenting with knee trauma where TAK is a concern. The SLT is generally considered the gold standard test for diagnosis of TAK, but it is invasive and has a wide range of diagnostic accuracy. Intra-articular air has been found to be a sensitive marker for TAK in CT studies. Thus, additional investigations into the diagnostic accuracy of POCUS for this finding should be undertaken.
- 1 supplemental video
Case Reports
Defibrillator lead perforation leading to concerning electrocardiogram findings: case report.
- Rosenberg, Bryan ;
- Hockstein, Max ;
- Hadadi, Cyrus
Case Report: We report the case of a 71-year-old woman experiencing chest pain after an ICD placement two weeks earlier. On presentation, she exhibited ST-segment elevation on her ECG. Computed tomography confirmed ICD lead migration. The patient’s hemodynamics were normal, and she was discharged home after a five-day hospital stay following a lead revision.
Conclusion: Although rare, ICD lead perforation is a potential cause of chest pain and ischemic ECG changes. Emergency physicians should consider lead perforation as a potential differential diagnosis when evaluating chest pain in patients with ICDs, taking into account the potential complications of coronary angiography.
A Critical Combination of Esophageal Rupture and Upside-down Stomach: A Case Report
- Tipton, Kay Nicole ;
- Schroder, Daniel
Introduction: Spontaneous esophageal rupture, or Boerhaave syndrome, and upside-down stomach are rare pathologies associated with grave sequelae. Boerhaave syndrome can have a mortality rate as high as 44%. Upside-down stomach accounts for less than 5% of hiatal hernias and can lead to incarceration and volvulus.
Case Report: An 80-year-old woman presented to the emergency department with sudden onset, severe epigastric pain. Physical examination revealed normal vital signs with mild epigastric tenderness. Imaging obtained revealed a large hiatal hernia and findings concerning for esophageal perforation. The patient was started on 3.375 grams of intravenous piperacillin/tazobactam, and transfer to a tertiary care facility was initiated. After transfer, esophagography confirmed a perforation near the gastroesophageal junction and findings consistent with an upside-down stomach. The patient underwent successful repair of the esophageal perforation and gastropexy followed by intensive care unit admission and ultimately discharge.
Conclusion: Boerhaave syndrome and upside-down stomach are two conditions with high associated morbidity and mortality requiring prompt intervention. Information obtained in the history and physical examination including acute onset of chest pain after vomiting, tachypnea, subcutaneous emphysema, and hypoxia can assist in the diagnosis of the described pathologies. These signs and symptoms can be subtle on examination but are important in raising clinical suspicion for an otherwise rare etiology for acute onset chest pain.
Permissive Hypotension in a Patient with Severe Hypernatremia: A Case Report
- Hlady, Andrea ;
- Kerner, David ;
- Walker, Laura
Case Report: We present the case of a medically complex patient who had gradually worsening alteration of mental status and mean arterial pressures in the 50s on presentation to the emergency department.
Conclusion: Final diagnoses included severe hypernatremia and hypovolemic shock secondary to poor oral intake. We used judicious fluid repletion with gradual improvement in sodium levels and permissive hypotension to avoid rapid osmotic shifts. Balancing reperfusion and the risk for osmotic effects of aggressive fluid resuscitation can be a challenging situation for the multidisciplinary team.
Ruptured Ovarian Artery Aneurysm in a Postmenopausal Female: Case Report
- Patel, Raj ;
- Russell, Amy ;
- Randall, Melanie M.
Case Report: We present a case of a postmenopausal female presenting to the emergency department with flank pain. Point-of-care ultrasound showed free fluid in the abdomen. She was diagnosed with an ovarian artery aneurysm on computed tomography angiography and treated successfully with embolization.
Conclusion: Ruptured ovarian artery aneurysm is an uncommon cause of intra-abdominal hemorrhage in women.
Acute Abdominal Pain and a Whirlpool Sign on Computerized Tomography: A Case Report
- Libby, Christopher ;
- Stern, Evan ;
- Hoelle, Robyn
Case Report: We present a case of a 75-year-old female who presented with non-specific abdominal pain. The rare whirlpool sign on computed tomography identified a mesenteric volvulus as the cause of small bowel obstruction. She was taken to the operating room and, after successful resection of the small bowel, she recovered and ultimately was discharged home.
Conclusion: Early identification of a whirlpool sign and early surgical consultation are key to providing the best chance for salvage of ischemic small bowel due to mesenteric volvulus and to prevent a fatal outcome.
Emergency Department Doppler Assessment of a Central Retinal Artery Occlusion: Case Report
- McGuire, Duncan ;
- Calleja, Robert ;
- Pai, Eric ;
Introduction: Vision loss is a symptom found frequently in patients presenting to the emergency department (ED). Central retinal artery occlusion (CRAO) is an uncommon yet time-sensitive and critical cause of painless vision loss in which delayed diagnosis can lead to significant morbidity. Emergency medicine literature documents the ability to diagnose a CRAO using ultrasound by identifying the hyperechoic thrombus coined the retrobulbar spot sign.
Case Report: We present the case of a patient presenting with painless monocular vision loss for which CRAO was diagnosed in the ED using point-of-care ultrasound enhanced by the utilization of serial Doppler examinations as well as calculation of the central retinal artery resistive index.
Conclusion: Despite the pre-existing literature on point-of-care ultrasound investigation of central retinal artery occlusion, there are no emergency medicine case reports describing serial examination of the central retinal artery by spectral Doppler or calculation of arterial resistive index to improve this evaluation and monitor progression of the pathology. [2024;7(5)1–5.]
Transcatheter Arterial Embolization for Atraumatic Splenic Rupture in TEE-negative Endocarditis: A Case Report
- High, Daniel P. ;
- Acosta-Rullán, Jose M. ;
- Herrera, Danay ;
- Danckers, Mauricio ;
- Heller, Daniel ;
- Zapata, Daniel
Case Report: We present a case of a 56-year-old immunocompetent female with porcine bioprosthetic mitral valve replacement, automated implanted cardioverter-defibrillator, and atrial fibrillation on apixaban who was found to have in-hospital atraumatic splenic rupture complicating infective endocarditis with Haemophilus parainfluenza. The rupture was treated successfully by endovascular embolization. Usual treatment with six weeks of antibiotics provided durable cure without further complication, and no surgical intervention was needed for either the valve or spleen.
Conclusion: Transcatheter arterial embolization should be considered early in atraumatic splenic rupture. Relevant abdominal and cerebral imaging should be considered in all cases of suspected or confirmed infective endocarditis where unexplained symptoms are present.
Peritonsillar Abscess and Post-aspiration Bleed Identified with Point-of-care Ultrasound Using Endocavitary Probe: A Case Report
- Floyd, Jaclyn ;
- Dahl, Brandon ;
- Whited, Matthew ;
- Kurzweil, Ami
Case Report: A 19-year-old male presented to the ED with complaints of severe sore throat and fever for the prior five days. A POCUS using an endocavitary probe with sterile cover demonstrated hypoechoic debris with a “swirl sign.” Ultrasound was used to successfully guide needle aspiration by using in-plane needle guidance. The patient had significant bleeding after needle aspiration, and repeat POCUS clearly identified a new pocket of blood that had formed and was contained in the soft tissue. We monitored the size of the hematoma in real time with ultrasound to ensure the hematoma had no rapid expansion and was stable.
Conclusion: Among the differential diagnoses for sore throat, the diagnosis of peritonsillar abscess is particularly concerning as it is both common and generally requires swift intervention. Presentations can range from a mild infection to a life-threatening emergency with potential airway compromise. The two primary avenues for treatment include either needle aspiration or incision and drainage. Ultrasound can successfully identify the abscess and other landmarks for safe and successful drainage, as well as early identification of complications.
Diabetic Ketoalkalosis: A Case Report
- Brill, April ;
- Chheda, Nirav ;
- Strama, Daniel ;
- Soundarajan, Ramesh
Case Report: A 52-year-old female with a history of insulin-dependent diabetes mellitus type 2 presented to the ED with abdominal pain, nausea, and vomiting for three days. Her diagnostic workup revealed diabetic ketoacidosis but with concurrent metabolic alkalosis. Standard treatment for DKA was initiated, and there was improvement of her mentation and resolution of metabolic derangements.
Conclusion: Overlooking a diagnosis of DKA because of alkalosis on venous blood gas testing could lead to inappropriate treatment and, therefore, increased risk of morbidity and mortality in the affected patient.
Inferior Pancreaticoduodenal Artery Pseudoaneurysm Causing Biliary Obstruction: A Case Report
- Meloy, Patrick ;
- Lindquester, Will S. ;
- Stebbins, Jeffrey ;
- Bromberek, Elaine
Case Report: Here we present the case of a 64-year-old male patient with previous history of alcohol use disorder leading to chronic pancreatitis and prior embolization of an inferior pancreaticoduodenal pseudoaneurysm, who presented to the emergency department (ED) with abdominal pain, nausea, and vomiting, and was found to have a large recurrent inferior pancreaticoduodenal pseudoaneurysm with associated obstructive cholangitis and pancreatitis via contrast-enhanced computed tomography (CT) of the abdomen and pelvis. The patient was managed emergently by interventional radiology angiography with embolic coiling and percutaneous biliary catheter placement, and he subsequently underwent biliary duct stenting with gastroenterology. The patient was successfully discharged after a brief hospitalization after resolution of his pancreatitis and associated hyperbilirubinemia.
Conclusion: Pancreaticoduodenal artery aneurysms and pseudoaneurysms are rare and dangerous visceral pathologies. Patients can be diagnosed rapidly in the ED with CT imaging and need
Severely Painful and Pruritic Forearm Rash: A Case of Caterpillar Envenomation in South Florida
- Autrey, Cody M. ;
- Martinez, Stephanie A. ;
- Remaly, Michael ;
- Boccio, Eric
Case Report: We present the case of a patient presenting to the emergency department (ED) with acute-onset severe left forearm pain with associated pruritic rash incurred while working in a retail store. Initial therapeutic management included administration of analgesics, antihistamines, and steroids. After obtaining a comprehensive history and consulting with the Poison Control Center, we suspected an asp caterpillar envenomation. Following extraction of the caterpillar spines with silk tape, the patient’s symptoms improved. After a period of observation in the ED, the patient was discharged home without any known sequelae.
Conclusion: Although asp caterpillars typically inhabit trees and foliage, human exposure to the caterpillar may occur in developed environments. Effective history-taking, prompt communication with toxicologic experts, and complete removal of intact spines are essential for early identification and effective clinical management of asp caterpillar envenomation.
Use of Point-of-care Ultrasound to Diagnose Rectus Abdominis Strain in the Acute Setting: A Case Report
- Sanoja, Alejandro J. ;
- Shalaby, Michael
Case Report: We report a rare case of rectus abdominis muscle tear in an amateur bodybuilder diagnosed by point-of-care ultrasound (POCUS) in the emergency department (ED). The patient had presented to the ED three separate times after strenuous exercise, received costly diagnostic workups, and ultimately was diagnosed on the third visit with grade 2 bilateral rectus abdominis tear. The patient was given appropriate education and sports medicine follow-up. He underwent rehabilitation focused on trunk and core stability. At eight-week follow-up, the patient had made a full recovery.
Conclusion: To our knowledge, a case of bilateral rectus abdominis tear diagnosed by ultrasound in the emergency setting has not been previously published. Our case report highlights the utility of POCUS in diagnosing musculoskeletal pathology and preventing costly bounce-back visits.
Silicone Embolism Syndrome Causing Altered Mental Status and Respiratory Failure After an Unlicensed Gluteal Silicone Injection: A Case Report
- Lin, Christopher ;
- Robison, Jeremiah
Case Report: We describe a case in which a previously healthy, 28-year-old female presented with new-onset seizures and acute respiratory distress syndrome (ARDS) in the setting of a recent cosmetic procedure with silicone injections to the gluteal region. The patient’s hospital course was complicated by altered mental status, respiratory failure, rapid hemodynamic compromise, and eventual death.
Conclusion: In rare cases, one possible complication of cosmetic procedures is silicone embolism syndrome, which is characterized by pneumonitis, alveolar hemorrhage, and ARDS. The patient described in this report also experienced neurologic symptoms including seizure and altered mental status. This is a clinical diagnosis that relies upon thorough history-taking and detailed physical exam. Documentation on this phenomenon is limited, and medical management has not yet been standardized for this condition. Morbidity and mortality remain high.
Cardiac Arrest During a Ferric Derisomaltose Infusion Followed by Complete Heart Block: A Case Report
- Scott, Michael ;
- Jansen, Natalie ;
- Bilello, Leslie A.
Introduction: Ferric derisomaltose is the newest available parenteral iron formulation. Studies have demonstrated a good safety profile with improved tolerability compared to alternative parenteral iron formulations. To date there have been no reported acute, life-threatening cardiac events associated with ferric derisomaltose.
Case Report: An 86-year-old male who had previously tolerated routine iron infusions received a first dose of ferric derisomaltose at an outpatient infusion clinic. Six minutes into the infusion the patient became unresponsive with no palpable pulse. Return of spontaneous circulation was achieved after two minutes of chest compressions. Electrocardiogram showed complete heart block requiring transcutaneous pacing and vasopressor administration. The patient was transferred to the emergency department for stabilization and then admitted to the cardiac intensive care unit. During admission, the patient received a dual-chamber, permanent pacemaker without complication and was ultimately discharged.
Conclusion: It may be reasonable to consider parenteral iron as a toxicological etiology for patients presenting with complete heart block temporally associated with parenteral iron administration, particularly in patients with underlying conduction abnormalities.
When Educational Images Don’t Reflect the Population: Phlegmasia Cerulea Dolens, a Case Report
- Bornstein, Kasha ;
- LaRosa, Elizabeth ;
- Byrd, Kelsey ;
- Laney, Daniel ;
- Ferral, Hector ;
- Murphy-Lavoie, Heather
Introduction: Phlegmasia cerulea dolens (PCD) is an uncommon, potentially life-threatening complication of acute deep venous thromboses that requires a timely diagnosis. The name of the condition, the visual diagnostic criteria, and the preponderance of cases in the literature referencing findings exclusively in patients with lighter skin complexions means that PCD may not be on the differential diagnosis for the patient with more melanated skin who is experiencing this time-sensitive vascular emergency.
Case Report: We describe one case of PCD in a patient with darker skin complexion and the importance of identifying clinical findings, regardless of skin color, given the paucity of reference images for PCD in darker complected patients. Our literature review yielded 60 case reports for PCD. Only two papers included images referencing patients of color.
Conclusion: Accurate diagnosis requires recognition of diagnostic findings, which may vary significantly between phenotypically distinct populations. Many pathognomonic physical exam findings rely on descriptors based on presentation in phenotypically white patients.
Profound Alkalosis and Prolonged QT Interval Due to Inappropriate Gastrostomy Tube Loss: A Case Report
- Turner, Forrest ;
- Friedman, Brandon ;
- Meyers, H. Pendell ;
- Smith, Stephen W.
Introduction: Severe metabolic alkaloses are relatively rare but can carry a high mortality rate. Treatment involves supportive care and treatment of underlying causes.
Case Report: A 55-year-old male dependent on a gastrojejunostomy tube presented to the emergency department for altered mental status. The patient had metabolic alkalosis, electrolyte abnormalities, and prolonged QT interval on electrocardiogram. Examination and history revealed that chronic drainage of gastric fluid via malfunctioning a gastrojejunostomy tube resulted in profound alkalosis. The patient recovered with supportive care, electrolyte repletion, and gastrojejunostomy tube replacement.
Conclusion: This case highlights the importance of gastrointestinal acid-base pathophysiology.
Face-off Droop: A Case Report of Pediatric Stroke
- Robertson, Duncan ;
- Peirce, Hayden F. ;
- Nicpon, Marek D. ;
- Otterson, Eric M. ;
- O'Connor, Laurel ;
- Rissmiller, Julia G. ;
- Binder, Zachary W.
Introduction: Cerebrovascular accidents rarely occur in children; the incidence of ischemic stroke in patients <16 years of age is between 0.6–7.9/100,000. However, they are the fourth most common cause of acute neurological deficits in the pediatric population, and possible cases should be evaluated with a high index of suspicion to ensure timely intervention.
Case Report: We describe a previously healthy 17-year-old male who presented to the pediatric emergency department with a left facial droop and hemiparesis consistent with a stroke. The patient’s age and lack of comorbidities made this an extremely uncommon presentation. Our patient’s neurologic symptoms were believed to have been caused by a recent traumatic clavicular injury sustained two weeks prior, which subsequently led to vascular insult.
Conclusion: Cerebrovascular accidents are an important cause of morbidity and mortality in pediatric patients. Cerebrovascular accidents in children are most often secondary to congenital causes; however, care should be taken to assess for acquired causes, such as trauma to major blood vessels. While rarely implicated in traumatic injuries, arterial structures posterior to the medial clavicle can result in severe complications.
Images in Emergency Medicine
Clinical images in emergency medicine: cushing’s disease.
- Vadhan, Jason D. ;
- Hansen, Nathaniel ;
- Benitez, Fernando L. ;
- Velez, Larissa I.
Case Presentation: A 22-year-old female presented to the emergency department with a two-month history of worsening fatigue, unintentional weight gain, and progressive facial swelling. Physical examination findings included hirsutism, moon facies, and abdominal striae. Subsequent brain magnetic resonance imaging revealed the presence of a 2.4-centimeter pituitary macroadenoma, confirming the diagnosis of Cushing’s disease. The patient was then admitted for neurosurgical tumor resection.
Discussion: Cushing’s disease is exceedingly rare and often presents with symptoms resembling more prevalent disorders, contributing to delays in diagnosis. Therefore, maintaining a high index of suspicion for this disease is crucial for emergency physicians.
- 1 supplemental ZIP
Rash and Fever in a Returned Traveler
- Kons, Helena ;
- Herron, Elliott D. ;
- Pacheco, Zachary S. ;
- Shufflebarger, Erin F.
Discussion: Dengue is one of many viral illnesses that should be considered in returning travelers presenting with fever and other nonspecific symptoms. Emergency physicians must keep a broad differential when evaluating fever in returned travelers and prioritize history and physical exam findings to help narrow the diagnosis and provide appropriate management and supportive care while awaiting further confirmatory testing.
Atraumatic Orbital Emphysema in a Young Woman
- Albornoz, Eladio ;
- Wildemuth, Janet ;
- Valenzuela, Josephine
Discussion: Atraumatic orbital emphysema is a rare clinical condition more common in early middle-aged female patients with certain historical features such as chronic sinusitis, facial surgery or trauma, tobacco smoking, or current upper respiratory symptoms. While most cases will resolve spontaneously, rarely this condition can lead to vision-threatening orbital compartment syndrome, requiring lateral canthotomy or needle decompression.
One in a Million: A Woman Presenting with Unilateral Painful Ophthalmoplegia
- Bennett, Kevin ;
Case Presentation: A 52-year-old female presented to the emergency department with four days of right periorbital pain, ipsilateral temporal headache, diplopia, and photophobia. Physical examination of the right eye revealed painful ophthalmoplegia, cranial nerves III and VI paresis, increased intraocular pressure, and mild proptosis. Magnetic resonance venogram and magnetic resonance imaging orbits with contrast demonstrated an abnormal signal surrounding the right cavernous sinus/petrous apex. Tolosa-Hunt syndrome (THS) was diagnosed. Per neurology recommendations, the patient was placed on a steroid regimen over the course of three weeks. She was discharged on hospital day nine following resolution of symptoms. She had no recurrence of symptoms or residual deficits noted at her two-week follow-up appointment.
Discussion: With an estimated annual incidence of one case per million, THS is a sinister etiology of unilateral headache, painful ophthalmoplegia, and oculomotor palsy. Tolosa-Hunt syndrome is caused by granulomatous inflammation in the cavernous sinus and is highly responsive to corticosteroids. Magnetic resonance imaging studies of the cavernous sinus and orbital apex are highly sensitive for THS and characteristically show enlargement and focal-enhancing masses within the affected cavernous sinus.
Child with Closed Head Injury and Persistent Vomiting
- Khan, Abdullah
Case Presentation: We present the case of a six-year-old child with autism who presented with persistent vomiting in the setting of a closed head injury (CHI). Computed tomography of the head was normal, but due to persistent vomiting a radiograph of the abdomen was done, which showed multiple, rare-earth magnets in the abdomen. There was no history of witnessed ingestion. These magnets had caused enteroenteric fistula formation leading to persistent vomiting.
Discussion: In the setting of CHI, vomiting can be a sign of concussion or intracranial hemorrhage. In cases of CHI where intracranial pathology is ruled out and vomiting still persists, it is important to explore intra-abdominal causes of vomiting, especially in developmentally challenged children as they have higher incidence of unwitnessed foreign body ingestions.
CPC-EM Full-Text Issue
- Valenzi, Nicole
- Open access
- Published: 15 June 2020
Strategies to measure and improve emergency department performance: a scoping review
- Elizabeth E. Austin ORCID: orcid.org/0000-0002-8438-2362 1 ,
- Brette Blakely 1 ,
- Catalin Tufanaru 1 ,
- Amanda Selwood 1 ,
- Jeffrey Braithwaite 1 &
- Robyn Clay-Williams 1
Scandinavian Journal of Trauma, Resuscitation and Emergency Medicine volume 28 , Article number: 55 ( 2020 ) Cite this article
30k Accesses
29 Citations
8 Altmetric
Metrics details
Over the last two decades, Emergency Department (ED) crowding has become an increasingly common occurrence worldwide. Crowding is a complex and challenging issue that affects EDs’ capacity to provide safe, timely and quality care. This review aims to map the research evidence provided by reviews to improve ED performance.
Methods and findings
We performed a scoping review, searching Cochrane Database of Systematic Reviews, Scopus, EMBASE, CINAHL and PubMed (from inception to July 9, 2019; prospectively registered in Open Science Framework https://osf.io/gkq4t/ ). Eligibility criteria were: (1) review of primary research studies, published in English; (2) discusses a) how performance is measured in the ED, b) interventions used to improve ED performance and their characteristics, c) the role(s) of patients in improving ED performance, and d) the outcomes attributed to interventions used to improve ED performance; (3) focuses on a hospital ED context in any country or healthcare system. Pairs of reviewers independently screened studies’ titles, abstracts, and full-texts for inclusion according to pre-established criteria. Discrepancies were resolved via discussion. Independent reviewers extracted data using a tool specifically designed for the review. Pairs of independent reviewers explored the quality of included reviews using the Risk of Bias in Systematic Reviews tool. Narrative synthesis was performed on the 77 included reviews. Three reviews identified 202 individual indicators of ED performance. Seventy-four reviews reported 38 different interventions to improve ED performance: 27 interventions describing changes to practice and process (e.g., triage, care transitions, technology), and a further nine interventions describing changes to team composition (e.g., advanced nursing roles, scribes, pharmacy). Two reviews reported on two interventions addressing the role of patients in ED performance, supporting patients’ decisions and providing education. The outcomes attributed to interventions used to improve ED performance were categorised into five key domains: time, proportion, process, cost, and clinical outcomes. Few interventions reported outcomes across all five outcome domains.
Conclusions
ED performance measurement is complex, involving automated information technology mechanisms and manual data collection, reflecting the multifaceted nature of ED care. Interventions to improve ED performance address a broad range of ED processes and disciplines.
Introduction
Over the last two decades, Emergency Department (ED) crowding has become an increasingly common occurrence worldwide [ 1 ]. EDs must continue to provide care during periods of crowding, and respond to expected changes (e.g., seasonal increase in demand) and unexpected changes (e.g., unanticipated events and varying demand) [ 2 ]. However, crowding impedes ED staffs’ capacity to provide timely, safe and quality care. It extends the time patients spend in ED, and threatens patient outcomes [ 3 ].
Crowding in EDs is the product of input, throughput and output factors such as the volume of patients arriving to be seen, the time taken to assess and treat patients, and the availability of beds in hospital wards [ 4 ]. Interventions (e.g., decision-making structure, resource allocation, procedures) to address these factors have been widely implemented, with mixed results [ 5 , 6 , 7 , 8 ]. Identifying effective interventions known to have improved care can support the uptake of those interventions in different contexts. Understanding the characteristics of those interventions and their limitations can inform the development of new strategies to address common patient flow problems.
Ideally, the design and selection of performance measures should align with the system’s purpose and improvement strategy in order to identify the extent to which the system is working effectively. It is unsurprising then that input, throughput and output measures such as wait-time, length of stay and patient satisfaction have been used to report on EDs’ performance [ 4 , 9 ]. Understanding how ED performance has been measured in the past will support the selection of measures and inform the development of new measures to address gaps in performance knowledge.
The purpose of this scoping review was to map the research evidence provided by reviews on strategies to measure and improve ED performance. The review questions addressed were: (1) how is ED performance measured, (2) what are the interventions used to improve ED performance and (3) what is the role(s) of patients in improving ED performance, and (4) what are the outcomes attributed to interventions used to improve ED performance.
Study design
We conducted a scoping review of the literature from inception of bibliographic databases to July 2019 related to strategies to measure and improve ED performance. The study protocol was prospectively registered in December 2018 in the Open Science register ( https://osf.io/73r4t ). This protocol guided the review in adherence with the preferred reporting items for systematic reviews and meta-analyses statement (PRISMA) [ 10 ].
Inclusion criteria
Systematic reviews of primary research studies, reviews of reviews (umbrella reviews), and other research syntheses not fulfilling all criteria for systematic reviews published in the English-language peer-reviewed literature were included that met the following additional criteria: (1) review studies involving clinicians, patients, and/ or administrators in the ED or review studies that measure ED performance without involving participants (e.g., Length of Stay or patient mortality retrieved from aggregate hospital data); (2) discusses a) how performance is measured in the ED, b) interventions used to improve ED performance and their characteristics, c) the role(s) of patients in improving ED performance, and d) the outcomes attributed to interventions used to improve ED performance; (3) focuses on studies in a hospital ED context in any country or healthcare system.
Search strategy
To identify eligible studies, we developed a comprehensive search strategy using medical subject headings and text words for the general concepts of performance measures, interventions, and patient involvement. Cochrane Database of Systematic Reviews, Scopus, Embase, CINAHL and PubMed were searched on 14 January 2019. No date limits were used. English only publications were considered. An updated search was completed on 9 July 2019 and included a date filter (publications from 1 January 2019 to 31 December 2019). The full search strategy for all databases is shown in Appendix A (See Additional file 1 ).
An example, illustrating the search strategy for PubMed, is as follows:
((((emergency Service, Hospital [mh]) OR emergency department [tw])) AND (((((quality of health care [mh]) OR quality improvement [mh]) OR quality [tw]) OR improvement [tw]) OR performance [tw])) AND ((((((((review [ti]) OR systematic review [ti]) OR meta-analysis [ti]) OR meta-synthesis [ti]) OR scoping review [ti]) OR integrative review [ti]) OR overview [ti]) OR umbrella review [ti])
Study selection
The results of the searches were entered into EndNote citation management software (version 8.2; Thompson Reuters, New York, NY), and duplicates were removed. For each review, title, abstract, and full-text were independently screened by pairs of reviewers for inclusion according to pre-established criteria. Disagreements were resolved via discussion. Abstracts flagged as potentially relevant by reviewers underwent full-text review.
Data extraction and quality assessment
The data was extracted by independent reviewers by using an extraction tool specifically designed for the review. The data extraction form was piloted for usability prior to data extraction. The extraction form included information on Author(s), year of publication, country where review was conducted, type of review, review objectives and questions, number of studies included, types of intervention/s, intervention characteristics, type of measure used and/ or type of outcome measured.
The quality of the included papers was assessed using the Risk of Bias in Systematic Reviews (ROBIS) tool for assessing the risk of bias in systematic reviews [ 11 ]. The purpose of this assessment was only to allow for the quality of the included reviews to be mapped/ described. Prior to critical appraisal, the ROBIS was piloted on a sample of reviews. The quality of included reviews was explored by pairs of independent reviewers. Disagreements were resolved via discussion.
Data processing and analysis
A narrative synthesis was performed for this review, including numerical statistical summaries, textual commentaries, and tabular and graphical representations.
The combined searches yielded 4981 articles, including 1996 duplicate articles. Of these, 2985 abstracts and 134 full-texts were reviewed with 77 articles meeting inclusion criteria. Figure 1 illustrates the PRISMA diagram for the identification, screening, and inclusion processes.
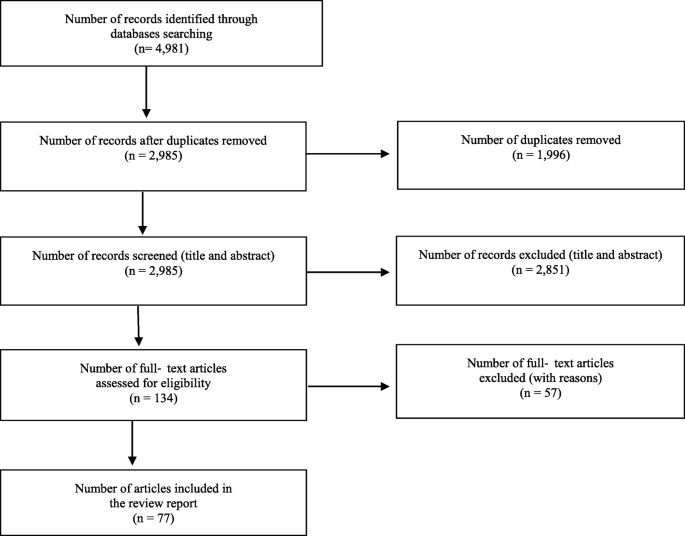
PRISMA flow diagram for study selection
An additional table outlines the characteristics of the included articles addressing ED performance measures (See Additional file 2 ). An additional table outlines the characteristics of the included articles addressing interventions, and patient role in ED performance (See Additional file 3 ). An additional table outlines the evidence contribution of the included reviews to each review question (See Additional file 4 ). Distribution of included reviews published per year (2000–2019) is provided in Fig. 2 . Figure 3 shows the distribution of locations where published reviews were conducted (based on the country affiliation of the first author).
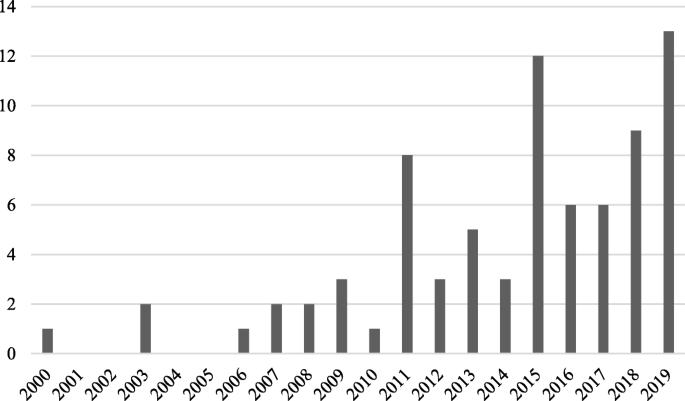
Distribution of published reviews over time
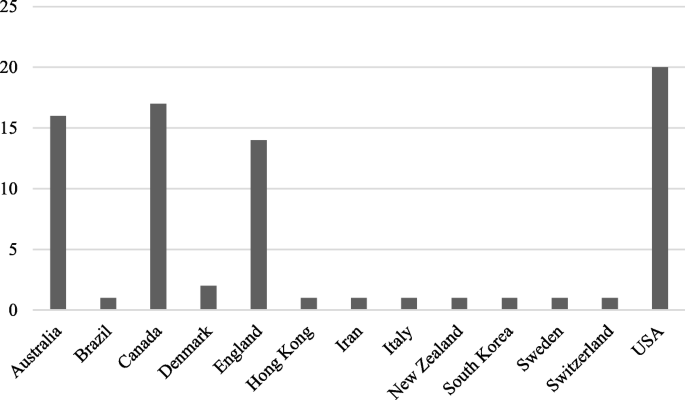
Distribution of published reviews by country affiliation of first author
Quality assessment
Using the ROBIS tool, 31 reviews were assessed as being low bias, 31 as high bias, and 15 as unclear bias. The ROBIS risk of bias assessment results for each domain and the overall risk of bias for individual reviews are presented in an additional file (See Additional file 5 ). Figure 4 displays a summary ROBIS assessment across all included reviews, graphically presenting the results of the ROBIS assessment for each domain and the overall rating.
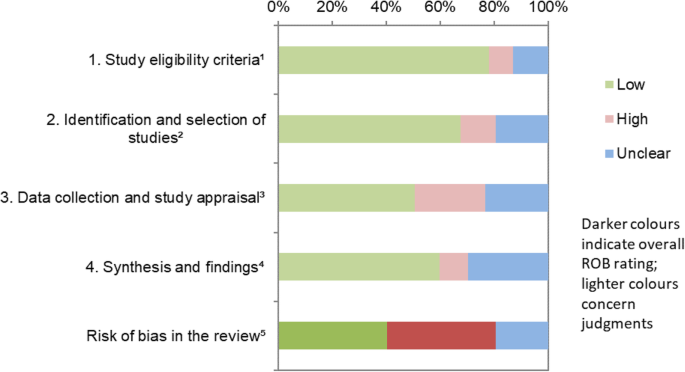
Graphical presentation for ROBIS results across all included reviews. 1 study eligibility criteria prespecified and appropriate for the review question. 2 sensitivity of the search. 3 rigour of the data collection process. 4 appropriateness of the synthesis for the review question. 5 overall risk of bias. “Low”, “high”, or “unclear” represents the rated level of concern about bias associated with each domain [ 11 ]
How ED performance is measured
Three reviews reported on ED performance measures [ 12 , 13 , 14 ]. Madsen (2015) extracted evidence for 202 individual indicators of ED performance from 127 articles, categorising them into process (e.g., time to diagnosis, physician workload), outcome (e.g., mortality, ambulance diversion), satisfaction (e.g., rate of complaints, patient participation in own care), structural/ organisational (e.g., admission rate, resources) and equity (e.g., weekday/weekend variation, sex, race, age) performance measures. Data sources used to generate the indicators are ED information technology, questionnaires, chart reviews, and multihospital databases [ 12 ]. Sørup (2013) identified 55 different performance measures and categorised ED performance measures into patient related measures focusing on safety (e.g., medication errors, unplanned reattendance), patient centeredness (e.g., complaints, left-without-being-seen), and satisfaction; employee related measures focusing on occupational profile (e.g., educational positions), and work environment; and operational performance focusing on planning (e.g., occupancy rate), utilisation (e.g., number of ECG’s taken, number of consultations), efficiency (e.g., ED admission transfer rate, length of stay), and time intervals (e.g., time to registration, triage, treatment). Stang (2015) examined crowding measures linked with quality of care including ED volume, number of patients in the waiting room, and ED length of stay.
Interventions used to improve ED performance and their characteristics
The remaining 74 articles addressed interventions used to improve ED performance. Interventions to improve ED performance address either practices and processes or team composition. Interventions addressing how tasks were performed in ED were identified as practice and process interventions. Interventions addressing the discipline or training of professionals practicing in ED were identified as team composition interventions.
Practices and processes
Six domains of clinical practice and processes have been targeted for interventions. They are: triage, care transitions, process re-design, point-of-care testing, observation units, and technology.
Designed to expedite care, triage processes sort patients according to urgency or type of service required [ 15 ]. Twelve reviews examined interventions relating to triage systems and processes. Triage based interventions included having a physician present [ 8 , 16 , 17 , 18 , 19 ] also called a triage liaison physician [ 20 ], a triage team consisting of at least 2 medical personnel (nurse or physician) [ 21 , 22 ], dedicated triage resources (e.g., ECG machine and ECG technician [ 23 ]), triage education [ 23 ], variations of basic triage [ 15 ], triage protocols [ 24 , 25 ], and nurse-led triage services [ 26 ]. A description of the characteristics for each type of triage intervention is provided in Table 1 .
Care transitions (handover processes)
Care transitions involved patient handover, which is the process of transferring accountability and responsibility for patient care to another person [ 27 ]. Seven reviews examined interventions relating to patient handover processes and transitions in care. Patient handover processes and transitions in care interventions include handover tools [ 27 , 28 , 29 , 30 ], bedside registration [ 19 , 31 ], discharge planning [ 31 ], discharge communication [ 32 ], process protocols and guidelines [ 27 , 29 , 30 ], handover training [ 29 ], dedicated offload nurse for triaging and assessing EMS patients [ 30 ], nurse discharge coordinators [ 33 ]. A description of the characteristics for each type of care transition intervention is provided in Table 2 .
- Process re-design
Process re-design refers to changes in how tasks are performed. Twenty-three reviews examined interventions relating to process re-design. Processes that have been re-designed included clinical guidelines and protocols [ 25 , 31 , 34 , 35 , 36 ], patient assignment and referral processes [ 4 , 31 , 36 , 37 , 38 ], organisational processes (e.g., communication, administration) [ 19 , 25 , 35 , 39 , 40 ], nurse-initiated care processes [ 8 , 17 , 21 , 41 , 42 , 43 , 44 ], clinical decision supports [ 45 , 46 , 47 ], and lean management/ lean thinking interventions [ 48 , 49 , 50 ]. A description of the characteristics for each type of process re-design intervention is provided in Table 3 .
- Point-of-care testing
Point-of-care testing refers to laboratory analysis located in the ED [ 8 , 21 ]. Five reviews examined point of care testing in ED [ 8 , 19 , 21 , 51 , 52 ]. Point-of-care testing has been used for a range of diagnostic tests including cardiac troponin [ 51 ], metabolic [ 19 ], urinalysis, pregnancy testing, cardiac markers, glucose [ 19 ], influenza, and respiratory syncytial virus [ 52 ].
- Observation units
Observation Unit interventions refer to ED-based observation units [ 31 ]. Twelve reviews examined observation units in ED [ 4 , 8 , 17 , 18 , 19 , 25 , 31 , 39 , 53 , 54 , 55 , 56 ]. ED based observation units have been developed for specific clinical needs such as Chest pain and Asthma [ 31 , 39 ], for specific processes such as assessment and procedures (e.g., Rapid Assessment Zones/ Pods) [ 18 , 55 ], medically stable patients likely to require admission (e.g., Medical Assessment Units) [ 4 , 8 , 17 ], or further investigations (e.g., Short Stay Units) [ 8 , 17 , 54 , 56 ], management for more than 4 h (e.g., ED managed Acute Care Unit) [ 19 ], or to manage referrals from GPs (e.g., Quick Diagnostic Units) [ 18 ]. A description of the characteristics for each type of process re-design intervention is provided in Table 4 .
Technology has been increasingly integrated into the ED [ 57 ]. Seven reviews examined interventions addressing technology in the ED. Technology has been introduced into EDs in the form of health information technology such as computerised clinical support systems (e.g., decision supports and provider entry forms) [ 45 , 58 ], mobile devices [ 57 ], and telecommunication technology [ 59 ], computer simulation [ 60 ], and eHealth records access [ 61 , 62 ]. A description of the characteristics for each type of technology intervention is provided in Table 5 .
Team composition interventions
Different roles and specialties have been integrated into the ED. These included advanced nursing roles, physiotherapy, general practitioners, scribes and physician assistants, pharmacy, and mental health services, as well as the development of professional skills.
Advanced Nursing Roles . Seven reviews examined interventions relating to advancing nursing roles in the ED. Advanced nursing interventions primarily include the nurse practitioner role [ 17 , 18 , 63 , 64 , 65 , 66 ] sometimes called advanced nurse practitioner/ advanced clinical practitioner/ advanced practice nurse [ 66 , 67 ], clinical nurse specialists [ 65 ], certified registered nurse anaesthetists [ 65 ], and Clinical Initiatives Nurse (CIN [ 17 , 68 ];. Advanced nursing roles typically require further education and require a minimum of 2 years emergency nursing experience [ 68 ]. A description of the characteristics for each type of advanced nursing role intervention is provided in Table 6 .
Physiotherapy
Three reviews examined interventions relating to physiotherapy roles in ED [ 69 , 70 , 71 ]. The role of physiotherapists in ED includes the assessment and management of acute and subacute musculoskeletal conditions, recent burns and diabetic wounds, provision of in-service training to other ED staff, liaising with nursing, medical, and allied health staff, and ensuring safe discharge from ED including arranging community services [ 69 , 70 , 71 ]. Physiotherapists have also been trained to read and request imaging and to prescribe a limited number of medications [ 69 , 70 ].
General practitioners
Two reviews examined interventions relating to general practitioner roles in ED [ 72 , 73 ]. There are different models in which general practitioners have been introduced into ED [ 72 , 73 ]. General practitioners have been used to staff non-urgent (rather than urgent) streams when patients are triaged into separate streams [ 72 , 73 ]. General practitioner services are also available onsite next to the ED and patients self-select or are redirected to these services from the ED. General practitioners have also been involved in the triage of patients presenting to the ED [ 72 , 73 ]. General practitioners have also been fully integrated into ED, providing care jointly with ED staff on a range of primary care and higher acuity emergency cases [ 72 , 73 ].
Scribes and physician assistants
Four reviews examined interventions relating to models of care using support staff such as scribes and physician assistant roles in ED [ 8 , 18 , 74 , 75 , 76 ]. A description of the characteristics for scribes and physician assistants interventions is provided in Table 7 .
Two reviews examined interventions relating to pharmacy roles in ED [ 77 , 78 ]. The scope of pharmacy roles in the ED varied. In the ED, pharmacists conduct consultations including interpreting results and providing pharmacotherapy recommendations [ 77 , 78 ]. ED pharmacy programs also included pharmacists tracking patients medication due times for repeat medications, completing medication histories, documenting patient body weight, height, and allergies [ 77 , 78 ]. Pharmacists have also been involved ED patient follow-up on culture and susceptibility results, adjusting or discontinuing therapy as needed [ 77 , 78 ].
Mental health services
Two reviews examined interventions relating to mental health services in ED [ 79 , 80 ] including Liaison Mental Health Services [ 79 , 80 ], co-located Psychiatry Liaison Personnel/ Spaces [ 80 ], Psychiatry Specialist Services [ 80 ]. A description of the characteristics for each type of mental health services intervention is provided in Table 8 .
Professional development
Nine reviews examined professional development interventions in ED. Professional development interventions included eight-hour customer service training related to applying industry customer service principles to health care, benchmarks, and taught customer service skills such as negotiating agreement and resolution of expectations [ 31 , 39 ]; and a 10 week medical Spanish language course [ 39 ]. The provision of audit/ feedback (from a supervisor/ colleague/ external coder) on clinical practice has been implemented in a variety of formats including weekly case specific, every 6 weeks individual feedback with group discussion; or individual feedback provided via email, written, verbal, electronic, and combination of media, one on one, group, (e.g., patient outcomes, quality of documentation [ 81 , 82 , 83 ]. Other interventions include cross-training nurses to care for patients in a designated area [ 25 ], monthly staff education/ workshops about hand hygiene with elements of targeted feedback [ 84 ], and clinical education to improve nurses’ and medical staffs’ knowledge of pain management through an education program [ 42 , 85 ].
The role(s) of patients in improving ED performance
Patients are consumers of healthcare services provided by EDs. The delivery of healthcare depends on the relationship between clinicians and patients and the degree to which patients play an active or passive role [ 86 ]. Two reviews examined the role of patients in improving ED performance [ 42 , 86 ]. Patients’ role in improving ED performance has been primarily addressed by involving patients in shared decision making. Shared decision-making involves active patient involvement with the clinician, sharing information and collaboratively taking steps to reach agreement about which treatment to implement [ 86 ]. Shared decision making has been addressed through decision supports [ 86 ], and education [ 42 ]. A description of the characteristics for each type of patient role intervention is provided in Table 9 .
The outcomes attributed to interventions used to improve ED performance
The outcomes attributed to interventions used to improve ED performance identified by the review can be categorised into five key areas: Time, proportion, process, cost, and clinical outcomes. Time-based measures record time stamps/ intervals, and sub-cycle intervals [ 25 ]. Measures of time intervals varied, however, the most commonly used were length of stay (LOS) in ED and waiting time. Proportion-based measures record elements of ED performance rates [ 25 ]. Measures of proportion-based measures varied widely and included admissions, resource use, and treatment follow-up rate. Process-based measures document elements of ED process performance [ 25 ]. Direct and indirect measures of quality of care, including left without being seen, did not wait, as well as patient and provider satisfaction, were commonly reported ED process performance measures. Cost-based measures indicate the financial implications of health care provided. Measures of cost varied and lacked detail, and were often reported simply as “costs” [ 18 , 51 , 62 ]. Clinical-based measures indicate the medical outcomes for patients of the health care provided. Measures of clinical outcomes reported varied, however, and the most commonly used were adverse events and readmission.
Overall, time-based and process-based outcome domains were the most widely used measures for interventions with 24 out of the 30 individual interventions reporting at least one of each of these domains. Proportion-based outcomes were similarly well reported on for interventions with 21 out of the 30 interventions reporting proportion-based measures. Cost-based and clinical-based outcomes were the least utilised domains with only 12 and 17 interventions respectively reporting at least one outcome in these domains.
Team composition
The time-based outcome was the most widely used domain for team composition interventions, with 10 of the 13 interventions reporting at least one time-based measure. Proportion-based measures were reported for nine of the 13 interventions with process-based and clinical-based measures reported for 8 of the interventions. Cost-based outcomes were the least utilised, with six interventions reporting at least one outcome in this domain. An additional file provides a full list of intervention performance measures reported for the included interventions (See Additional file 6 ). Figure 5 displays a summary of the types of interventions within practices and processes and team composition, as well as graphically presenting the proportion of the total number of outcome measures reported for each domain for each intervention.
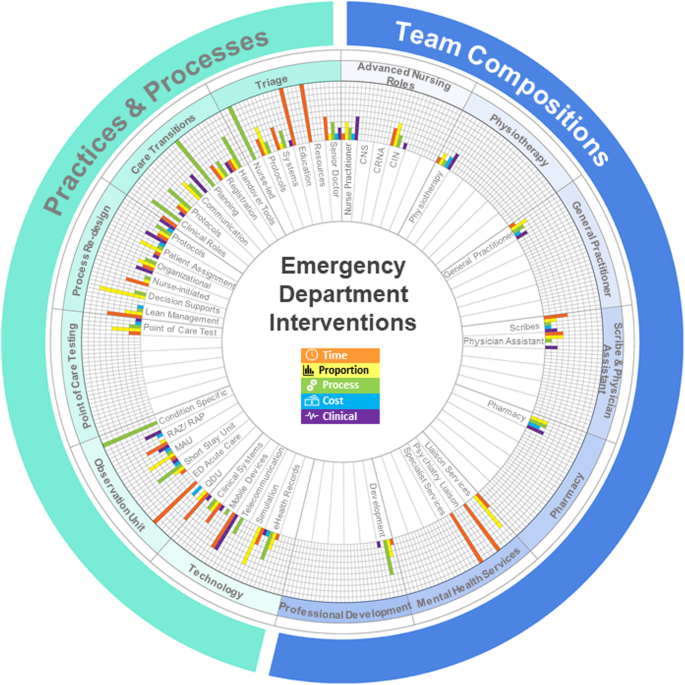
Overview of the outcome measures used for ED interventions. The rich picture summarises the types of interventions identified by this review. The graphs for each intervention present the proportion of outcome measures reported for each domain for each intervention. Each proportion was calculated as the number of identified outcome measures in the domain divided by the total number of outcome measures for the intervention. CNS, clinical nurse specialist; CRNA, certified registered nurse anaesthetist; CIN, clinical initiatives nurse; RAZ/RAP, rapid assessment zone/ rapid assessment pod; MAU, medical assessment unit; ED, Emergency Department; QDU, quick diagnosis unit
In this review we aimed to map the research evidence of strategies to measure and improve ED performance. There was strong alignment between how ED performance is measured, the types of ED interventions implemented, and the outcome measures used to assess effectiveness of those interventions.
While EDs worldwide may share a common purpose [ 87 , 88 , 89 ], the differences and complexity within each ED system is reflected in the vast number of measures used to understand different aspects of ED performance. Similarly, the different ways these measures have been categorised reflects differences in the interpretation of that common purpose. For EDs and the communities they serve, the selection of performance measures is critical to ensuring a comprehensive, accurate and precise picture of ED performance is developed. It is equally important to develop a shared understanding how ED performance data is collected to ensure that measures used for performance assessment or comparison are valid.
The results of our review show that the delivery of care in ED has evolved over the last 20 years with the implementation of a wide range of interventions to improve ED performance. The interventions identified by this review address very specific aspects of how care is provided in ED, suggesting that a systems perspective has not been applied. Crucially, EDs are complex adaptive systems and any intervention implemented to improve performance is likely influenced by existing models of care, as well as a variety of contextual factors such as funding, availability of skilled workforce, and the physical space available.
Changing patient involvement in the provision of care also plays a role in ED performance. The small number of reviews identified by this review that involved patient perspectives suggests that care delivery in the ED is likely driven by clinicians and protocols, with patients as passive consumers of care. In the crowded and frantic ED context, achieving patient-centred care is likely a challenging task [ 33 ]. Our findings suggest that achieving active participation by patients in ED care delivery is possible, but more research is needed on the implications for ED performance and patients’ clinical and psychosocial outcomes.
Intervention outcome measures allow us to determine if the intervention to improve ED performance was successful or if it had unintended outcomes. While the use of all five types of outcome measures synthesised in our review would provide clinicians, hospital administrators and researchers with the most insight into ED performance and intervention effectiveness, implementation of the full suite of measures may not be possible in some contexts. Most studies reported the use of three or fewer types of outcome measures. Measures of time were commonly combined with proportion or process measures. The use of time, proportion and process measures provides insight into the speed of healthcare provision, the quantity of resources used (e.g., diagnostic tests), and the quality of patient management (e.g., clinical documentation). However, intervention implementation decisions are often made based on department budgets or the availability of funding. As such, the inclusion of cost measures is increasingly important to inform clinicians’ and administrators’ decisions about ED performance and intervention effectiveness. Finally, measures of clinical outcomes are also important for examining the assumption that system changes in healthcare provide improved patient safety and clinical outcomes, and this is a neglected area for many interventions.
Limitations
This scoping review is the first, to our knowledge, to synthesise the many review articles to comprehensively describe the different strategies that have been used to measure and improve ED performance. Limitations of the current study include our pragmatic choice to only include reviews published in English and the potential biases of the included studies. The published reviews examining the effectiveness of interventions in the ED context might have suffered from publication bias, with negative results less likely to be published. As a result of this publication bias, it is unclear what interventions are unsuccessful or if particular context characteristics result in unsuccessful interventions, or negatively impact on patient care.
Over the last two decades, the way care has been delivered in ED has changed dramatically in response to increased demand and increasing complexity, and it is likely that it will continue to change over the next two decades. In turn, the way we measure ED performance has changed with our capacity to collect and analyse data. We need to think critically about the performance measures we use to define ED performance to ensure we are capturing a complete and dynamic picture that accurately reflects how an ED is performing. As shown by this review, a number of different strategies have been used to improve ED performance. As both internal and external pressures on ED continue to grow, future intervention initiatives will be needed to ensure the tragic consequences of crowding in ED are avoided. Crucially, a comprehensive range of meaningful outcome measures for interventions needs to be used to accurately establish the effectiveness of ED interventions and inform system changes and decision-making.
Availability of data and materials
All data generated or analysed during this study are included in this published article and its supplementary information files.
Di Somma S, Paladino L, Vaughan L, Lalle I, Magrini L, Magnanti M. Overcrowding in emergency department: an international issue. Intern Emerg Med. 2015;10(2):171–5.
Article PubMed Google Scholar
Braithwaite J, Wears RL, Hollnagel E. Resilient health care: turning patient safety on its head. International J Qual Health Care. 2015;27(5):418–20.
Article Google Scholar
Miró O, Antonio MT, Jiménez S, De Dios A, Sánchez M, Borrás A, et al. Decreased health care quality associated with emergency department overcrowding. Eur J Emerg Med. 1999;6(2):105–7.
Hoot NR, Aronsky D. Systematic review of emergency department crowding: causes, effects, and solutions. Ann Emerg Med. 2008;52(2):126–136.e1.
Handel DA, Ma OJ, Workman J, Fu R. Impact of an expeditor on emergency department patient throughput. West J Emerg Med. 2011;12(2):198–203.
PubMed PubMed Central Google Scholar
Shetty A, Gunja N, Byth K, Vukasovic M. Senior streaming assessment further evaluation after triage zone: a novel model of care encompassing various emergency department throughput measures. EMA - Emerg Med Australas. 2012;24(4):374–82.
Karpas A, Finkelstein M, Reid S. Parental preference for rehydration method for children in the emergency department. Pediatr Emerg Care. 2009;25(5):301–6.
De Freitas L, Goodacre S, O’Hara R, Thokala P, Hariharan S. Interventions to improve patient flow in emergency departments: an umbrella review. Emerg Med J. 2018;35(10):626–37.
Schull MJ, Guttmann A, Leaver CA, Vermeulen M, Hatcher CM, Rowe BH, et al. Prioritizing performance measurement for emergency department care: consensus on evidencebased quality of care indicators. Can J Emerg Med. 2011;13(5):300–9.
Google Scholar
Moher D, Liberati A, Tetzlaff J, Altman DG. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. J Clin Epidemiol. 2009;62(10):1006–12.
Whiting P, Savovi J, Higgins JPT, Caldwell DM, Reeves BC, Shea B, et al. ROBIS: a new tool to assess risk of bias in systematic reviews was developed. J Clin Epidemiol. 2016;69:225–34.
Article PubMed PubMed Central Google Scholar
Madsen M, Kiuru S, Castrèn M, Kurland L. The level of evidence for emergency department performance indicators: systematic review. Eur J Emerg Med. 2015;22(5):298–305.
Sørup CM, Jacobsen P, Forberg JL. Evaluation of emergency department performance - a systematic review on recommended performance and quality-in-care measures. Scand J Trauma Resusc Emerg Med. 2013;21(1):62.
Stang AS, Crotts J, Johnson DW, Hartling L, Guttmann A. Crowding measures associated with the quality of emergency department care: a systematic review. Acad Emerg Med. 2015;22(6):643–56.
Harding KE, Taylor NF, Leggat SG. Do triage systems in healthcare improve patient flow? A systematic review of the literature. Aust Health Rev. 2011;35(3):371–83.
Abdulwahid MA, Booth A, Kuczawski M, Mason SM. The impact of senior doctor assessment at triage on emergency department performance measures: systematic review and meta-analysis of comparative studies. Emerg Med J. 2016;33(7):504–13.
Elder E, Johnston ANB, Crilly J. Review article: systematic review of three key strategies designed to improve patient flow through the emergency department. EMA - Emerg Med Australas. 2015;27(5):394–404.
Wylie K, Crilly J, Toloo G, Fitzgerald G, Burke J, Williams G, et al. Review article: emergency department models of care in the context of care quality and cost: a systematic review. EMA - Emerg Med Australas. 2015;27(2):95–101.
Morley C, Unwin M, Peterson GM, Stankovich J, Kinsman L. Emergency department crowding: a systematic review of causes, consequences and solutions. PLoS One. 2018;13(8):e0203316.
Article PubMed PubMed Central CAS Google Scholar
Rowe BH, Guo X, Villa-Roel C, Schull M, Holroyd B, Bullard M, et al. The role of triage liaison physicians on mitigating overcrowding in emergency departments: a systematic review. Acad Emerg Med. 2011;18(2):111–20.
Oredsson S, Jonsson H, Rognes J, Lind L, Göransson KE, Ehrenberg A, et al. A systematic review of triage-related interventions to improve patient flow in emergency departments. Scand J Trauma Resusc Emerg Med. 2011;19(1):43.
Ming T, Lai A, Lau PM. Can team triage improve patient flow in the emergency department? A systematic review and meta-analysis. Adv Emerg Nurs J. 2016;38(3):233–50.
Chhabra S, Eagles D, Kwok ESH, Perry JJ. Interventions to reduce emergency department door-to- electrocardiogram times: a systematic review. CJEM. 2019;21(5):607–17.
Robinson DJ. An integrative review: triage protocols and the effect on ED length of stay. J Emerg Nurs. 2013;39(4):398–408.
McCaughey D, Erwin CO, DelliFraine JL. Improving capacity management in the emergency department: a review of the literature, 2000-2012. J Healthc Manag. 2015;60(1):63–75.
PubMed Google Scholar
Rehman SA, Ali PA. A review of factors affecting patient satisfaction with nurse led triage in emergency departments. Int Emerg Nurs. 2016;29:38–44.
Dawson S, King L, Grantham H. Review article: improving the hospital clinical handover between paramedics and emergency department staff in the deteriorating patient. EMA - Emerg Med Australas. 2013;25(5):393–405.
Alimenti D, Buydos S, Cunliffe L, Hunt A. Improving perceptions of patient safety through standardizing handoffs from the emergency department to the inpatient setting: a systematic review. J Am Assoc Nurse Pract. 2019;31(6):354–63.
Flynn D, Francis R, Robalino S, Lally J, Snooks H, Rodgers H, et al. A review of enhanced paramedic roles during and after hospital handover of stroke, myocardial infarction and trauma patients. BMC Emerg Med. 2016;17(1):5.
Reay G, Norris JM, Nowell L, Hayden KA, Yokom K, Lang ES, et al. Transition in Care from EMS providers to emergency department nurses: a systematic review. Prehosp Emerg Care. 2020; 24(3):421–33.
Boudreaux ED, Cruz BL, Baumann BM. The use of performance improvement methods to enhance emergency department patient satisfaction in the United States: a critical review of the literature and suggestions for future research. Acad Emerg Med. 2006;13(7):795–802.
Curran JA, Gallant AJ, Zemek R, Newton AS, Jabbour M, Chorney J, et al. Discharge communication practices in pediatric emergency care: a systematic review and narrative synthesis. Syst Rev. 2019;8(1):83.
Shankar KN, Bhatia BK, Schuur JD. Toward patient-centered care: a systematic review of older adults’ views of quality emergency care. Ann Emerg Med. 2014;63(5):529–50.
Mieiro DB, de Oliveira ÉBC, da Fonseca REP, Mininel VA, Zem-Mascarenhas SH, Machado RC. Strategies to minimize medication errors in emergency units: an integrative review. Rev Bras Enferm. 2019;72:307–14.
Juillard CJ, Mock C, Goosen J, Joshipura M, Civil I. Establishing the evidence base for trauma quality improvement: a collaborative WHO-IATSIC review. World J Surg. 2009;33(5):1075–86.
Kirkland SW, Soleimani A, Rowe BH, Newton AS. A systematic review examining the impact of redirecting low-acuity patients seeking emergency department care: is the juice worth the squeeze? Emerg Med J. 2019;36(2):97–106.
Hughes JM, Freiermuth CE, Shepherd-Banigan M, Ragsdale L, Eucker SA, Goldstein K, et al. Emergency department interventions for older adults: a systematic review. J Am Geriatr Soc. 2019;67(7):1516–25.
Kumar GS, Klein R. Effectiveness of case management strategies in reducing emergency department visits in frequent user patient populations: a systematic review. J Emerg Med. 2013;44(3):717–29.
Boudreaux ED, O’Hea EL. Patient satisfaction in the emergency department: a review of the literature and implications for practice. J Emerg Med. 2004;26(1):13–26.
Jones P, Schimanski K. The four hour target to reduce emergency department “waiting time”: a systematic review of clinical outcomes. EMA - Emerg Med Australas. 2010;22(5):391–8.
Cabilan CJ, Boyde M. A systematic review of the impact of nurse-initiated medications in the emergency department. Australas Emerg Nurs J. 2017;20(2):53–62.
Article CAS PubMed Google Scholar
Williams S, Keogh S, Douglas C. Improving paediatric pain management in the emergency department: an integrative literature review. Int J Nurs Stud. 2019;94:9–20.
Considine J, Shaban RZ, Curtis K, Fry M. Effectiveness of nurse-initiated X-ray for emergency department patients with distal limb injuries. Eur J Emerg Med. 2019;26(5):314–22.
Rowe BH, Villa-Roel C, Guo X, Bullard MJ, Ospina M, Vandermeer B, et al. The role of triage nurse ordering on mitigating overcrowding in emergency departments: a systematic review. Acad Emerg Med. 2011;18(12):1349–57.
Bennett P, Hardiker NR. The use of computerized clinical decision support systems in emergency care: a substantive review of the literature. J Am Med Inform Assoc. 2017;24(3):655–68.
Deblois S, Chartrand-Lefebvre C, Toporowicz K, Chen Z, Lepanto L. Interventions to reduce the overuse of imaging for pulmonary embolism: a systematic review. J Hosp Med. 2018;13(1):52–61.
Desai S, Liu C, Kirkland SW, Krebs LD, Keto-Lambert D, Rowe BH. Effectiveness of implementing evidence-based interventions to reduce C-spine image ordering in the emergency department: a systematic review. Acad Emerg Med. 2018;25(6):672–83.
Bucci S, De Belvis AG, Marventano S, De Leva AC, Tanzariello M, Specchia ML, et al. Emergency department crowding and hospital bed shortage: is lean a smart answer? A systematic review. Eur Rev Med Pharmacol Sci. 2016;20(20):4209–19.
CAS PubMed Google Scholar
Holden RJ. Lean thinking in emergency departments: a critical review. Ann Emerg Med. 2011 Mar 1;57(3):265–78.
Isfahani HM, Tourani S, Seyedin H. Features and results of conducted studies using a lean management approach in emergency Department in Hospital: a systematic review. Bull Emerg Trauma. 2019;7(1):9.
Bingisser R, Cairns C, Christ M, Hausfater P, Lindahl B, Mair J, et al. Cardiac troponin: a critical review of the case for point-of-care testing in the ED. Am J Emerg Med. 2012;30(8):1639–49.
Doan Q, Enarson P, Kissoon N, Klassen TP, Johnson DW. Rapid viral diagnosis for acute febrile respiratory illness in children in the emergency department. Cochrane Database Syst Rev. 2014;(9):CD006452. https://doi.org/10.1002/14651858.CD006452.pub4 .
Goodacre SW. Should we establish chest pain observation units in the UK? A systemic review and critical appraisal of the literature. J Accid Emerg Med. 2000;17(1):1–6.
Article CAS PubMed PubMed Central Google Scholar
Konnyu KJ, Kwok E, Skidmore B, Moher D. The effectiveness and safety of emergency department short stay units: a rapid review. Open Med. 2012;6(1):e10.
Bullard MJ, Villa-Roel C, Guo X, Holroyd BR, Innes G, Schull MJ, et al. The role of a rapid assessment zone/pod on reducing overcrowding in emergency departments: a systematic review. Emerg Med J. 2012;29(5):372–8.
Galipeau J, Pussegoda K, Stevens A, Brehaut JC, Curran J, Forster AJ, et al. Effectiveness and safety of short-stay units in the emergency department: a systematic review. Acad Emerg Med. 2015;22(8):893–907.
Dexheimer JW, Borycki EM. Use of mobile devices in the emergency department: a scoping review. Health Informatics J. 2015;21(4):306–15.
Georgiou A, Prgomet M, Paoloni R, Creswick N, Hordern A, Walter S, et al. The effect of computerized provider order entry systems on clinical care and work processes in emergency departments: a systematic review of the quantitative literature. Ann Emerg Med. 2013;61(6):644–53.
Kelton DK, Szulewski A, Howes D. Real-time video telemedicine applications in the emergency department: a scoping review of literature. Can J Emerg Med. 2018;20(6):920–8.
Mohiuddin S, Busby J, Savović J, Richards A, Northstone K, Hollingworth W, et al. Patient flow within UK emergency departments: a systematic review of the use of computer simulation modelling methods. BMJ Open. 2017;7(5):e015007.
Bowden T, Coiera E. The role and benefits of accessing primary care patient records during unscheduled care: a systematic review. BMC Med Inform Decis Mak. 2017;17(1):138.
Hersh WR, Totten AM, Eden KB, Devine B, Gorman P, Kassakian SZ, et al. Outcomes from health information exchange: systematic review and future research needs. JMIR Med Informatics. 2015;3(4):e39.
Carter AJE, Chochinov AH. A systematic review of the impact of nurse practitioners on cost, quality of care, satisfaction and wait times in the emergency department. Can J Emerg Med. 2007;9(4):286–95.
Jennings N, Clifford S, Fox AR, O’Connell J, Gardner G. The impact of nurse practitioner services on cost, quality of care, satisfaction and waiting times in the emergency department: a systematic review. Int J Nurs Stud. 2015;52(1):421–35.
Kleinpell RM, Ely EW, Grabenkort R. Nurse practitioners and physician assistants in the intensive care unit: an evidence-based review. Crit Care Med. 2008;36(10):2888–97.
Thamm C, Teleni L, Chan RJ, Stone L, Mccarthy AL. Nurse-led interventions for cancer patients in emergency departments: systematic review. Collegian. 2019;26(2):311–9.
Williams K. Advanced practitioners in emergency care: a literature review. Emerg Nurse. 2017;25(4):36–41.
Innes K, Jackson D, Plummer V, Elliott D. Care of patients in emergency department waiting rooms - an integrative review. J Adv Nurs. 2015;71(12):2702–14.
Anaf S, Sheppard LA. Physiotherapy as a clinical service in emergency departments: a narrative review. Physiotherapy. 2007;93(4):243–52.
Ferreira GE, Traeger AC, Maher CG. Review article: a scoping review of physiotherapists in the adult emergency department. Emerg Med Australas. 2019;31(1):43–57.
Kilner E. What evidence is there that a physiotherapy service in the emergency department improves health outcomes? A systematic review. J Health Serv Res Policy. 2011;16(1):51–8.
Gonçalves-Bradley D, Khangura JK, Flodgren G, Perera R, Rowe BH, Shepperd S. Primary care professionals providing non-urgent care in hospital emergency departments. Cochrane Database Syst Rev. 2018;(2):CD002097. https://doi.org/10.1002/14651858.CD002097.pub4 .
Ramlakhan S, Mason S, O’Keeffe C, Ramtahal A, Ablard S. Primary care services located with EDs: a review of effectiveness. Emerg Med J. 2016;33(7):495–503.
Cabilan CJ, Eley RM. Review article: potential of medical scribes to allay the burden of documentation and enhance efficiency in Australian emergency departments. Emerg Med Australas. 2015;27(6):507–11.
Doan Q, Sabhaney V, Kissoon N, Sheps S, Singer J. A systematic review: the role and impact of the physician assistant in the emergency department. Emerg Med Australas. 2011;23(1):7–15.
Heaton HA, Castaneda-Guarderas A, Trotter ER, Erwin PJ, Bellolio MF. Effect of scribes on patient throughput, revenue, and patient and provider satisfaction: a systematic review and meta-analysis. Am J Emerg Med. 2016;34(10):2018–28.
Cohen V, Jellinek SP, Hatch A, Motov S. Effect of clinical pharmacists on care in the emergency department: a systematic review. Am J Heal Pharm. 2009;66(15):1353–61.
Hammond DA, Gurnani PK, Flannery AH, Smetana KS, Westrick JC, Lat I, et al. Scoping review of interventions associated with cost avoidance able to be performed in the intensive care unit and emergency department. Pharmacother J Hum Pharmacol Drug Ther. 2019;39(3):215–31.
Callaghan P, Eales S, Coates T, Bowers L. A review of research on the structure, process and outcome of liaison mental health services. J Psychiatr Ment Health Nurs. 2003;10(2):155–65.
Evans R, Connell J, Ablard S, Rimmer M, O’Keeffe C, Mason S. The impact of different liaison psychiatry models on the emergency department: a systematic review of the international evidence. J Psychosom Res. 2019;119:53–64.
Lavoie CF, Schachter H, Stewart AT, McGowan J. Does outcome feedback make you a better emergency physician? A systematic review and research framework proposal. Can J Emerg Med. 2009;11(6):545–52.
Rogers RLG, Narvaez Y, Venkatesh AK, Fleischman W, Hall MK, Taylor RA, et al. Improving emergency physician performance using audit and feedback: a systematic review. Am J Emerg Med. 2015;33(10):1505–14.
Lorenzetti DL, Quan H, Lucyk K, Cunningham C, Hennessy D, Jiang J, et al. Strategies for improving physician documentation in the emergency department: a systematic review. BMC Emerg Med. 2018;18(1):36.
Seo HJ, Sohng KY, Chang SO, Chaung SK, Won JS, Choi MJ. Interventions to improve hand hygiene compliance in emergency departments: a systematic review. J Hosp Infect. 2019;102(4):394–406.
Sampson FC, Goodacre SW, O’Cathain A. Interventions to improve the management of pain in emergency departments: systematic review and narrative synthesis. Emerg Med J. 2014;31:e9–18.
Flynn D, Knoedler MA, Hess EP, Murad MH, Erwin PJ, Montori VM, et al. Engaging patients in health care decisions in the emergency department through shared decision-making: a systematic review. Acad Emerg Med. 2012;19(8):959–67.
Fleischmann T, Fulde G. Emergency medicine in modern Europe. Emerg Med Australas. 2007;19(4):300–2.
Black JJM, Davies GD. International EMS systems: United Kingdom. Resuscitation. 2005;64(1):21–9.
Morganti KG, Bauhoff S, Blanchard JC, Abir M, Iyer N, Smith A, et al. The evolving role of emergency departments in the United States. Rand Heal Q. 2013;3(2):3.
Download references
Acknowledgements
We would like to acknowledge and thank Ms. Teresa Winata for providing support in the proof-reading process. We would also like to acknowledge and thank Mr. Drew McTavish for providing support in the development of Figures.
This project was not funded.
Author information
Authors and affiliations.
Australian Institute of Health Innovation, Macquarie University, Sydney, Australia
Elizabeth E. Austin, Brette Blakely, Catalin Tufanaru, Amanda Selwood, Jeffrey Braithwaite & Robyn Clay-Williams
You can also search for this author in PubMed Google Scholar
Contributions
EEA, BB, JB and RCW made substantial contributions to the conception of the work. EEA, CT and AS made substantial contributions to the acquisition, analysis and interpretation of the data. All authors approved the submitted version and have agreed both to be personally accountable for the author’s own contributions and to ensure that questions related to the accuracy or integrity of any part of the work, even ones in which the author was not personally involved, are appropriately investigated, resolved, and the resolution documented in the literature.
Corresponding author
Correspondence to Elizabeth E. Austin .
Ethics declarations
Ethics approval and consent to participate.
Not applicable.
Consent for publication
Competing interests.
The authors declare that they have no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Additional file 1: appendix a..
The full search strategy for all databases.
Additional file 2: Table 1.
Characteristics of the included reviews on ED performance measures.
Additional file 3: Table 2.
Characteristics of the included reviews on interventions to improve ED performance.
Additional file 4: Table 3.
The evidence contribution to the review questions of the included reviews.
Additional file 5: Table 4.
The ROBIS Risk of Bias results for each domain and the overall risk of bias for the included reviews
Additional file 6: Table 14.
The performance measures reported by the included reviews for each intervention.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Austin, E.E., Blakely, B., Tufanaru, C. et al. Strategies to measure and improve emergency department performance: a scoping review. Scand J Trauma Resusc Emerg Med 28 , 55 (2020). https://doi.org/10.1186/s13049-020-00749-2
Download citation
Received : 18 March 2020
Accepted : 27 May 2020
Published : 15 June 2020
DOI : https://doi.org/10.1186/s13049-020-00749-2
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Length of stay
- Patient satisfaction
Scandinavian Journal of Trauma, Resuscitation and Emergency Medicine
ISSN: 1757-7241
- Submission enquiries: Access here and click Contact Us
- General enquiries: [email protected]

- PubMed Central / WestJEM
- PubMed WestJem Abstracts
- eScholarship PDF Repository
- Physicians News Network
- Interactive Issue/ISSUU
- ISSUU Download Instructions
- Medscape WestJEM
- COVID-19 Articles
- Current Issue: Volume 25 Issue 2
- Electronic Publication in Press
- Past Issues
- CDEM CORD Special Issues in Education
- CORD Abstracts
- MEMC Abstracts
- Focus Category
- Article Category
- Current Issue Volume 8 Issue 1
- Why WestJEM?
- WestJEM Submissions
- CPC-EM Submissions
- WestJEM Submission Guidelines
- CPC-EM Submission Guidelines
- CDEM/CORD Submission Guidelines
- Submission Conditions for Acceptance
- Photo Consent Form
- Conflicts of Interest
- Statement On Informed Consent
- Statement on Human and Animal Rights
- Manuscript Veracity
- Malpractice and Ethics
- Retraction Guidelines
- Copyright/Errata
- CPC Emergency Medicine
- Concise Academic Writing
- Reviewer Requirements
- Reviewer Instructions
- Review Examples
- Section Editor Requirements
- Section Editor Instructions
- Peer Review Training Module
- About WestJEM
- WestJEM Niche
- Journal History
- Journal Facts
- Editors and Editorial Board
- Top Section Editors & Reviewers
- American College of Osteopathic Emergency Physicians
- California ACEP
- California Chapter of AAEM
- UC Irvine Health School of Medicine
- Subscribers
- Press Releases
- Academic Job Board
- Advertising

Latest Manuscripts

The EM Cases Summaries are succinct, written, easily navigable, key point reports of each main episode podcast , authored by Our Team that you can download to your smartphone or tablet to reference and read at the bedside or at your leisure automatic download via dropbox.

Download individual pdf EM Cases Summaries
By clicking on the category and then episode title below, all summaries.
Episode 194 Subarachnoid Hemorrhage Recognition, Workup, Diagnosis with Jeff Perry & Katie Lin
Episode 193 Life Threatening Asthma with Leeor Sommer & Sameer Mal
Episode 192 Asthma Management – 5 Step Approach with Leeor Sommer & Sameer Mal
Episode 191 Future of EM – Systems Thinking with Alecs Chochinov & David Petrie
Episode 190 Carpal Bone Injuries with Arun Sayal & Matt Distefano
Episode 189 Wrist Injuries with Arun Sayal & Matt Distefano
Episode 188 Hemoptysis with Bourke Tillmann & Scott Weingart
Episode 187 Crashing Analphylaxis & AMAX4 Algorithm with Ben McKenzie
Episode 186 Traumatic Dental Emergencies with Chris Nash & Richard Ngo
Episode 185 Atraumatic Dental Emergencies with Chris Nash & Richard Ngo
Episode 184 Drug Interactions with David Juurlink & Walter Himmel
Episode 183 PID & Genital Lesions with Catherine Varner & Robyn Shafer
Episode 182 STIs: Cervicitis, Vulvovaginitis, Urethritis with Catherine Varner & Robyn Shafer
Episode 181 CVT, IIH, GCA, Peripartum Headache with Roy Baskind & Amit Shah
Episode 180 Acetaminophen Poisoning with Emily Austin & Margaret Thompson
Episode 179 Specific Hand Injuries with Matt Distenfano and Arun Sayal
Episode 177 Bronchiolitis Diagnostic Challenges & Management with Suzanne Schuh
Episode 176 Orthopedic X-rays Pitfalls with Arun Sayal & Yatin Chadha
Episode 175 Orthopedic Differential: SCARED OF Mnemonic with Arun Sayal & Yatin Chadha
Episode 174 Traumatic Pneumothorax – Is Less More? with Mathieu Toulouse
Episode 173 Febrile Infant with Brett Burstein & Gary Joubert
Episode 172 Syncope Simplified with David Carr
Episode 170 Part 2 Cardiac Arrest Controversies: PoCUS, Communication, ECPR, Termination with Bourke Tillmann, Scott Weingart, Sara Gray & Rob Simard
Episode 169 Part 1 Cardiac Arrest Controversies with Bourke Tillmann, Scott Weingart, Sara Gray & Rob Simard
Episode 167 Myocarditis with Paul Dorian & Walter Himmel
Episode 166 Pericarditis & Cardiac Tamponade with Paul Dorian & Walter Himmel
Episode 164 Part 2 Acute Heart Failure: Cardiogenic Shock Simplified with Tarlan Hedayati & Bourke Tillmann
Episode 163 Part 1 Acute Heart Failure with Tarlan Hedayati & Bourke Tillmann
Episode 161 Red Flag Headaches: Cervical Artery Dissection with Amit Shah & Roy Baskind
Episode 160 Part 2 Geriatric Trauma with Barbara Haas, Bourke Tillmann & Camilla Wong
Episode 159 Part 1 Geriatric Trauma with Barbara Haas, Bourke Tillmann & Camilla Wong
Episode 158 Management of Spontaneous Pneumothorax with Gil Yehudaiff & Mehdi Tahiri
Episode 157 Neuromuscular Diseases with George Porfiris & Roy Baskind
Episode 156 Approach to Acute Motor Weakness with George Porfiris & Roy Baskind
Episode 155 Part 2 Bradycardia: Treatment of Bradycardia & Bradydysrhythmias with Paul Dorian & Tarlan Hedayati
Episode 154 Part 1 Bradycardia: Approach to Bradycardia with Paul Dorian & Tarlan Hedayati
Episode 153 Pediatric Minor Head Injury & Concussion with Sarah Reid & Roger Zemek
Episode 152 Massive Hemorrhage Protocols with Jeannie Callum, Andrew Petrosoniak & Barabara Haas
Episode 151 Part 2 AKI: ED Management with Ed Etchells & Bourke Tillmann
Episode 150 Part 1 AKI: A Simple ED Approach & Rhabdomyolysis with Ed Etchells & Bourke Tillmann
Episode 149 Part 2 Liver Emergencies: Thrombosis & Bleeding, PVT, SBP, Paracentesis with Walter Himmel & Brian Steinhart
Episode 148 Part 1 Liver Emergencies: HE, HRS, Liver Tests, Drugs to Avoid with Walter Himmel & Brian Steinhart
Episode 147 Part 2 Diabetic Emergencies: HHS Recognition & ED Management with Melanie Baimel, Leeor Sommer & Bourke Tillmann
Episode 146 Part 1 Diabetic Emergencies: DKA Recognition & ED Management with Melanie Baimel, Leeor Sommer & Bourke Tillmann
Episode 145 Physician Compassion with Barbara Tatham
Episode 144 Part 2 Urologic Emergencies: Testicular Torsion with Natalie Wolpert & Yonah Krakowsky
Episode 143 Part 1 Urologic Emergencies: Priapism & Urinary Retention with Natalie Wolpert & Yonah Krakowsky
Episode 142 Neonatal Resuscitation with Hilary Whyte, Jabeen Fayyaz & Emily MacNeil
Episode 140 Part 4 COVID-19: Protected Intubation with George Kovacs
Episode 139 Part 3 COVID-19: PPE, Conservation Strategies & Protected Code Blue with Laurie Mazurik
Episode 138 Part 2 COVID-19: Surge Capacity Strategies with Daniel Kollek
Episode 137 Part 1 COVID-19: Screening, Diagnosis & Management with Andrew Morris & Howard Ovens
Episode 136 Part 2 Shoulder Injuries: Occult Injuries & Proximal Humerus Fractures with Arun Sayal & Dale Dantzer
Episode 135 Part 1 Shoulder Injuries: Approach & Dislocations with Arun Sayal & Dale Dantzer
Episode 133 Status Epilepticus with Paul Koblic & Aylin Reid
Episode 132 Approach to Resolved Seizure with Paul Koblic & Aylin Reid
Episode 131 PEA arrest & PseudoPEA with Rob Simard & Scott Weingart
Episode 130 Community Acquired Pneumonia with Leeor Sommer and Andrew Morris
Episode 129 ED Overcrowding & Access Block with Grant Innes, Howard Ovens & Sam Campbell
Episode 128 Low Risk Chest Pain & High Sensitivity Troponin with Andrew McRae & Eddy Lang
Episode 127 Part 2 Drugs that Work & Drugs that Don’t: Antiemetics etc with Joel Lexchin & Justin Morgenstern
Episode 126 Part 1 Drugs that Work & Drugs that Don’t: Analgesics etc with Joel Lexchin & Justin Morgenstern
Episode 125 Electrical Injuries with Joel Fish, Maria Invankovic
Episode 124 Burn & Inhalation Injuries with Joel Fish, Maria Invankovic & George Kovacs
Episode 123 Pediatric UTI Myths and Misperceptions with Olivia Ostrow & Michelle Science
Episode 122 Sepsis & Septic Shock with Sara Gray
Episode 121 Elbow Injuries Pitfalls with Arun Sayal & Dale Dantzer
Episode 120 Stroke Management in the Age of Endovascular Therapy with Walter Himmel & David Dushenski
Episode 119 Part 2 Trauma – The 1st & Last 15 Mintures with Kylie Bosman, Chris Hicks & Andrew Petrosoniak
Episode 118 Part 1 Trauma – The 1st & Last 15 Minutes with Kylie Bosman, Chris Hicks & Andrew Petrosoniak
Episode 117 TIA update with Walter Himmel & David Dushenski
Episode 116 Opioid Misuse, Overdose & Withdrawal with Aaron Orkin, Michelle Klaiman & Kathryn Dong
Episode 115 Agitated Patient with Reuben Strayer & Margaret Thompson
Episode 114 Part 2 PE Challenges in Diagnosis: Imaging, PE in Pregnancy, Subsegmental PE with Eddy Lang & Kerstin DeWit
Episode 113 Part 1 PE Challenges in Diagnosis with Eddy Lang & Kerstin DeWit
Episode 112 Tachydysrhythmias with Amal Mattu & Paul Dorion
Episode 111 Effective Learning Strategies in EM with Jonathan Sherbino & Rick Penciner
Episode 110 Airway Pitfalls with Scott Weingart
Episode 109 Skin & Soft Tissue Infections with Andrew Morris & Melanie Baimel
Episode 108 Pediatric Physical Abuse with Carmen Coombs & Alyson Holland
Episode 107 Blunt Ocular Trauma with Anna MacDonald
Episode 106 Toxic Alcohols – Minding the Gaps with Margaret Thompson & Emily Austin
Episode 105 Commonly Missed Ankle Injuries with Arun Sayal & Hossein Mehdian
Episode 104 ICH – The Golden Hour with Walter Himmel & Scott Weingart
Episode 103 Preventing Burnout & Promoting Wellness in EM with Sara Gray & Chris Trevelyan
Episode 102 Part 2 GI Bleed with Anand Swaminathan & Salim Rezaie
Episode 101 Part 1 GI Bleed with Anand Swaminathan, Salim Rezaie & Jeannie Callum
Episode 100 Disaster Medicine with Laurie Mazurik, Daniel Kollek & Joshua Bezanson
Episode 99 Highlights from EMU 2017: Lyme, signover, patient complaints & vertigo with Chris Hicks, Walter Himmel, Matt Poyner & Leeor Sommer
Episode 98 Teaching on Shift with Amal Mattu & Rick Penciner
Episode 97 EM Literature Review 2016 with Joel Yaphe, Jason Fischer & Justin Morgenstern
Episode 96 Cardiac Arrest Care beyond ACLS live from EMU 2017 with Jordan Chenkin
Episode 95 Pediatric Polytrauma with Sue Beno & Fuad Alnaji
Episode 94 UTI Myths & Misconceptions with Andrew Morris & Justin Morgenstern
Episode 93 PALS Guidelines with Allan DeCaen & Anthony Crocco
Episode 92 Aortic Dissection from EM Cases Course with Anton Helman & David Carr
Episode 91 Occult Knee Injuries with Arun Sayal & Hossein Mehdian
Episode 90 Low & Slow Poisoning with Margaret Thompson & Emily Austin
Episode 89 Part 2 DOACs: Bleeding & Reversal with Walter Himmel, Ben Bell & Jim Douketis
Episode 88 Part 1 DOACs: Use & Misuse, DVT & Afib with Walter Himmel, Ben Bell & Jim Douketis
Episode 87 Alcohol Withdrawal & Delrium Tremens with Sara Gray, Bjug Borgundvaag and Mel Kahan
Episode 86 Emergency Management of Hyperkalemia with Melanie Baimel & Ed Etchells
Episode 85 Medical Clearance of Psychiatric Patients with Howard Ovens, Brian Steinhart & Ian Dawe
Episode 84 Congenital Heart Disease Emergencies with Gary Joubert & Ashley Strobel
Episode 83 Critical Care Controveries from SMACC with Mark Forrest, Chris Hicks, Chris Nickson & Scott Weingart
Episode 82 Radiology Controversies with Walter Himmel & Ryan Margau
Episode 81 EM Literature Review with Joel Yaphe
Episode 80 Presentation Skills with Eric Letovsky & Rick Penciner
Episode 79 Pediatric Asthma with Sanjay Mehta and Dennis Scolnik
Episode 78 Anaphylaxis & Anaphylactic Shock with David Carr from the EM Cases Course
Episode 77 Fever in the Returning Traveler with Nananin Meshkat & Matthew Muller
Episode 76 Pediatric Procedural Sedation with Amy Drendel
Episode 75 Part 2 Diagnostic Decision Making in EM with Walter Himmel, Chris Hicks & David Dushenski
Episode 74 Opioid Misuse in EM with David Juurlink & Re uben Strayer
Episode 73 Pediatric Seizure & Status Epilepticus with Angelo Mikrogianakis & Lawrence Richer
Episode 72 Part 2 ACLS Guidelines 2015: Post Arrest Care with Laurie Morrison, Steve Lin & Scott Weingart
Episode 71 Part 1 ACLS Guidelines 2015: Cardiac Arrest with Laurie Morrison & Steve Lin
Episode 70 End of Life Care in EM with Howard Ovens, Shona MacLachlan & Paul Miller
Episode 69 Obesity Emergency Management with Rich Levitan, David Barbic & Andrew Sloas
Episode 68 Sickle Cell Disease with John Foote & Richard Ward
Episode 67 Pediatric Pain Management with Anthony Crocco & Samina Ali
Episode 66 Backboard and Collar Nightmares from EMU Conference with Kylie Bosman
Episode 65 IV Iron for Anemia in EM with Walter Himmel, Jeannie Callum & Yulia Lin
Episode 64 Part 2 Highlights from Update in EM Conference Whistler 2015 with David Carr & Chris Hicks
Episode 63 Pediatric DKA with Sarah Reid & Sarah Curtis
Episode 62 Part 1 Diagnostic Decision Making in EM with Walter Himmel, Chris Hicks & David Dushenski
Episode 61 Part 1 Highlights from Update in EM Conference Whistler 2015 with Joel Yaphe, Paul Hannam & Anil Chopra
Episode 60 Emergency Management of Hyponatremia with Melanie Baimel & Edward Etchells
Episode 59 Bronchiolitis with Sanjay Mehta & Dennis Scolnik
Episode 58 Tendons & Ligaments: Commonly Missed Uncommon Orthopaedic Injuries with Ivy Cheng & Hossein Mehdian
Episode 56 Stiell Sessions – Clinical Decision Rules & Risk Scales with Ian Stiell & Hans Rosenberg
Episode 55 Part 2 Weingart Himmel Sessions – Fluids in Sepsis & Post-Intubation Sedation with Scott Weingart & Walter Himmel
Episode 54 Part 1 Weingart Himmel Sessions – Preoxygenation & DSI with Walter Himmel & Scott Weingart
Episode 53 Part 3 Pediatric POCUS: Appendicitis & Intussusception with Adam Sivitz & Alex Arroyo
Episode 53 Part 2 Pediatric POCUS: Lung with Alyssa Abo
Episode 53 Part 1 Pediatric POCUS: Nerve Blocks with Jason Fischer
Episode 52 Commonly Missed Uncommon Orthopedic Injuries with Ivy Cheng & Hossein Mehdian
Episode 51 Managing Difficult Patients with Walter Himmel, Jean Pierre Champagne & Ann Shook
Episod e 50 Recognition & Management of Pediatric Sepsis & Septic Shock with Gina Neto & Sarah Reid
Episode 49 Effective Patient Communication, Patient Centered Care & Patient Satisfaction with Walter Himmel, Jean Pierre Champagne & Ann Shook
Episode 48 Pediatric Fever Without a Source with Sarah Reid & Gina Neto
Episode 47 Evidence Based Medicine with Walter Himmel
Episode 46 Social Media in Emergency Medicine Learning with Rob Rogers, Ken Milne & Brent Thoma
Episode 45 Swadron on Vertigo, Mattu on Cardiology Literature from EM Update Conference 2014 with Stuart Swadron & Amal Mattu with Joel Yaphe, Lisa Thurgur & David Carr
Episode 43 Appendicitis Controversies with David Dushenski & Brian Steinhart
Episode 42 Mesenteric Ischemia & Pancreatitis with David Dushenski & Brian Steinhart
Episode 41 Hypertensive Emergencies with Joel Yaphe & Clare Atzema
Episode 40 Asymptomatic Hypertension with Joel Yaphe & Clare Atzema
Episode 39 Update in Trauma Literature with Dave MacKinnon & Mike Brzozowski
Episode 38 ENT Emergencies with Leeor Sommer & Maria Ivankovic
Episode 37 Anticoagulants, PCCs & Platelets with Walter Himmel, Katerina Pavenski & Jeannie Callum
Episode 36 Transfustions, Anticoagulants & Bleeding with Walter Himmel, Katerina Pavenski & Jeannie Callum
Episode 35 Pediatric Orthopedic Emergencies with Sanjay Mehta & Jonathan Pirie
Episode 34 Geriatric Emergency Medicine with Don Melady & Jaques Lee
Episode 33 Oncologic Emergencies with John Foote & Joel Yaphe
Episode 32 Whistler’s Update in Emergency Medicine Conference 2013
Episode 31 Part 2 Procedures: Lumbar Puncture, Spontaneous Pneumothorax & Ultrasound-Guided Fracture Reduction with Jordan Chenkin & Jamie Blicker
Episode 30 Part 1 Procedures: Central Lines, Surgical Airways & Pericardiocentesis with Jordan Chenkin & Jamie Blicker
Episode 29 Hand Emergencies with Andrew Arcand & Laura Tate
Episode 28 Aortic Dissection, Acute Limb Ischemia & Compartment Syndrome with David Carr & Anil Chopra
Episode 27 Drugs of Abuse – Stimulants & Opiates with Margaret Thompson & Lisa Thurgur
Episode 26 Low Back Pain Emergencies with Walter Himmel & Brian Steinhart
Episode 25 Pediatric & Adult Syncope with Anna Jarvis & Eric Letovsky
Episode 24 COPD & Pneumonia with Anil Chopra & John Foote
Episode 23 Vaginal Bleeding in Early Pregnancy with Ross Claybo & Dave Dushenski
Episode 22 Whistler’s Update in Emergency Medicine Conference 2012
Episode 21 Pulmonary Embolism with John Foote & Anil Chopra
Episode 20 Atrial Fibrillation with Clare Atzema, Nazanin Meshkat & Bryan Au
Episode 19 Part 2 Pediatric Abdominal Pain: Gastroenteritis, Constipation & Bowel Obstruction with Anna Jarvis & Stephen Freedman
Episode 19 Part 1 Pediatric Abdominal Pain: Approach & Appendicitis with Anna Jarvis & Stephen Freedman
Episode 18 Part 2 POCUS: More Point of Care Ultrasound with Jordan Chenkin, Greg Hall, Jason Fischer & Paul Hannam
Episode 18 Part 1 POCUS: Pearls, Pitfalls & Controversies with Jordan Chenkin, Greg Hall, Jason Fischer & Paul Hannam
Episode 17 Part 2 Stroke: Dabigitran & Intracranial Hemorrhage with Walter Himmel & Dan Selchen
Episode 17 Part 1 Stroke: Emergency Stroke Controversies with Walter Himmel & Dan Selchen
Episode 16 Acute Monoarthritis with Joel Yaphe & Indy Ghosh
Episode 15 Part 2 Acute Coronary Syndromes: Management with Eric Letovsky, Mark Mensour & Neil Fam
Episode 15 Part 1 Acute Coronary Syndromes: Risk Stratification with Eric Letovsky, Mark Mensour & Neil Fam
Episode 14 Part 2 Headache: Thunderclap Headache – Cervical Artery Dissection & Cerebral Venous Thrombosis with Anil Chopra & Stella Yiu
Episode 14 Part 1 Headache: Migraine Headache & Subarachnoid Hemorrhage with Anil Chopra & Stella Yiu
Episode 13 Killer Coma Cases with Brian Steinhart & David Carr
Episode 12 ACLS Guidelines with Steven Brooks & Michael Feldman
Episode 11 Cognitive Decision Making & Medical Error with Doug Sinclair & Chris Hicks
Episode 10 Trauma Pearls & Pifalls with Dave MacKinnon & Mike Brzozowski
Episode 9 Nontraumatic Eye Emergencies with Simon Kinsgley & George Porfiris
Episode 8 Emergency Airway Controversies with Jonathan Sherbino, Mark Mensour & Andrew Healy
Episode 7 Medical & Surgical Emergencies in Pregnancy with Dave Dushenski & Shirley Lee
Episode 6 Transient Ischemic Attack with Walter Himmel & Dan Selchen
Episode 5 Renal Colic, Toxicology Update & Body Packers with Lisa Thurgur & Paul Rosenberg
Episode 4 Acute Congestive Heart Failure with Brian Steinhart & Eric Letovsky
Episode 3 Pediatric Head Injury with Rahim Valani & Jen Riley
Episode 2 Excited Delirium with Margaret Thompson & Dan Cass
Episode 1 Occult Fractures & Dislocation with Arun Sayal & Natalie Mamen
Cardiovascular
Gastroenterology, genitourinary, hematology & oncology.
Episode 132 Approach to Resolved Seizure with Paul Koblic & Aylin Reid
Episode 14 Part 2 Headaches: Thunderclap Headache – Cervical Artery Dissection & Cerebral Venous Thrombosis with Anil Chopra & Stella Yiu
Episode 14 Part 1 Headaches: Migraine & Subarachnoid Hemorrhage with Anil Chopra & Stella Yiu
Ophthalmology
Orthopedics.
Episode 136 Part 2 Shoulder Injuries: Occult Injuries & Humerus Fractures with Arun Sayal & Dale Dantzer
Episode 50 Recognition & Management of Pediatric Sepsis & Septic Shock with Gina Neto & Sarah Reid
Respirology
Resuscitation, special populations.
Episode 74 Opioid Misuse in EM with David Juurlink & Reuben Strayer
Support EM Cases
Subscribe to, our newsletter.
Unlock exclusive free content and resources by subscribing to our newsletter now!

Search form
Emergency department crowding hits crisis levels, risking patient safety.

(© stock.adobe.com)
In a pair of new studies, Yale researchers document a widespread and increasing level of overcrowding in America’s emergency departments (EDs), a crisis that puts patient safety and access to care at risk.
For the studies, the researchers examined, respectively, the progression in recent years of two measures of ED function and hospital capacity: boarding time — or how long patients remain in the ED after physicians have determined they should be admitted to the hospital — and how often patients leave the ED before receiving care.
Their findings, they say, help characterize the bigger issues that underlie ED crowding. And they show that the issue worsened during the COVID-19 pandemic. Their methods also yield more timely assessments of these key indicators, which historically have been hard to come by.
“ This is not an ED management issue,” said Arjun Venkatesh , an associate professor of emergency medicine at Yale School of Medicine and an author of the studies. “These are indicators of overwhelmed resources and symptoms of deeper problems in the health care system.”
The studies were both published Sept. 30 in JAMA Network Open.
It was during the 1980s that ED crowding emerged as an issue of national concern. The problem has only gotten worse in the decades since, with negative effects for patients and hospital staff alike. For patients, studies have found that ED crowding is correlated with discomfort, reduced privacy, treatment delays, and higher risk of prolonged disease and death. ED crowding also leads to increased violence toward staff, greater clinician and nurse turnover, and high rates of burnout. A recent study found nearly 63% of surveyed U.S. physicians experienced burnout in 2021.
In one of the new studies , researchers found that boarding times — or the amount of time patients were kept in the emergency department after clinicians had determined they should be admitted — were related to hospital occupancy rates, or the percentage of staffed inpatient beds that are occupied. The Joint Commission, an independent national health care accrediting body, has recommended that boarding time not exceed four hours.
For the study, Yale researchers evaluated these measures in U.S. hospitals during the COVID-19 pandemic, from January 2020 to December 2021. They found that when occupancy exceeded 85%, boarding times exceeded this four-hour standard. In fact, under those circumstances, the median ED boarding time was 6.58 hours. Boarding times also worsened throughout this time period, outpacing occupancy rates.
This relationship makes sense, says Alexander Janke, lead author of the studies, because when occupancy is high, there are few available beds to move patients from the ED. And with diminishing capacity, wait times are compounded.
“ Hospitals must have some flexible capacity so there are places for patients with emergencies requiring hospitalization to go,” said Janke, who conducted the research while a fellow at Yale School of Medicine and is now at the University of Michigan. “And that capacity doesn’t exist in a lot of places.” Which means patients stay in the ED until space opens at their destination and ED beds remain occupied, limiting the number available to new patients.
This latter impact can affect ED wait times. And when those are long, patients are more likely to leave before being evaluated. In the second study, researchers assessed the rates at which patients in U.S. hospitals decided to leave EDs before even being seen by a clinician.
From January 2017 to December 2021, the median rate of patients leaving without being seen nearly doubled from 1.1% to 2.1%. At the worst performing hospitals, those rates were as high as 10% by the end of 2021, a number Janke called “astonishing.”
“ It’s a measure of access to care,” he said. “If you have to wait hours and hours to be evaluated in the ED, then that’s not the access to care that we have required by law in [the Emergency Medical Treatment and Active Labor Act, or EMTALA].” (Enacted in 1986, EMTALA requires universal provision of emergency care by hospitals that accept Medicare payments.)
These findings, the researchers say, offer a snapshot of the current state of EDs in the United States, and provide critical data that typically are difficult to obtain in a timely manner. Though hospitals are required to report certain measures on a yearly basis, those data often aren’t released publicly for another two or three years, rendering them irrelevant, said Janke.
“ The health care system is a living, breathing organism, and it’s like we measured its vital signs one time three years ago and that’s how we make public policy,” he said. “You and I should know whether the acute care system where we live has the capacity to address, say, a heart attack or a stroke in a family member. This is a problem that affects population health.”
The researchers want people outside of the ED community to recognize this population-level effect and the impacts of ED crowding.
“ We hope our findings begin to draw attention and accountability for the human toll of the ED boarding crisis,” said Ted Melnick , associate professor of emergency medicine at Yale School of Medicine and an author of the studies.
For both studies, the researchers collected data from a large electronic health record vendor, an approach that’s particularly helpful in the absence of other national or local data.
“ Future partnerships with electronic health record vendors can continue to shed light on crises like this,” Melnick said.
Health & Medicine
Media Contact
Fred Mamoun: [email protected] , 203-436-2643
Tracking the cellular and genetic roots of neuropsychiatric disease

Celebrating staff service

Sea of love: Behind the unusual sexual parasitism of deep-water anglerfish

Peter Raymond appointed Oastler Professor of Biogeochemistry
- Show More Articles

An official website of the United States government
Here’s how you know
Official websites use .gov
A .gov website belongs to an official government organization in the United States.
Secure .gov websites use HTTPS
A lock ( Lock A locked padlock ) or https:// means you’ve safely connected to the .gov website. Share sensitive information only on official, secure websites. .
FEMA Case Study Library
Collections.
- COVID-19 Best Practice Case Studies
- Interagency Recovery Coordination Case Studies
- Mitigation Best Practices
- Preparedness Grants Case Studies
- Assistance to Firefighters Grant Case Studies
- Loss Avoidance Studies
- Risk MAP Best Practices
- Cooperating Technical Partners Program Success Stories

Search All Case Studies
West virginia forms partnerships to increase rural engagement.
West Virginia partners with the Pioneer Network to help spread flood risk information and build community capacity.
Rebuilding Education: Tipton County's Response to a Devastating Tornado
On March 31, 2023, an EF3 tornado wreaked havoc in Tipton County, causing one fatality and 28 injuries in Covington, Tennessee. The Tipton County School Board took on the critical responsibility of swiftly reintegrating students into classrooms for the remainder of the academic year.
Protecting School Children from Tornadoes: State of Kansas School Shelter Initiative
On May 3, 1999, a series of intense storms moved through “Tornado Alley,” producing numerous tornadoes that tore through areas of Oklahoma and Kansas.
Miami County, Ohio: Virtual Inspections
Current building codes require site inspections at several stages throughout the construction process. These can include inspections of concrete slabs, foundation walls, insulation, and roof ice guards, as well as re-inspections of specific or code-required (i.e., welds, masonry, etc.) items.
Hurricane Resistant Building Code Helps Protect Alabama
Coastal Alabama has seen rapid growth over the past decade, but it also happens to be the area most vulnerable to hurricanes and other natural hazards in the state.
Community Wind Shelters: Background and Research
Because of the rising frequency of extreme weather, the Federal Emergency Management Agency (FEMA) strongly encourages homeowners and communities to build safe rooms to FEMA standards. Community shelters have been consistently needed due to the increased risk posed by strong winds and flying debris during natural hazards.
Mitigation Matters: Rebuilding for a Resilient Future
It’s imperative to acquaint yourself with alternative resources designed to mitigate losses resulting from uncovered damages. These resources are equally essential in fortifying your significant investments against the potential impact of natural hazards, fostering resilience, and minimizing vulnerabilities.
Austin: The State Capital’s Fight Against Wildfire
In 2013, Austin was ranked the city with the third greatest risk of wildfire-related structure losses, specifically for communities outside the urban core. These areas, known as the wildland-urban interface, are in the transition zone between undeveloped rural wildlands and developed areas and account for 61% of households in Austin and 64% of the land within Austin city limits.
Puerto Rico: de la recuperación a la resiliencia
Conozca lo aspectos más destacados de los avances en la recuperación de la isla tras los huracanes María y Fiona, y los terremotos de 2020. Este resumen abarca una selección de proyectos de recuperación que afectan al sector de la salud, la seguridad pública, la red energética y las instalaciones de distribución de agua, entre otros.
Puerto Rico: From Recovery to Resilience
Explore highlights of recovery progress on the island after hurricanes María and Fiona, and the earthquakes in 2020. This overview covers a selection of recovery projects that impact the health sector, public safety, energy grid, water distribution facilities and more.
- Join Our List
Emergency Department Case Studies
These case studies were contributed by emergency departments across massachusetts and beyond and serve as examples of innovative strategies that may help improve ed safety..
▸ back to top
Cognitive overload
Care coordination
Republish This Story
Stranded in the ER, Seniors Await Hospital Care and Suffer Avoidable Harm

Every day, the scene plays out in hospitals across America: Older men and women lie on gurneys in emergency room corridors moaning or suffering silently as harried medical staff attend to crises.
Even when physicians determine these patients need to be admitted to the hospital, they often wait for hours — sometimes more than a day — in the ER in pain and discomfort, not getting enough food or water, not moving around, not being helped to the bathroom, and not getting the kind of care doctors deem necessary.
“You walk through ER hallways, and they’re lined from end to end with patients on stretchers in various states of distress calling out for help, including a number of older patients,” said Hashem Zikry, an emergency medicine physician at UCLA Health.
Physicians who staff emergency rooms say this problem, known as ER boarding, is as bad as it’s ever been — even worse than during the first years of the covid-19 pandemic, when hospitals filled with desperately ill patients.
While boarding can happen to all ER patients, adults 65 and older, who account for nearly 20% of ER visits, are especially vulnerable during long waits for care. Also, seniors may encounter boarding more often than other patients. The best estimates I could find, published in 2019, before the covid-19 pandemic, suggest that 10% of patients were boarded in ERs before receiving hospital care. About 30% to 50% of these patients were older adults.
“It’s a public health crisis,” said Aisha Terry, an associate professor of emergency medicine at George Washington University School of Medicine and Health Sciences and the president of the board of the American College of Emergency Physicians, which sponsored a summit on boarding in September.
Email Sign-Up
Subscribe to KFF Health News' free Morning Briefing.
What’s going on? I spoke to almost a dozen doctors and researchers who described the chaotic situation in ERs. They told me staff shortages in hospitals, which affect the number of beds available, are contributing to the crisis. Also, they explained, hospital administrators are setting aside more beds for patients undergoing lucrative surgeries and other procedures, contributing to bottlenecks in ERs and leaving more patients in limbo.
Then, there’s high demand for hospital services, fueled in part by the aging of the U.S. population, and backlogs in discharging patients because of growing problems securing home health care and nursing home care, according to Arjun Venkatesh, chair of emergency medicine at the Yale School of Medicine.
The impact of long ER waits on seniors who are frail, with multiple medical issues, is especially serious. Confined to stretchers, gurneys, or even hard chairs, often without dependable aid from nurses, they’re at risk of losing strength, forgoing essential medications, and experiencing complications such as delirium, according to Saket Saxena, a co-director of the geriatric emergency department at the Cleveland Clinic.
When these patients finally secure a hospital bed, their stays are longer and medical complications more common. And new research finds that the risk of dying in the hospital is significantly higher for older adults when they stay in ERs overnight, as is the risk of adverse events such as falls, infections, bleeding, heart attacks, strokes, and bedsores.
Ellen Danto-Nocton, a geriatrician in Milwaukee, was deeply concerned when an 88-year-old relative with “strokelike symptoms” spent two days in the ER a few years ago. Delirious, immobile, and unable to sleep as alarms outside his bed rang nonstop, the older man spiraled downward before he was moved to a hospital room. “He really needed to be in a less chaotic environment,” Danto-Nocton said.
Several weeks ago, Zikry of UCLA Health helped care for a 70-year-old woman who’d fallen and broken her hip while attending a basketball game. “She was in a corner of our ER for about 16 hours in an immense amount of pain that was very difficult to treat adequately,” he said. ERs are designed to handle crises and stabilize patients, not to “take care of patients who we’ve already decided need to be admitted to the hospital,” he said.
How common is ER boarding and where is it most acute? No one knows, because hospitals aren’t required to report data about boarding publicly. The Centers for Medicare & Medicaid Services retired a measure of boarding in 2021. New national measures of emergency care capacity have been proposed but not yet approved.
“It’s not just the extent of ED boarding that we need to understand. It’s the extent of acute hospital capacity in our communities,” said Venkatesh of Yale, who helped draft the new measures.
In the meantime, some hospital systems are publicizing their plight by highlighting capacity constraints and the need for more hospital beds. Among them is Massachusetts General Hospital in Boston, which announced in January that ER boarding had risen 32% from October 2022 to September 2023. At the end of that period, patients admitted to the hospital spent a median of 14 hours in the ER and 26% spent more than 24 hours.
Maura Kennedy, Mass General’s chief of geriatric emergency medicine, described an 80-something woman with a respiratory infection who languished in the ER for more than 24 hours after physicians decided she needed inpatient hospital care.
“She wasn’t mobilized, she had nothing to cognitively engage her, she hadn’t eaten, and she became increasingly agitated, trying to get off the stretcher and arguing with staff,” Kennedy told me. “After a prolonged hospital stay, she left the hospital more disabled than she was when she came in.”
When I asked ER doctors what older adults could do about these problems, they said boarding is a health system issue that needs health system and policy changes. Still, they had several suggestions.
“Have another person there with you to advocate on your behalf,” said Jesse Pines, chief of clinical innovation at US Acute Care Solutions, the nation’s largest physician-owned emergency medicine practice. And have that person speak up if they feel you’re getting worse or if staffers are missing problems.
Alexander Janke, a clinical instructor of emergency medicine at the University of Michigan, advises people, “Be prepared to wait when you come to an ER” and “bring a medication list and your medications, if you can.”
To stay oriented and reduce the possibility of delirium, “make sure you have your hearing aids and eyeglasses with you,” said Michael Malone, medical director of senior services for Advocate Aurora Health, a 20-hospital system in Wisconsin and northern Illinois. “Whenever possible, try to get up and move around.”
Friends or family caregivers who accompany older adults to the ER should ask to be at their bedside, when possible, and “try to make sure they eat, drink, get to the bathroom, and take routine medications for underlying medical conditions,” Malone said.
Older adults or caregivers who are helping them should try to bring “things that would engage you cognitively: magazines, books … music, anything that you might focus on in a hallway where there isn’t a TV to entertain you,” Kennedy said.
“Experienced patients often show up with eye masks and ear plugs” to help them rest in ERs with nonstop stimulation, said Zikry of UCLA. “Also, bring something to eat and drink in case you can’t get to the cafeteria or it’s a while before staffers bring these to you.”
We’re eager to hear from readers about questions you’d like answered, problems you’ve been having with your care, and advice you need in dealing with the health care system. Visit kffhealthnews.org/columnists to submit your requests or tips.
Related Topics
- Navigating Aging
- Public Health
- Emergency Medicine
Copy And Paste To Republish This Story
By Judith Graham Updated May 6, 2024 Originally Published May 6, 2024
“You walk through ER hallways, and they’re lined from end to end with patients on stretchers in various states of distress calling out for help, including a number of older patients,” said Hashem Zikry, an emergency medicine physician at UCLA Health.
Physicians who staff emergency rooms say this problem, known as ER boarding, is as bad as it’s ever been — even worse than during the first years of the covid-19 pandemic, when hospitals filled with desperately ill patients.
“It’s a public health crisis,” said Aisha Terry, an associate professor of emergency medicine at George Washington University School of Medicine and Health Sciences and the president of the board of the American College of Emergency Physicians, which sponsored a summit on boarding in September.
What’s going on? I spoke to almost a dozen doctors and researchers who described the chaotic situation in ERs. They told me staff shortages in hospitals, which affect the number of beds available, are contributing to the crisis. Also, they explained, hospital administrators are setting aside more beds for patients undergoing lucrative surgeries and other procedures, contributing to bottlenecks in ERs and leaving more patients in limbo.
Then, there’s high demand for hospital services, fueled in part by the aging of the U.S. population, and backlogs in discharging patients because of growing problems securing home health care and nursing home care, according to Arjun Venkatesh, chair of emergency medicine at the Yale School of Medicine.
The impact of long ER waits on seniors who are frail, with multiple medical issues, is especially serious. Confined to stretchers, gurneys, or even hard chairs, often without dependable aid from nurses, they’re at risk of losing strength, forgoing essential medications, and experiencing complications such as delirium, according to Saket Saxena, a co-director of the geriatric emergency department at the Cleveland Clinic.
Ellen Danto-Nocton, a geriatrician in Milwaukee, was deeply concerned when an 88-year-old relative with “strokelike symptoms” spent two days in the ER a few years ago. Delirious, immobile, and unable to sleep as alarms outside his bed rang nonstop, the older man spiraled downward before he was moved to a hospital room. “He really needed to be in a less chaotic environment,” Danto-Nocton said.
Several weeks ago, Zikry of UCLA Health helped care for a 70-year-old woman who’d fallen and broken her hip while attending a basketball game. “She was in a corner of our ER for about 16 hours in an immense amount of pain that was very difficult to treat adequately,” he said. ERs are designed to handle crises and stabilize patients, not to “take care of patients who we’ve already decided need to be admitted to the hospital,” he said.
How common is ER boarding and where is it most acute? No one knows, because hospitals aren’t required to report data about boarding publicly. The Centers for Medicare & Medicaid Services retired a measure of boarding in 2021. New national measures of emergency care capacity have been proposed but not yet approved.
“It’s not just the extent of ED boarding that we need to understand. It’s the extent of acute hospital capacity in our communities,” said Venkatesh of Yale, who helped draft the new measures.
Maura Kennedy, Mass General’s chief of geriatric emergency medicine, described an 80-something woman with a respiratory infection who languished in the ER for more than 24 hours after physicians decided she needed inpatient hospital care.
“She wasn’t mobilized, she had nothing to cognitively engage her, she hadn’t eaten, and she became increasingly agitated, trying to get off the stretcher and arguing with staff,” Kennedy told me. “After a prolonged hospital stay, she left the hospital more disabled than she was when she came in.”
“Have another person there with you to advocate on your behalf,” said Jesse Pines, chief of clinical innovation at US Acute Care Solutions, the nation’s largest physician-owned emergency medicine practice. And have that person speak up if they feel you’re getting worse or if staffers are missing problems.
Alexander Janke, a clinical instructor of emergency medicine at the University of Michigan, advises people, “Be prepared to wait when you come to an ER” and “bring a medication list and your medications, if you can.”
To stay oriented and reduce the possibility of delirium, “make sure you have your hearing aids and eyeglasses with you,” said Michael Malone, medical director of senior services for Advocate Aurora Health, a 20-hospital system in Wisconsin and northern Illinois. “Whenever possible, try to get up and move around.”
Friends or family caregivers who accompany older adults to the ER should ask to be at their bedside, when possible, and “try to make sure they eat, drink, get to the bathroom, and take routine medications for underlying medical conditions,” Malone said.
Older adults or caregivers who are helping them should try to bring “things that would engage you cognitively: magazines, books … music, anything that you might focus on in a hallway where there isn’t a TV to entertain you,” Kennedy said.
“Experienced patients often show up with eye masks and ear plugs” to help them rest in ERs with nonstop stimulation, said Zikry of UCLA. “Also, bring something to eat and drink in case you can’t get to the cafeteria or it’s a while before staffers bring these to you.”
We’re eager to hear from readers about questions you’d like answered, problems you’ve been having with your care, and advice you need in dealing with the health care system. Visit kffhealthnews.org/columnists to submit your requests or tips.
We encourage organizations to republish our content, free of charge. Here’s what we ask:
You must credit us as the original publisher, with a hyperlink to our kffhealthnews.org site. If possible, please include the original author(s) and KFF Health News” in the byline. Please preserve the hyperlinks in the story.
It’s important to note, not everything on kffhealthnews.org is available for republishing. If a story is labeled “All Rights Reserved,” we cannot grant permission to republish that item.
Have questions? Let us know at KHNHelp@kff.org
More From KFF Health News

Medicaid Unwinding Deals Blow to Tenuous System of Care for Native Americans

Newsom Boosted California’s Public Health Budget During Covid. Now He Wants To Cut It.

Clean Needles Save Lives. In Some States, They Might Not Be Legal.

Journalists Broach Topics From Treating Shooting Victims to Sunscreen Safety
Thank you for your interest in supporting Kaiser Health News (KHN), the nation’s leading nonprofit newsroom focused on health and health policy. We distribute our journalism for free and without advertising through media partners of all sizes and in communities large and small. We appreciate all forms of engagement from our readers and listeners, and welcome your support.
KHN is an editorially independent program of KFF (Kaiser Family Foundation). You can support KHN by making a contribution to KFF, a non-profit charitable organization that is not associated with Kaiser Permanente.
Click the button below to go to KFF’s donation page which will provide more information and FAQs. Thank you!
- Open access
- Published: 17 May 2024
Antibiotic susceptibility patterns and trends of the gram-negative bacteria isolated from the patients in the emergency departments in China: results of SMART 2016–2019
- Ying Fu 1 , 2 ,
- Feng Zhao 1 , 2 ,
- Jie Lin 1 , 2 ,
- Pengcheng Li 3 &
- Yunsong Yu 4 , 5 , 6
BMC Infectious Diseases volume 24 , Article number: 501 ( 2024 ) Cite this article
197 Accesses
8 Altmetric
Metrics details
The study aims were to evaluate the species distribution and antimicrobial resistance profile of Gram-negative pathogens isolated from specimens of intra-abdominal infections (IAI), urinary tract infections (UTI), respiratory tract infections (RTI), and blood stream infections (BSI) in emergency departments (EDs) in China.
From 2016 to 2019, 656 isolates were collected from 18 hospitals across China. Minimum inhibitory concentrations were determined by CLSI broth microdilution and interpreted according to CLSI M100 (2021) guidelines. In addition, organ-specific weighted incidence antibiograms (OSWIAs) were constructed.
Escherichia coli ( E. coli ) and Klebsiella pneumoniae ( K. pneumoniae ) were the most common pathogens isolated from BSI, IAI and UTI, accounting for 80% of the Gram-negative clinical isolates, while Pseudomonas aeruginosa ( P. aeruginosa ) was mainly isolated from RTI. E. coli showed < 10% resistance rates to amikacin, colistin, ertapenem, imipenem, meropenem and piperacillin/tazobactam. K. pneumoniae exhibited low resistance rates only to colistin (6.4%) and amikacin (17.5%) with resistance rates of 25–29% to carbapenems. P. aeruginosa exhibited low resistance rates only to amikacin (13.4%), colistin (11.6%), and tobramycin (10.8%) with over 30% resistance to all traditional antipseudomonal antimicrobials including ceftazidime, cefepime, carbapenems and levofloxacin. OSWIAs were different at different infection sites. Among them, the susceptibility of RTI to conventional antibiotics was lower than for IAI, UTI or BSI.
Conclusions
Gram-negative bacteria collected from Chinese EDs exhibited high resistance to commonly used antibiotics. Susceptibilities were organ specific for different infection sites, knowledge which will be useful for guiding empirical therapies in the clinic.
Peer Review reports
Antimicrobials are frequently used in emergency departments (EDs) in China and a study noted that the proportion of emergency patients treated with antibiotics was as high as 39.31 to 43.45% from 2016 to 2019 [ 1 ]. Antibiotic stewardship in EDs should avoid administration of broad-spectrum antibiotics, shorten their use times, as well as minimizing their unnecessary use [ 2 ]. However, as patients presenting to EDs are often in an acute state, physicians have to make decisions in a very short time frame and they prescribe antibiotics empirically. For critically ill infected patients, guidelines recommend to start antibiotic treatment in the first hour of recognition [ 3 ], which means that it is frequently impossible to get microbiology results to guide the choice of antimicrobial therapy. In order to support the choice of empiric antibiotic treatments, consensus guidelines as well as local antibiotic drug susceptibility detection and various antimicrobial surveillance programs have been introduced in China [ 4 , 5 ].
One approach to individualized empiric antibiotic therapy is the Weighted-Incidence Syndromic Combination Antibiogram, which is comprised of information about the likelihood a treatment regimen will be effective for all relevant organisms for a given infection based on existing large datasets [ 6 , 7 , 8 ]. A similar approach is the organ-specific weighted incidence antibiogram (OSWIA), which estimates probable susceptibilities of organ specific isolates to specific antibiotics [ 9 ]. The Study for Monitoring Antimicrobial Resistance Trends (SMART) global surveillance program monitors in vitro susceptibilities of clinical Gram-negative bacilli to antimicrobial agents obtained from blood stream infections (BSI), intra-abdominal infections (IAI), urinary tract infections (UTI) and respiratory tract infections (RTI). The purpose of the present study was to determine the prevalence and susceptibilities of various bacteria to conventional antibiotics in patients attending Chinese EDs through a retrospective analysis of the SMART data collected from 2016 to 2019 and to determine differences of organ distributions between the infecting bacterial strains.
In this study, the patient informed consent was waived and authorized by the Ethics Committee of Sir Run Run Shaw Hospital, Zhejiang University School of Medicine (Approval Number: 20210811-33).
All bacterial isolates were collected from discarded clinical specimens of hospitalized patients with BSI, IAI, UTI and RTI between 2016 and 2019 who were admitted to the EDs of 18 hospitals across China (Supplementary Table 1 ). The IAI specimen is derived from tissues or organs within the abdominal cavity, including the stomach, intestines, liver, spleen, pancreas, kidneys that have been infected by pathogens, resulting in infectious diseases [ 10 ]. RTI refers to an infection of the tissues in the respiratory system by pathogens such as viruses, bacteria, or fungi. RTI specimens from the respiratory tract included nasal and throat swabs, sputum samples, bronchoalveolar lavage fluid, respiratory secretions, and others [ 11 ]. Identification of isolates was initially made by each hospital laboratory and then the specimens were sent for laboratory re-identification using MALDI-TOF/MS (Bruker Daltonics, USA). Any duplicate isolates collected from the same patient were excluded from the data analysis.
Antimicrobial susceptibility testing
Testing was carried out in the Peking Union Medical College Hospital clinical microbiology laboratory using the Trek Diagnostic System (Thermo Fisher Scientific). Clinical isolates and reference strains were detected using the microbroth dilution method. Minimum inhibitory concentrations (MICs) were determined with reference to the antimicrobial breakpoint of the CLSI M100 (2021) [ 12 ]. The antibiotics tested were amikacin (AMK), cefepime (FEP), ceftazidime (CAZ), aztreonam (ATM), ceftriaxone (CRO), colistin (COL), ertapenem (ETP), levofloxacin (LVX), cefoxitin (FOX), imipenem (IPM), tobramycin (TOB), meropenem (MEM) and piperacillin–tazobactam (TZP).
Definition of antimicrobial-resistant strains
Carbapenem resistance of Escherichia coli ( E. coli ) and Klebsiella pneumoniae ( K. pneumoniae ) refers to resistance to any of IPM, MEM or ETP. Carbapenem-resistant Pseudomonas aeruginosa ( P. aeruginosa ) was defined as resistance to IPM or MEM.
Quinolone resistance to E. coli, K. pneumoniae and P. aeruginosa was defined as resistance to LVX.
Third generation cephalosporin resistance to E. coli and K. pneumoniae was defined as resistance to any CRO or CAZ, and the strains susceptible or intermediate to carbapenems (IPM, MEM or ETP). P. aeruginosa resistant to third-generation cephalosporin was defined as resistance to CAZ (CAZ-resistant PA) and the strains susceptible or intermediate to carbapenems (IPM, MEM).
OSWIA calculation
Data were retrospectively analyzed to establish the distribution of bacteria in various organs for BSI, IAI, UTI and RTI. OSWIA values were determined as previously described [ 9 ].
Patient characteristics and specimen source
Between January 01, 2016 and December 31, 2019, a total of 656 isolated were obtained from ED patients. The patient characteristics are detailed in Table 1 . The patients average age was 60.6 years (range: 1–101), comprising 388 males and 268 females. Most infections were hospital-acquired (HA) (58.1%), while 249 (38.0%) were community-acquired (CA) and for 26 data were not applicable. The isolates included 210 strains from IAI collected during surgery from the peritoneal fluid, appendix, abscesses, pancreas, gall bladder, liver and stomach. A total of 122 strains from BSI, 112 strains from UTI mainly from the urine, and 208 strains from RTI taken from bronchoalveolar lavage, endotracheal aspirate, thoracentesis or sputum were identified, as well as 4 strains from unconfirmed organs.
Distribution of Gram-negative bacteria obtained from BSI, IAI, UTI and RTI
Enterobacterales were the most common Gram-negative bacilli isolated from emergency patients with BSI, IAI and UTI (Fig. 1 ). E. coli accounted for 48.4% in BSI, 58.6% in IAI and 72.3% in UTI, while K. pneumoniae accounted for 24.6%, 21.4% and 11.6%, respectively and other Enterobacterales were much less common than E. coli and K. pneumoniae . The pathogen distribution in RTI was distinctly different from the other three infection types, with P. aeruginosa and K. pneumoniae being the most common species each accounting for about 40% of the Gram-negative pathogens. Since the composition ratio of Gram-negative bacteria was different at different infection sites (Fig. 1 , Supplementary Table 2 ) the varying patterns between infected organs should be considered when prescribing empirical treatments.
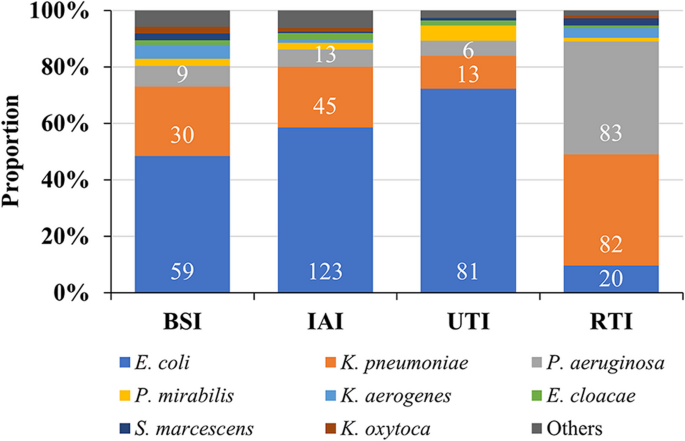
Distribution of Gram-negative bacilli in BSI, IAI, UTI and RTI. Abbreviations: BSI, blood steam infection; IAI, intra-abdominal infection; UTI, urinary tract infection
Distribution of Gram-negative bacteria from 2016 to 2019
The distribution of Gram-negative pathogens was stable between 2016 and 2019, with E. coli , K. pneumoniae and P. aeruginosa being the top 3 species, accounting for more than 80% of the clinical isolates (Fig. 2 , Supplementary Table 3 ).
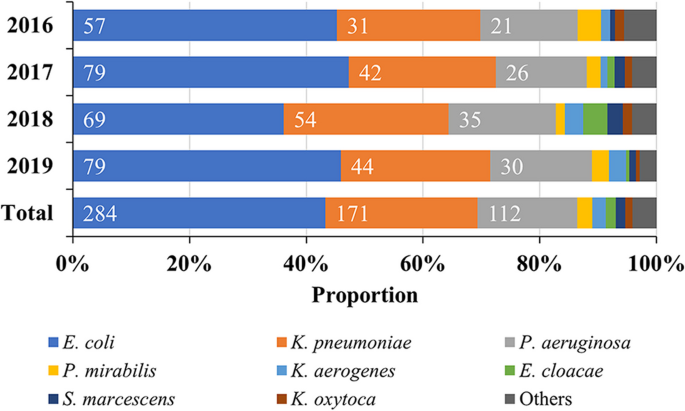
Composition ratio of Gram-negative bacteria in EDs from 2016 to 2019. Abbreviation: ED, emergency department.
Distribution of Gram-negative bacteria in different age groups of patients
Among the strains collected, regardless of the organ of origin, the predominant species were P. aeruginosa, E. coli and K. pneumoniae . However, the composition ratio of the main bacterial groups were different in infection sites within age groups (Fig. 3 a-d) and were generally different especially in the age group ≤ 39 years (Fig. 3 e, Supplementary Table 4 ).
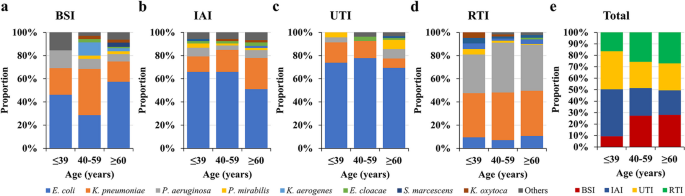
Comparison of the composition ratio of microbiota in different infected organs and age groups. Abbreviations: BSI, blood steam infection; IAI, intra-abdominal infection; RTI, respiratory tract infection; UTI, urinary tract infection.
Monitoring of drug susceptibility
Drug resistance rate monitoring of major gram-negative bacteria from 2016 to 2019.
E. coli exhibited < 10% resistance to AMK, COL, ETP, IPM, MEM and TZP, with the exception in 2016 to TZP, but generally TZP resistance rates were reduced between 2016 and 2019. Otherwise, resistance rates were more than 30%, with the exception of FOX (16.2%). K. pneumoniae exhibited < 20% resistance only to AMK and 6.4% to COL between 2016 and 2019. P. aeruginosa only exhibited low resistant rates of 13.4% to AMK, 11.6% to COL and 10.8% to TOB from 2016 to 2019 (Table 2 ).
Detection rate and drug susceptibility of specific antibiotic-resistant bacteria from 2016 to 2019
Isolation of carbapenem-resistant, quinolone-resistant or third-generation cephalosporin-resistant e. coli, k. pneumoniae and p. aeruginosa.
In isolates, the carbapenem-resistant E. coli and P. aeruginosa showed an overall downward trend. However, the rate of detection of carbapenem-resistant E. coli was relatively low, being only 1.3% in 2019, while for carbapenem-resistant P. aeruginosa in 2019 it was 30.0% and for carbapenem-resistant K. pneumoniae strains in 2019, 34.1%, the rate being higher than in 2018 (18.5%). The rate of detection of quinolone-resistant E. coli or K. pneumoniae showed a decreasing trend in the four years studied, being 55.7% in 2019 for the detection of quinolone-resistant E. coli and 36.4% for K. pneumoniae . The detection rate of quinolone-resistant P. aeruginosa was 26.7% in 2019 and lower than in 2018 (42.9%). The detection rates of third-generation cephalosporin-resistant E. coli and K. pneumoniae as well as P. aeruginosa showed an irregular trend from 2016 to 2019, being between 44.3%–63.2% and 9.1%–24.1% as well as 2.9%–15.4%, respectively throughout the years. Compared to E. coli, there were only few numbers of third-generation cephalosporin-resistant K. pneumoniae and P. aeruginosa isolates found between 2016 and 2019 (Fig. 4 , Supplementary Table 5 ).
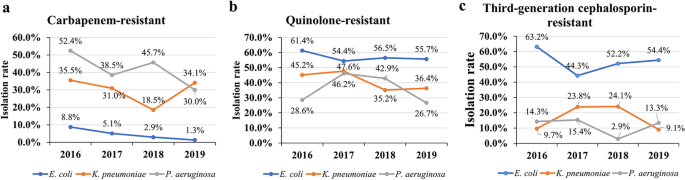
Isolation (detection) rate of carbapenem-resistant, quinolone-resistant, third-generation cephalosporin-resistant E. coli , K. pneumoniae and P. aeruginosa from 2016 to 2019
Specific drug resistance rates (%) of strains to antibiotics from 2016 to 2019
For E. coli , the resistance rate of carbapenem-resistant E. coli to AMK was 33.3%, and to the other antibiotics tested were > 60%, apart from COL (25.0%). Quinolone-resistant E. coli exhibited the lowest resistance rates to AMK (4.3%), ETP (5.6%), IPM (5.0%) and MEM (5.6%). The resistance rates of third-generation cephalosporin-resistant E. coli was 2.0% to AMK and 0% to ETP, IPM and MEM.
Carbapenem-resistant K. pneumoniae were 57.1% resistant to AMK and quinolone-resistant K. pneumoniae were 42.0% resistant to AMK, with low resistance rates only found to COL (8.2% and 10.1%), respectively. Third-generation cephalosporin-resistant K. pneumoniae was 6.7% resistant to AMK and 0% to ETP, IPM and MEM.
For carbapenem-resistant P. aeruginosa , the drug resistance to AMK was 30.4%, for TOB 28.0% and for COL (10.9%). For quinolone-resistant P. aeruginosa, only resistance rates to AMK (24.4%) and TOB (26.1%) as well as COL (9.8%) remained low. Third-generation cephalosporins resistant P. aeruginosa, showed low resistance rates of 0% to AMK, IPM, MEM and TOB (Table 3 ).
Antimicrobial susceptibility monitoring during empiric treatment of different infection sites and organs
In the weighted susceptibility assessment of different infection sites, it was found that the susceptibility of the same antibacterial drug at different organs and infection sites was different. For example, AMK, TOB, ETP, IPM and MEM were the antibiotics with > 90% susceptibility for BSI, but only AMK and MEM were > 90% effective antibiotics against IAI. High-susceptibility to antibiotics in UTI included AMK, TOB and MEM (all > 90%), and except for AMK, COL and TOB, the susceptibility to other antibiotics at the site of RTI infections was < 80% (Fig. 5 , Supplementary Table 6 ).
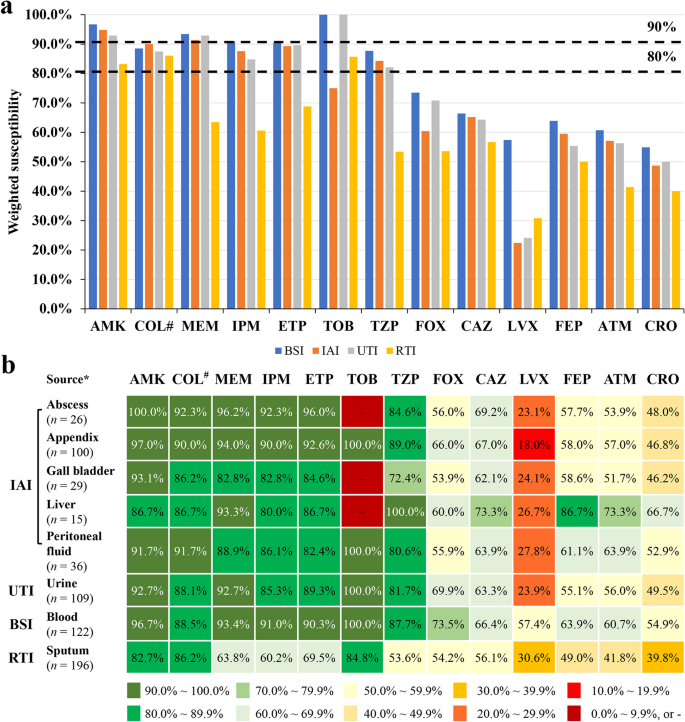
Organ distribution related susceptibilities. a Differences in susceptibility of antibiotics at different infection sites. b Differences in weighted drug susceptibilities of antibiotics at different organs and infection sites. Note: *only sites from which more than 10 pathogenic bacteria were collected have been included; #, intermediate rate was shown for COL; -, no detection. Abbreviations: AMK, amikacin; ATM, aztreonam; BSI, blood steam infections; CAZ, ceftazidime; CRO, ceftriaxone; ETP, ertapenem; FEP, cefepime; FOX, cefoxitin; IAI, intra-abdominal infections; IPM, imipenem; LVX, levofloxacin; MEM, meropenem; RTI, respiratory tract infections; TOB, tobramycin; TZP, piperacillin/tazobactam; UTI, urinary tract infections
This study analyzed Chinese data from the global SMART surveilance program and found that the most frequently isolated Gram-negative bacteria were Enterobacterales , a finding similar to previous results from SMART studies and the China Antimicrobial Surveillance Network (CHINET) [ 13 , 14 ]. Enterobacterales are of particular concern given their ability to develop and spread resistance to penicillins, cephalosporins, carbapenems and quinolones [ 12 , 15 , 16 ]. As these are the most commonly used antibiotics in hospitals, such resistance would leave physicians with very limited treatment options. The vast majority of the pathogens were E. coli , K. pneumoniae and P. aeruginosa (86.4%), with resistance rates for cephalosporins in the range of 31.0%–57.0% and for ATM 44.0%–45.5%, indicating a high rate of ESBL-producing strains [ 17 ], which underlines the global health problem of cephalosporin resistance [ 18 ]. Previous SMART surveilence results found ESBL rates of 46.3%–49.1% for E. coli and 25.6%–26.8% for K. pneumoniae [ 13 ]. In the 2021 CHINET surveillance, resistance to third-generation cephalosporins was detected in 55.6% of E. coli and 43.8% of K. pneumoniae , also indicating the high ESBL prevalence in China [ 14 ]. The resistance rates for the fluoroquinolone LVX (36.6%–56.7%) were in a similar range to cephalosporins in this study, which might reflect the overuse of fluoroquinolones, especially since the development of cephalosporin-resistance [ 19 , 20 ]. They were similar to the rates reported by the 2021 CHINET surveillance of LVX resistance detected as 53.6% for E. coli and 28.3% for K. pneumoniae isolates [ 14 ]. One approach to overcome cephalosporin resistance is the use of combination of a β-lactam and a β-lactamase inhibitor [ 21 ], such as tazobactam, which led to essentially reduced resistance rates of about 10% for otherwise cephalosporin-resistant E. coli and K. pneumoniae in the present study. Of concern is the rising resistance rate of K. pneumoniae to carbapenems , which reached25%–29% in the present study and was similar to the rate of about 25% found in the 2021 CHINET surveillance study [ 14 ].
Resistance rates for COL were generally low, but susceptibility breakpoints have been abolished in recent CLSI guidelines. Treatments with COL should be applied with maximum renally adjusted doses, since the previous MIC of 2 μg/mL could not be achieved in 50% of patients with normal renal functions and acute kidney injury occurs frequently with conventional doses. Recommendations include strongly preferred alternative drugs for active or combination treatments [ 22 , 23 ]. Also, TOB is not commonly used in China, which might explain the low resistance rates found in the present study.
P. aeruginosa was the third most common pathogen detected and the most common Gram-negative pathogen found in RTI. It exhibited > 30% resistance to traditional antipesudomoas antibiotics, including CAZ, FEP, TZP, IPM, MEM and LVX. These results are similar to those reported in a recent SMART study that investigated P. seudomonas resistance to antibiotics in China [ 24 ].
This present survey included only isolates collected in EDs, since patients admitted to EDs are frequently candidates for urgent empiric antibiotic treatment, which should be administered according to the site of infection and the clinical severity of symptoms [ 25 ]. The characteristics of infected patients and physicians' routine treatments in the ED differed compared to other departments. This is because the infected site may initially not be clearly defined, patients cannot be observed for a long period of time, and etiological evidence is rarely available; doctors and nurses in EDs also have a very heavy workload. It is therefore convenient to use drugs which only need administration once a day to ED patients, including ETP once a day, AMK intramuscular injection, as well as LVX once a day, which can be sequenced simultaneously.
In order to offer guidelines for chosing an empiric treatment, organ specific therapy based on pathogen distribution differences and their antibiotic resistance variations have been developed [ 6 , 8 ]. Of these, OSIWA was first applied for HA and CA infections of different intra-abdominal organs [ 9 ]. In the present study, we expanded the evaluation of OSIWA for the empirical treatment of IAI also to UTI, BSI and RTI. When considering the distribution of pathogens at a single infection site – for example E. coli caused more than 50% of all IAI and more than 60% of all UTI – whereas for RTI infections E. coli was the pathogen in < 15% of all cases (Fig. 3 ). The OSIWA shown in Fig 5 indicate the probabilities of successful empiric drug treatment for single infections sites. For RTI and IAI the choice of empirical antibiotics with expected efficacy was limited, but for UTI and BSI more antibiotics are available.
Limitations of the present survey were the relatively low sample numbers since only isolates from EDs have been included, which have had an influence on the resistance patterns reported and combination treatments with β-lactams, aminoglycoside and fluoroquinolone were not considered. In addition, since in the SMART data collection detailed data regarding resistance mechanisms are not included, susceptibility test results only can infer the mechanism of ESBL production in cephalosporin but not in carbapenem resistance.
The pathogens isolated from BSI, IAI, UTI and RTI between 2016 and 2019 in Chinese EDs were mainly E. coli, K. pneumoniae and P. aeruginosa ,but therewere considerable resistance pattern differences as well as organ distributions between the bacterial strains. OSIWA determinations led to organ specific antibiotic drug effectiveness patterns, which should help to guide the choice of suitable empirical antibiotic treatments, especially for urgent infected cases in EDs.
Availability of data and materials
The SMART database is not public and is only accessible to SMART investigators, but the data that support the findings of this study are directly available from MSD China or from the corresponding author Yunsong Yu upon reasonable request and with permission of MSD China.
Abbreviations
blood stream infections
community acquired
ceftazidime
China Antimicrobial Surveillance Network
ceftriaxone
emergency departments
hospital acquired
intra-abdominal infections
levofloxacin
minimum inhibitory concentrations
organ-specific weighted incidence antibiograms
respiratory tract infections.
Study for Monitoring Antimicrobial Resistance Trends
piperacillin–tazobactam
urinary tract infections
Zhu Y, Qiao Y, Dai R, Hu X, Li X. Trends and patterns of antibiotics use in China’s Urban tertiary hospitals, 2016-19. Front Pharmacol. 2021;12:757309.
Article CAS PubMed PubMed Central Google Scholar
Luyt C-E, Bréchot N, Trouillet J-L, Chastre J. Antibiotic stewardship in the intensive care unit. Crit Care. 2014;18(5):480.
Article PubMed PubMed Central Google Scholar
Evans L, Rhodes A, Alhazzani W, Antonelli M, Coopersmith CM, French C, et al. Surviving sepsis campaign: international guidelines for management of sepsis and septic shock 2021. Crit Care Med. 2021;49(11):e1063-1143.
Article PubMed Google Scholar
Hay SI, Rao PC, Dolecek C, Day NPJ, Stergachis A, Lopez AD, et al. Measuring and mapping the global burden of antimicrobial resistance. BMC Med. 2018;16(1):78.
Schnall J, Rajkhowa A, Ikuta K, Rao P, Moore CE. Surveillance and monitoring of antimicrobial resistance: limitations and lessons from the GRAM project. BMC Med. 2019;17(1):176.
Randhawa V, Sarwar S, Walker S, Elligsen M, Palmay L, Daneman N. Weighted-incidence syndromic combination antibiograms to guide empiric treatment of critical care infections: a retrospective cohort study. Crit Care. 2014;18(3):R112.
Cook A, Sharland M, Yau Y, Group* P, Bielicki J. Improving empiric antibiotic prescribing in pediatric bloodstream infections: a potential application of weighted-incidence syndromic combination antibiograms (WISCA). Expert Rev Anti Infect Ther. 2022;20(3):445–56.
Article CAS PubMed Google Scholar
Hebert C, Ridgway J, Vekhter B, Brown EC, Weber SG, Robicsek A. Demonstration of the weighted-incidence syndromic combination antibiogram: an empiric prescribing decision aid. Infect Control Hosp Epidemiol. 2012;33(4):381–8.
Liu L, Ni Y. Antimicrobial susceptibilities of specific syndromes created with organ-specific weighted incidence antibiograms (OSWIA) in patients with intra-abdominal infections. BMC Infect Dis. 2018;18(1):584.
Chinese Society of Surgical Infection and Intensive Care, Chinese Society of Surgery, Chinese Medical Association. Chinese College of Gastrointestinal Fistula Surgeons, Chinese College of Surgeons, Chinese Medical Doctor Association. Chinese guideline for the diagnosis and management of intra-abdominal infection (2019 edition). Chin J Practical Surg. 2020;40(1):1–16.
Google Scholar
Chinese Medical Association. Clinical Guidelines: Respiratory diseases. Beijing: People’s Medical Publishing House; 2009. p. 174.
Nordmann P, Poirel L. Emergence of plasmid-mediated resistance to quinolones in enterobacteriaceae. J Antimicrob Chemother. 2005;56(3):463–9.
Zhang H, Johnson A, Zhang G, Yang Y, Zhang J, Li D, et al. Susceptibilities of Gram-negative bacilli from hospital- and community-acquired intra-abdominal and urinary tract infections: a 2016–2017 update of the Chinese SMART study. Infect Drug Resist. 2019;12:905–14.
Fupin HU, Yan GUO, Demei ZHU, Fu W, Xiaofei J, Yingchun XU, et al. CHINET surveillance of antimicrobial resistance among the bacterial isolates in 2021. Chin J Infect Chemother. 2022;22(5):521–30.
Ma J, Song X, Li M, Yu Z, Cheng W, Yu Z, et al. Global spread of carbapenem-resistant Enterobacteriaceae: Epidemiological features, resistance mechanisms, detection and therapy. Microbiol Res. 2023;266:127249.
De Angelis G, Del Giacomo P, Posteraro B, Sanguinetti M, Tumbarello M. Molecular mechanisms, epidemiology, and clinical importance of beta-lactam resistance in enterobacteriaceae. Int J Mol Sci. 2020;21(14):5090.
Rawat D, Nair D. Extended-spectrum β-lactamases in gram negative bacteria. J Glob Infect Dis. 2010;2(3):263–74.
Pana ZD, Zaoutis T. Treatment of extended-spectrum β-lactamase-producing Enterobacteriaceae (ESBLs) infections: what have we learned until now? F1000Res.2018;7:F1000 Faculty Rev-1347.
Ezelarab HAA, Abbas SH, Hassan HA, Abuo-Rahma GEA. Recent updates of fluoroquinolones as antibacterial agents. Arch Pharm (Weinheim). 2018;351(9):e1800141.
Hou J, Long X, Wang X, Li L, Mao D, Luo Y, et al. Global trend of antimicrobial resistance in common bacterial pathogens in response to antibiotic consumption. J Hazard Mater. 2023;442:130042.
Yahav D, Giske CG, Grāmatniece A, Abodakpi H, Tam VH, Leibovici L. New β-Lactam-β-Lactamase Inhibitor Combinations. Clin Microbiol Rev. 2020;34(1);e00115.
Satlin MJ, Lewis JS, Weinstein MP, Patel J, Humphries RM, Kahlmeter G, et al. Clinical and laboratory standards institute and European committee on antimicrobial susceptibility testing position statements on polymyxin b and colistin clinical breakpoints. Clin Infect Dis. 2020;71(9):e523-529.
CAS PubMed Google Scholar
Tsuji BT, Pogue JM, Zavascki AP, Paul M, Daikos GL, Forrest A, et al. International consensus guidelines for the optimal use of the polymyxins: endorsed by the American College of Clinical Pharmacy (ACCP), European Society of Clinical Microbiology and Infectious Diseases (ESCMID), Infectious Diseases Society of America (IDSA), International Society for Anti-infective Pharmacology (ISAP), Society of Critical Care Medicine (SCCM), and Society of Infectious Diseases Pharmacists (SIDP). Pharmacotherapy. 2019;39(1):10–39.
Croche Santander B, Campos Alonso E, Sanchez Carrion A, Marcos Fuentes L, Diaz Flores I, Vargas JC, et al. [Appropriateness of antibiotic prescribing in paediatric patients in a hospital emergency department]. Pediatr (Engl Ed). 2018;88(5):259–65.
Kollef MH, Shorr AF, Bassetti M, Timsit J-F, Micek ST, Michelson AP, et al. Timing of antibiotic therapy in the ICU. Crit Care. 2021;25(1):360.
Download references
Acknowledgements
The authors thank Shanghai BIOMED Science Technology Co., Ltd (Shanghai, China) for providing editorial assistance and MSD China for their financial support.
This study was sponsored by funding from Merck Sharp & Dohme LLC, a subsidiary of Merck & Co., Inc., Rahway, New Jersey, USA. The funding body was involved in the study design, analysis and interpretation of data, as well as the decision to submit the article for publication.
Author information
Authors and affiliations.
Department of Clinical Laboratory, Sir Run Run Shaw Hospital, School of Medicine, Zhejiang University, 310016, Hangzhou, Zhejiang Province, China
Ying Fu, Feng Zhao & Jie Lin
Key Laboratory of Precision Medicine in Diagnosis and Monitoring Research of Zhejiang Province, 310016, Hangzhou, Zhejiang Province, China
MRL Global Medical Affairs, MSD China, 200233, Shanghai, China
Pengcheng Li
Department of Infectious Diseases, Sir Run Run Shaw Hospital, School of Medicine, Zhejiang University, 310016, Hangzhou, Zhejiang Province, China
Key Laboratory of Microbial Technology and Bioinformatics of Zhejiang Province, 310012, Hangzhou, Zhejiang Province, China
Regional Medical Center for National Institute of Respiratory Diseases, Sir Run Run Shaw Hospital, School of Medicine, Zhejiang University, 310016, Hangzhou, Zhejiang Province, China
You can also search for this author in PubMed Google Scholar
Contributions
All authors made substantial contributions to the conception and design of the study, acquisition of data, or analysis and interpretation of data, took part in drafting the manuscript or critically revising it for important intellectual content, agreed to submit it to the current journal, gave final approval of the version to be published and agreed to be accountable for all aspects of the work.
Corresponding author
Correspondence to Yunsong Yu .
Ethics declarations
Ethical approval and consent to participate, consent for publication.
Not applicable.
Competing interests
Pengcheng Li is an employee of MSD China. All other authors declare no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Supplementary material 1., rights and permissions.
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Fu, Y., Zhao, F., Lin, J. et al. Antibiotic susceptibility patterns and trends of the gram-negative bacteria isolated from the patients in the emergency departments in China: results of SMART 2016–2019. BMC Infect Dis 24 , 501 (2024). https://doi.org/10.1186/s12879-024-09294-0
Download citation
Received : 14 December 2023
Accepted : 05 April 2024
Published : 17 May 2024
DOI : https://doi.org/10.1186/s12879-024-09294-0
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Antibiogram
- Cephalosporin
- Antibiotic-Resistance
BMC Infectious Diseases
ISSN: 1471-2334
- General enquiries: [email protected]
- Download PDF
- Share X Facebook Email LinkedIn
- Permissions
Maternal Vaccine Effectiveness Against Influenza-Associated Hospitalizations and Emergency Department Visits in Infants
- 1 Department of Pediatrics, Baylor College of Medicine and Texas Children’s Hospital, Houston
- 2 Influenza Division, National Center for Immunization and Respiratory Disease, US Centers for Disease Control and Prevention, Atlanta, Georgia
- 3 Vanderbilt University Medical Center, Nashville, Tennessee
- 4 University of Pittsburg Medical Center Children’s Hospital of Pittsburgh, University of Pittsburgh School of Medicine, Pittsburgh, Pennsylvania
- 5 Seattle Children’s Research Institute, Seattle, Washington
- 6 Cincinnati Children’s Hospital Medical Center, University of Cincinnati College of Medicine, Cincinnati, Ohio
- 7 University of Missouri, Kansas City School of Medicine, Children’s Mercy Kansas City, Kansas City
- 8 University of Rochester School of Medicine and Dentistry, Rochester, New York
- 9 University of California Los Angeles Mattel Children’s Hospital, Los Angeles
- Editorial Influenza Vaccination in Pregnancy—Rolling Up Sleeves for Pregnant Persons and Infants Matthew J. Zuber, MD; April Miller, MD, MPH; Katherine A. Poehling, MD, MPH JAMA Pediatrics
Question Is maternal influenza vaccination during pregnancy associated with a reduction in influenza-associated hospitalizations and emergency department (ED) visits in infants younger than 6 months?
Findings In this case-control study of 3764 infants younger than 6 months, maternal vaccination was associated with a reduction in influenza-associated hospitalizations and ED visits in infants. Vaccine effectiveness was highest among hospitalized infants, those younger than 3 months, and those born to mothers vaccinated in the third trimester.
Meaning The findings in this study indicate that maternal influenza vaccination during pregnancy provided important protection for the infant in the first few months of life before infants are eligible for vaccination.
Importance Influenza virus infection during pregnancy is associated with severe maternal disease and may be associated with adverse birth outcomes. Inactivated influenza vaccine during pregnancy is safe and effective and can protect young infants, but recent evidence, particularly after the 2009 novel influenza A (H1N1) pandemic, is limited.
Objective To evaluate the effectiveness of influenza vaccination during pregnancy against laboratory-confirmed influenza-associated hospitalizations and emergency department (ED) visits in infants younger than 6 months.
Design, Setting, and Participants This was a prospective, test-negative case-control study using data from the New Vaccine Surveillance Network from the 2016 to 2017 through 2019 to 2020 influenza seasons. Infants younger than 6 months with an ED visit or hospitalization for acute respiratory illness were included from 7 pediatric medical institutions in US cities. Control infants with an influenza-negative molecular test were included for comparison. Data were analyzed from June 2022 to September 2023.
Exposure Maternal influenza vaccination during pregnancy.
Main Outcomes and Measures We estimated maternal vaccine effectiveness against hospitalizations or ED visits in infants younger than 6 months, those younger than 3 months, and by trimester of vaccination. Maternal vaccination status was determined using immunization information systems, medical records, or self-report. Vaccine effectiveness was estimated by comparing the odds of maternal influenza vaccination 14 days or more before delivery in infants with influenza vs those without.
Results Of 3764 infants (223 with influenza and 3541 control infants), 2007 (53%) were born to mothers who were vaccinated during pregnancy. Overall vaccine effectiveness in infants was 34% (95% CI, 12 to 50), 39% (95% CI, 12 to 58) against influenza-associated hospitalizations, and 19% (95% CI, −24 to 48) against ED visits. Among infants younger than 3 months, effectiveness was 53% (95% CI, 30 to 68). Effectiveness was 52% (95% CI, 30 to 68) among infants with mothers who were vaccinated during the third trimester and 17% (95% CI, −15 to 40) among those with mothers who were vaccinated during the first or second trimesters.
Conclusions and Relevance Maternal vaccination was associated with reduced odds of influenza-associated hospitalizations and ED visits in infants younger than 6 months. Effectiveness was greatest among infants younger than 3 months, for those born to mothers vaccinated during the third trimester, and against influenza-associated hospitalizations.
- Editorial Influenza Vaccination in Pregnancy—Rolling Up Sleeves for Pregnant Persons and Infants JAMA Pediatrics
Read More About
Sahni LC , Olson SM , Halasa NB, et al. Maternal Vaccine Effectiveness Against Influenza-Associated Hospitalizations and Emergency Department Visits in Infants. JAMA Pediatr. 2024;178(2):176–184. doi:10.1001/jamapediatrics.2023.5639
Manage citations:
© 2024
Artificial Intelligence Resource Center
Pediatrics in JAMA : Read the Latest
Browse and subscribe to JAMA Network podcasts!
Others Also Liked
Select your interests.
Customize your JAMA Network experience by selecting one or more topics from the list below.
- Academic Medicine
- Acid Base, Electrolytes, Fluids
- Allergy and Clinical Immunology
- American Indian or Alaska Natives
- Anesthesiology
- Anticoagulation
- Art and Images in Psychiatry
- Artificial Intelligence
- Assisted Reproduction
- Bleeding and Transfusion
- Caring for the Critically Ill Patient
- Challenges in Clinical Electrocardiography
- Climate and Health
- Climate Change
- Clinical Challenge
- Clinical Decision Support
- Clinical Implications of Basic Neuroscience
- Clinical Pharmacy and Pharmacology
- Complementary and Alternative Medicine
- Consensus Statements
- Coronavirus (COVID-19)
- Critical Care Medicine
- Cultural Competency
- Dental Medicine
- Dermatology
- Diabetes and Endocrinology
- Diagnostic Test Interpretation
- Drug Development
- Electronic Health Records
- Emergency Medicine
- End of Life, Hospice, Palliative Care
- Environmental Health
- Equity, Diversity, and Inclusion
- Facial Plastic Surgery
- Gastroenterology and Hepatology
- Genetics and Genomics
- Genomics and Precision Health
- Global Health
- Guide to Statistics and Methods
- Hair Disorders
- Health Care Delivery Models
- Health Care Economics, Insurance, Payment
- Health Care Quality
- Health Care Reform
- Health Care Safety
- Health Care Workforce
- Health Disparities
- Health Inequities
- Health Policy
- Health Systems Science
- History of Medicine
- Hypertension
- Images in Neurology
- Implementation Science
- Infectious Diseases
- Innovations in Health Care Delivery
- JAMA Infographic
- Law and Medicine
- Leading Change
- Less is More
- LGBTQIA Medicine
- Lifestyle Behaviors
- Medical Coding
- Medical Devices and Equipment
- Medical Education
- Medical Education and Training
- Medical Journals and Publishing
- Mobile Health and Telemedicine
- Narrative Medicine
- Neuroscience and Psychiatry
- Notable Notes
- Nutrition, Obesity, Exercise
- Obstetrics and Gynecology
- Occupational Health
- Ophthalmology
- Orthopedics
- Otolaryngology
- Pain Medicine
- Palliative Care
- Pathology and Laboratory Medicine
- Patient Care
- Patient Information
- Performance Improvement
- Performance Measures
- Perioperative Care and Consultation
- Pharmacoeconomics
- Pharmacoepidemiology
- Pharmacogenetics
- Pharmacy and Clinical Pharmacology
- Physical Medicine and Rehabilitation
- Physical Therapy
- Physician Leadership
- Population Health
- Primary Care
- Professional Well-being
- Professionalism
- Psychiatry and Behavioral Health
- Public Health
- Pulmonary Medicine
- Regulatory Agencies
- Reproductive Health
- Research, Methods, Statistics
- Resuscitation
- Rheumatology
- Risk Management
- Scientific Discovery and the Future of Medicine
- Shared Decision Making and Communication
- Sleep Medicine
- Sports Medicine
- Stem Cell Transplantation
- Substance Use and Addiction Medicine
- Surgical Innovation
- Surgical Pearls
- Teachable Moment
- Technology and Finance
- The Art of JAMA
- The Arts and Medicine
- The Rational Clinical Examination
- Tobacco and e-Cigarettes
- Translational Medicine
- Trauma and Injury
- Treatment Adherence
- Ultrasonography
- Users' Guide to the Medical Literature
- Vaccination
- Venous Thromboembolism
- Veterans Health
- Women's Health
- Workflow and Process
- Wound Care, Infection, Healing
- Register for email alerts with links to free full-text articles
- Access PDFs of free articles
- Manage your interests
- Save searches and receive search alerts
- Skip to primary navigation
- Skip to main content
- Skip to primary sidebar
information for practice
news, new scholarship & more from around the world
- gary.holden@nyu.edu
- @ Info4Practice
Emergency department care experiences among people who use substances: a qualitative study
People who use substances (PWUS) encounter significant barriers to accessing care for their complex health needs. As a result, emergency departments (EDs) often become the first point of healthcare access for …
Read the full article ›
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- v.11(9); 2021

Understanding diagnostic processes in emergency departments: a mixed methods case study protocol
Michelle daniel.
1 Emergency Medicine, University of California San Diego School of Medicine, La Jolla, California, USA
SunYoung Park
2 School of Art and Design and School of Information, University of Michigan, Ann Arbor, Michigan, USA
Colleen M Seifert
3 Psychology, University of Michigan, Ann Arbor, Michigan, USA
P Paul Chandanabhumma
4 Family Medicine, University of Michigan, Ann Arbor, Michigan, USA
Michael D Fetters
Eric wilson.
5 Emergency Medicine, University of Michigan, Ann Arbor, Michigan, USA
Andrew B Canvasser
Hardeep singh.
6 Houston Veterans Affairs Center for Innovations in Quality, Effectiveness and Safety, Michael E. DeBakey Veterans Affairs Medical Center, Houston, Texas, USA
7 Department of Medicine, Baylor College of Medicine, Houston, Texas, USA
Kalyan Pasupathy
8 Mayo Clinic Department of Health Sciences Research, Rochester, Minnesota, USA
Prashant Mahajan
9 Emergency Medicine and Pediatrics, University of Michigan, Ann Arbor, Michigan, USA
Associated Data
bmjopen-2020-044194supp001.pdf
Introduction
Diagnostic processes in the emergency department (ED) involve multiple interactions among individuals who interface with information systems to access and record information. A better understanding of diagnostic processes is needed to mitigate errors. This paper describes a study protocol to map diagnostic processes in the ED as a foundation for developing future error mitigation strategies.
Methods and analysis
This study of an adult and a paediatric academic ED uses a prospective mixed methods case study design informed by an ED-specific diagnostic decision-making model (the modified ED-National Academies of Sciences, Engineering and Medicine (NASEM) model) and two cognitive theories (dual process theory and distributed cognition). Data sources include audio recordings of patient and care team interactions, electronic health record data, observer field notes and stakeholder interviews. Multiple qualitative analysis methods will be used to explore diagnostic processes in situ, including systems information flow, human–human and human–system interactions and contextual factors influencing cognition. The study has three parts. Part 1 involves prospective field observations of patients with undifferentiated symptoms at high risk for diagnostic error, where each patient is followed throughout the entire care delivery process. Part 2 involves observing individual care team providers over a 4-hour window to capture their diagnostic workflow, team coordination and communication across multiple patients. Part 3 uses interviews with key stakeholders to understand different perspectives on the diagnostic process, as well as perceived strengths and vulnerabilities, in order to enrich the ED-NASEM diagnostic model.
Ethics and dissemination
The University of Michigan Institutional Review Board approved this study, HUM00156261. This foundational work will help identify strengths and vulnerabilities in diagnostic processes. Further, it will inform the future development and testing of patient, provider and systems-level interventions for mitigating error and improving patient safety in these and other EDs. The work will be disseminated through journal publications and presentations at national and international meetings.
Strengths and limitations of this study
- Prospective, observational studies informed by theory which explore diagnostic processes in situ are uncommon, yet urgently needed to improve understanding of emergency department (ED) diagnosis.
- Study findings will provide critical, contextualised knowledge of how ED diagnosis and management is accomplished through interactions of patients, providers and tools, informing the design of interventions to mitigate error.
- A transdisciplinary team including safety experts, data scientists, systems engineers, cognitive psychologists and emergency physicians contributed to this mixed methods study design.
- The focus on one adult and one paediatric academic ED is methodologically critical to achieve a deep understanding of cognition in context, but may limit transferability to other settings.
Diagnosis and management of patients in emergency departments (EDs) involves highly complex cognitive processes under time pressure that are susceptible to errors, which we define as missed opportunities for improving diagnosis, regardless of patient outcomes. 1 While precise error rates are unknown, a conservative estimate of 5% of the 139 million ED visits annually suggests ~6.9 million errors per year. 2 Errors typically result from a complex interplay of factors arising from patients (eg, presenting symptoms, health literacy, disease complexity, behaviours), provider/care-team performance (eg, cognitive load, information gathering and synthesis, coordination) and systems (eg, health information technology, overcrowding, interruptions). 3 Current methods to study errors are suboptimal as they largely focus on retrospective analyses of what went wrong rather than understanding and contextualising diagnostic processes as they occur in the ED. Novel prospective studies are urgently needed to improve the understanding of ED diagnostic processes and to facilitate the development of interventions to improve patient safety.
We assembled a transdisciplinary team with expertise in emergency medicine, cognitive psychology, informatics, systems engineering, human–computer interaction (HCI) and design, anthropology, public health, mixed methods research and data science to address this gap. With support from the Agency for Healthcare Research and Quality, we are creating an Improving Diagnosis in Emergency and Acute Care—Learning Laboratory (IDEA-LL) to investigate ED diagnostic processes, study systems vulnerabilities and develop and iteratively test patient, provider and system-oriented interventions to mitigate diagnostic error. The three aims of the parent project (IDEA-LL) are shown in figure 1 .

Improving Diagnosis in Emergency and Acute Care—Learning Laboratory (IDEA-LL) Aims. ED, emergency department; EHR, electronic health record.
Patients that present to the ED often have complex and ambiguous problems that may not result in a ‘diagnosis’ if diagnosis is narrowly conceived of as a ‘label’ or solution to a problem. For the purposes of this study, we will operationalise diagnosis as an ongoing, sense-making process with inherent uncertainty as described by Ilgen et al . 4 Furthermore, we will use the term ‘diagnostic processes’ to encompass both diagnosis and related management processes.
Conceptual models of diagnostic and management reasoning typically break the process down into multiple components (eg, information gathering, hypothesis formation, differential diagnosis generation, development of a treatment plan). 5 A model recently proposed by the National Academies of Sciences, Engineering and Medicine (NASEM) incorporates these dynamic components and links diagnosis and management by healthcare teams to patient and system outcomes in a feedback loop. 3 This model, recently adapted by ED experts into the modified ED-NASEM model, 6 provides an overarching framework for exploring diagnostic processes in the current study.
Two complementary theories of human cognition also inform this work: dual process theory 7 and distributed cognition theory . 8 Dual process theory characterises information processing as it occurs ‘in the head’ of an individual. This theory holds that clinicians process information via two primary pathways: system 1 (pattern recognition) and system 2 (analytical thinking), and that experts switch back and forth between these two systems. 9 10 Inappropriate reliance on either system can result in errors. 11 12 Distributed cognition theory views information processing as occurring ‘out in the world’. 8 Cognitive tasks such as diagnosis are accomplished through their distribution across multiple individuals (eg, patients, nurses, physicians), external tools (eg, electronic health record (EHR), computer-based searches, medical devices), spatial arrangements and time. 13 Many of these tasks occur outside of the diagnosing clinician’s purview, including the prehospital setting and after patient disposition. Collaborative systems of people and tools (also known as ‘artefacts’) implement dynamic processes constituting a shared cognitive system to create a diagnosis, with breakdowns anywhere in the system potentially leading to error. 14–18 Individual cognitive processes ‘in the head’ are difficult to access in real time and must be inferred through observation or questioning; however, information processing in a distributed cognition system is more readily accessible through observation of interactions ‘out in the world’, which informs our study design.
This paper describes our three-part approach for sub-aims 1.1 and 1.2 in IDEA-LL, which focuses on using systems engineering and cognitive theories to explore ED diagnostic processes, as well as vulnerabilities that may lead to error . The purpose of parts 1 and 2 is to prospectively explore ED diagnostic processes and to understand the distributed cognitive system supporting diagnosis in everyday ED practice. The purpose of part 3 is to elaborate on and enrich the modified ED-NASEM model and to examine perceived strengths and vulnerabilities in emergency care diagnostic processes.
This work will use a prospective mixed methods case study design 19 20 to collect quantitative and qualitative data in an adult and a paediatric ED. We will use both process measures (ie, tracking specific steps leading to diagnosis including interactions with tools, communications between people and monitoring elapsed time), and multiple qualitative methods (eg, field observations, cognitive ethnography, 21 interviews) to map information capture, transfer and sharing among patients and providers leading to diagnosis. Data collection will occur December 2020–December 2021. An overview of the proposed studies appears in table 1 .
Overview of the proposed studies for sub-aims 1.1 and 1.2
ED, emergency department; NASEM, National Academies of Sciences, Engineering and Medicine.
Our data collection procedures, in accordance with distributed cognition theory, 8 13 will primarily focus on direct observations ‘out in the world’ as diagnosis unfolds within the sociocultural settings of two EDs. We will record how cognitive work is distributed across people and tools in context by recording interactions and documenting its organisation across physical space and time. In addition, we will elucidate individual cognition by obtaining provider responses to brief mini-interviews during clinical work. As interruptions can add to provider cognitive load and potentially alter diagnostic performance, we will conduct interviews opportunistically to minimise interruptions in patient care.
Parts 1, 2 and 3 will be conducted in a single academic tertiary care setting with an adult and a paediatric ED. These EDs serve an urban area (population ~120 000), in addition to a large suburban and rural catchment area. Both EDs are level I trauma centres, with a total annual census of 106 470 visits (74 034 adult and 32 436 paediatric). The EDs have 110 beds (88 adult and 22 paediatric), augmented by hallway and recliner space. The EDs are staffed by ~65 attending physicians, ~64 residents, ~40 advanced practice providers and ~380 nurses. Resident trainees include postgraduate years (PGY) 1–4 with 16 residents per class, and ~170 medical students rotate through the department annually on a 1-month required clerkship. According to health system policy, patients up to age 21 may be seen in the paediatric ED, however, patients ages 18–21 account for a small percentage of the total paediatric population (ie, ~5%).
Sampling, eligibility, recruitment, informed consent and data collection
Part 1: individual patient case as the unit of observation.
We will use purposive sampling of patients presenting to the ED who are at higher risk for diagnostic mishaps such as those with undifferentiated symptoms of abdominal pain, fever, chest pain or shortness of breath. 22–27 While data has linked chest pain symptoms with a wide range of never-miss conditions, 23 27 limited research has explored shortness of breath and never-miss conditions. Both symptoms will be included as they represent undifferentiated symptoms commonly seen in the ED that have been associated with missed diagnosis. We anticipate a minimum sample size of 24 patients based on previous observational studies in medicine. 28 The final sample size will be determined when adequate conceptual depth has been achieved in the findings. 29
Eligibility
Eligible adult patients will be 21 or older and capable of giving informed consent. Eligible paediatric patients will be between 0 and 21 years of age and their legally authorised representative must be capable of giving informed consent. For paediatric patients 13 years of age or older, assent will also be required. We will exclude non-English speaking patients and those with altered mental status due to limitations of obtaining informed consent.
Recruitment of patients
We will enrol patients with three types of undifferentiated presenting symptoms associated with a ‘high-risk’ for diagnostic errors, namely chest pain, shortness of breath and abdominal pain. Working in collaboration with the triage nurse as patients register, research personnel will identify potentially eligible patients at triage. We have a waiver for screening patients for eligibility and capturing initial information exchange prior to approaching for informed consent and enrolment. Informed consent will be conducted once triage is complete. After the patient is roomed, the researcher will notify the care team that the patient has been enrolled in the study. Enrolment will occur during varied ED clinical shifts over a period of 6 months. Participation will be completely voluntary and uncompensated.
Informed consent
Eligibility will be assessed by study personnel. Once determined eligible, patients (and any family or visitors present) will be asked for written informed consent. All primary providers associated with the patient will also be asked for informed consent. Consent from providers will largely be obtained prior to field observations via email, to minimise disruption.
Data collection
A small team of trained observers comprised of qualitative researchers and healthcare engineers will collect the qualitative data. These individuals do not have a background in emergency medicine, and thus no association with a particular professional role that might introduce bias into data collection.
Patient care trajectory assessment
Two observers will work together to follow the diagnostic processing of a patient case from triage to disposition. Since distributed cognition theory focuses on how information flows in interactions, one observer will follow the patient to capture interactions that occur at or near the patient’s bedside. The second observer will follow the ED provider(s) (typically a resident or physician assistant) to capture events related to the care that occurs away from the patient’s bedside. Both observers will use audio recording devices to capture verbatim information exchange. Phone calls are not recorded, so observers will directly query providers about the content of calls. We will capture patient–provider and provider–care team interactions to examine relationships between information input, output and the representation of information in various artefacts, to assess gaps in information exchange among patient, provider and care team members.
Observational data
Observers will use data collection forms developed through pilot observations. These forms will track approximate timing of events to allow for quantification of interactions (eg, communication between care providers and the patient or other providers, estimated duration of events, time spent using tools). Observers will also take extensive field notes first as jottings in the field, then expanded afterwards to full field observations. They will record their inferences and reflections in memos focused on context, content and concepts. 30
Time in care measures
Observational data will be supplemented by information available through the time-stamped EHR (eg, total time in ED, time from arrival to triage, time to room, time to provider, time to intervention (eg, medications, fluids), time to test performance, time from when results are available to when they are reviewed, time when patient data and diagnoses are recorded in the EHR and viewed by care team members).
Mini-interviews
Observers will briefly probe care team members to capture their thought processes during diagnostic work. At the end of the patient observation, the observers will ask patients and providers their perspectives on the complete diagnostic process and any strengths and vulnerabilities from their perspectives.
Part 2: ED provider as the unit of observation
Different contexts and team configurations can influence how cognition is distributed across ED providers and artefacts. 8 10 Thus, we will intentionally sample across different shifts (eg, day, evening, night) and work areas in the EDs to capture a range of patient volumes and staffing models. We will recruit attending physicians, residents, physician assistants and nurses to explore how different roles engage in the ED diagnostic process. These roles represent the core members of ED patient care teams, and intentional sampling by role will help us construct a 360-degree view of distributed cognition. This will allow us to discern how information flows and is processed in the system through interactions with people and artefacts. We anticipate a minimum of 24 provider observations. As in part 1, the final sample size will be determined by attainment of adequate conceptual depth. 29
Eligible providers will be directly involved in patient care. Attending physicians, physician assistants and nurses will have a minimum of 1 year’s experience working in the ED setting. Residents may be PGY 1–4.
Recruitment of providers
Providers will be recruited via email in advance of a shift or in person on the day of a shift by study personnel.
We will obtain informed consent of providers. Providers that refuse participation will not be observed. We anticipate these providers will come into contact with multiple patients and other providers as part of their routine work practices. We will provide an Institutional Review Board (IRB) approved information sheet to ‘incidental contacts’ notifying individuals that the information and communication will be recorded and collected for the purposes of research.
Observations
In part 2, we will shadow ED providers caring for multiple patients over a 4-hour time frame, ensuring capture of either beginning-of-shift or end-of-shift handovers. The provider observations will occur on different days than the patient case observations. Observers will follow a provider as they go about their work routine, communicating with other providers, accessing medical records, sending or answering pages, dictating or writing notes, accessing resources outside the ED, providing instruction to other care team members and so on. Audio recordings will supplement observer field notes to capture the detailed content of information-dense interactions. When providers are interacting with patients, only handwritten notes will be collected. Patients may decline the presence of the observer at any time.
In part 2, the focus is the interactions of people and tools within the sociocultural and sociotechnical context of the ED. In line with distributed cognition theory, observations will document exchanges between primary clinicians with patients, family or visitors, care team members and consultants and others over the 4-hour time frame. Additionally, we will collect details on how clinicians organise their patient cases and digital tools. 31 This study of interactions will capture the questions, orders, instruction, information sharing and recording, corrections, interruptions, workload demands, team dynamics and communication patterns over several hours of a shift. 11 In addition to audio recording, observers will use data collection forms, open-ended field notes and reflexive memos. Notations will be made of contextual factors such as overall ED volume and the number of patients a provider is concurrently managing. We will also capture use of artefacts such as paper or electronic notes used by providers.
During our observations, we will prompt providers to verbalise their thinking at key moments. At the end of the shift, the handover process between providers will be observed, and then individual providers will be briefly interviewed about their impressions of the diagnostic process over that shift.
Potential impact of mini-interviews and observations
In both parts 1 and 2 of this study, we acknowledge that the presence of researchers in the EDs could impact both thinking, that is, cognition and behaviour. By conducting mini-interviews, we could inadvertently alter participants thinking (by promoting synthesis), or at the very least make thinking more conscious. By having observers present, we could alter participant reactions per the ‘Hawthorne effect’, however, such alterations in behaviour have largely been shown to be insignificant. 32
Part 3: interviews with key stakeholders
We plan to conduct semi-structured interviews with attending physicians, residents/advanced practice providers, nurses, prehospital providers and patients. Groups will be purposively sampled based on roles and their experience with diagnostic processes. We anticipate a minimum of 20 interviews.
Eligible providers will be those involved in patient care with a minimum of 1 year’s experience working in or consulting in the ED. Eligible patients or legally authorised representatives will be English-speaking, capable of providing informed consent and have visited the ED within 2–3 weeks preceding the interview.
Recruitment of patients and providers
Patients will be recruited by a study coordinator prior to discharge or admission during their index ED visit. We will also use the patient recruitment portal ( https://umhealthresearch.org/ ). Providers will be recruited through email. A US$25 gift card will be provided to patients/caregivers as compensation for their time.
We will obtain informed consent from all patients, legally authorised representatives and provider participants.
Data collection instrument
An interview guide will be developed using distributed cognition theory and guided by the modified ED-NASEM model 6 of diagnosis. (Please see online supplemental appendix 1 for details of the interview guide.) Questions will direct participants to reflect on their own experiences with ED diagnostic processes. Probes will focus on elucidating key points of interaction among people, artefacts and systems for diagnosis, depicting how information flows through the system, emphasising activities that contribute to or inhibit timely diagnosis and highlighting perceptions of key points that lead to breakdowns and errors.
Supplementary data
Data collection process.
At the beginning of each session, we will brief participants on the nature of the study, explain the format of the session and establish a safe environment for information disclosure. Each interview will be recorded and last approximately 60 min.
Qualitative data entry and cleaning
Recordings from observations and interviews will be transcribed verbatim and stored in a secure location in accordance with IRB procedures. Only de-identified data will be made available to the broader research team. All qualitative data, including field observation notes and transcriptions, will be entered into and analysed using MaxQDA. Time stamped data and other quantitative measures will be entered first into excel, and then exported into SPSS.
Data analysis
Based on the research questions for each part, we will use both inductive and deductive analysis methods, with the latter shaped by the theories previously mentioned. The mixed data analysis will be qualitatively driven; that is, the quantitative measures will play a supportive role relative to an overarching qualitative analysis. 33 34 These mixed data will be merged in response to emerging findings where timing could frame and enhance understanding of qualitatively elucidated information. We will begin iterative data analysis during the data collection process. We will employ both qualitative and quantitative codes for the transcripts, field observation notes and mini-interviews from parts 1 and 2. Quantitative codes will characterise observed behaviours by counting the number and duration of interactions between people or artefacts, event occurrences (eg, pages, consults), dialogue analyses and other behaviours through the calculation of descriptive statistics.
Emergent themes will be identified and added as codes using an open coding method 35 to look for recurring themes. In the open coding method, two to three researchers from different professional backgrounds will analyse the transcripts and participant observation data following techniques described by Marshall and Rossman. 36 Since inductive analysis values the subjectivity of researchers as they make meaning from data, the backgrounds of the study team members conducting the analysis are important: MD and PM are emergency physicians who work in the adult and paediatric EDs under study; CMS is a cognitive psychologist who has a strong background in distributed cognition theory; PPC and MDF are experts in qualitative methodology; and SYP is an expert in HCI, design and complex systems. Each researcher will review a set of initial transcripts independently and code the content of each transcript. Each analyst will independently and continuously compare each incident, event, quote and instance to look for similarities and differences. The researchers will discuss, compare and reconcile differences in coding and create a consensus code template, which will then be used to code the remainder of transcripts. Weekly discussions will be held to interpret the meanings and themes from the beginning of the analysis.
During the data analysis, we will discuss emerging findings or questions with participants through a series of informal conversations to clarify any misconceptions and verify the validity of the themes identified in this study as another form of member checking. 37 To increase the reliability of our findings, we will then triangulate by comparing and contrasting data obtained via interviews and observations. Data collection will end when reasonable conceptual depth 29 has been achieved in the findings. Code reliability will be examined through independent coder comparisons, and differences resolved to consensus.
Integration of the quantitative findings into the analyses will occur through the use of joint display analysis where the quantitative data will be linked with related qualitative findings. 38 39 Additional targeted inquiries will be made of these data based on the emerging themes from the quantitative analysis. We will use multiple diagramming methods 40 (eg, communication, shared spaces, information flow, timelines) to map the process of ED diagnostic work practices. These descriptive data analyses will help develop a comprehensive map of the diagnostic process, identify factors that lead to potential breakdowns and design requirements that will guide our intervention design phase in aim 2 of the larger IDEA-LL study.
Comparison of the adult and the paediatric EDs within the same institutional context will allow the examination of differences such as patient age, illness, interactions, sociocultural context or physical layout that lead to differences in diagnostic processes. These analyses will help us construct a detailed map of the distributed diagnostic processes in the two EDs by identifying when and how key information is introduced, gathered, assembled, communicated, transferred and applied.
Patient and public involvement
To ensure our research focuses on issues relevant to patients and the public, patients will be involved at multiple stages. Part 1 focuses on individual patients with undifferentiated symptoms as they experience the diagnostic process. In part 2, although our focus is on providers treating multiple patients simultaneously, patients will again be invited to participate. Part 3 will include interviews with patients and caregivers so that we may learn from their experiences and solicit their insights on challenges and vulnerabilities in ED diagnostic processes. Thus, parts 1–3 ensure the patient experience will inform the development of future interventions to improve diagnosis.
Many aspects of the ED diagnostic process unfold within an increasingly information-rich environment that is poorly understood, resulting in limited knowledge about how to improve patient safety. Our study findings will shed new light on strengths and vulnerabilities in ED diagnostic processes. 31
A strength of this protocol is the interdisciplinary team that contributed to its development. Team members brought diverse perspectives on conceptual and theoretical models to guide data collection and analysis. Multiple study designs were considered to elucidate facets of cognition and sociotechnical/sociocultural work, and we chose to emphasise interaction processes, allowing us to prospectively learn from ‘what went wrong’ as well as ‘what went right’. 41 This shift in safety perspective has been recently highlighted as critical to understanding and reducing errors. Multilevel qualitative and semi-quantitative data analysis will enable a comprehensive and deep understanding of a distributed system, providing opportunities to examine how information is gathered and interpreted in the diagnostic process.
Another strength of this protocol is the integration of complementary models and theories to guide our data collection and analyses. An exclusive focus on dual process theory or distributed cognition (as is the case with many studies) misses out on the opportunity to appreciate simultaneously occurring processes (ie, what’s ‘in the head’ and ‘out in the world’). These theories will be leveraged to enrich the current modified ED-NASEM model of the diagnostic process, which currently implicitly incorporates some aspects of these theories, but does not do so explicitly.
To our knowledge, there have been few studies that use intensive, qualitatively driven mixed method approaches to examine ED diagnostic processes. Conducting in situ observations of the entire ED care delivery process, focused on individual patients and provider workflow, including physical workflow, documentation workflow, communication workflow and cognitive processes is particularly unique. This study will be one of the first to offer empirical data about how information is gathered, exchanged, recorded and used at the individual, team and system level, highlighting challenges and breakdowns that potentially lead to diagnostic errors in real-world emergency care settings.
This study design with two EDs in the same institutional setting holds constant the impact of certain system and community factors on ED diagnostic processes. Due to the many social and cultural factors influencing ED performance, focusing on two similarly situated EDs can improve our ability to observe system factors (eg, providers’ workflow, system workflow, interruptions, impacts of triage policies and ED care procedures). Additionally, a comparison between two EDs within the adult and paediatric settings allows differences in their diagnostic approaches to become salient.
As case study research, we will examine in great depth an adult and a paediatric ED in a single hospital system. While methodologically critical to achieve deep understanding of cognition in context, this may limit transferability. Further studies under the larger IDEA-LL study will compare ED systems in other settings.
Our findings will provide critical knowledge regarding how diagnostic processes occur across interactions of adult and paediatric patients, providers, care teams and tools in EDs. Findings will help identify opportunities for improving diagnostic processes, particularly those at risk of error in ED work systems. Finally, the results will inform intervention design for mitigating errors in the subsequent aims of IDEA-LL. This is the first step in our study to develop safer diagnostic processes in the ED that prevent patient harm.
Ethical approval for this study has been granted by the University of Michigan IRB (HUM00156261). We plan to share our results in peer-reviewed publications and national/international research platforms, however, we will not share identifying patient/provider information with anyone who is not approved by the IRB.
Supplementary Material
Acknowledgments.
The investigators would like to thank Elizabeth Duffy, MA and Sarah Parker, MPH, for their invaluable support throughout the protocol design process.
Correction notice: This article has been corrected since it was published. Author 'Andrew B Canvasser' has been included in the article.
Contributors: All authors participated in multiple team discussions to conceptualize the manuscript and to refine the methodologies. MD was the primary author of the manuscript with significant text refinement provided by SYP, EW, AC, KP, CMS, PPC, MDF, and PM. In particular, MD, HS, EW and CMS provided the theoretical framing, and CMS, AC, SYP, PPC, KP and MDF contributed methodological expertise. Data analysis a will be conducted by MD, CMS, HS, SYP, PPC, MDF and PM, with all authors contributing to interpretation of the findings. All authors read and approved the final manuscript.
Funding: This project was supported by grant number R18HS026622 from the Agency for Healthcare Research and Quality. The content is solely the responsibility of the authors and does not necessarily represent the official views of the Agency for Healthcare Research and Quality. Dr Singh is funded in part by the Houston Veterans Administration (VA) Health Services Research and Development (HSR&D) Centre for Innovations in Quality, Effectiveness and Safety (CIN13-413), the VA HSR&D Service (CRE17-127 and the Presidential Early Career Award for Scientists and Engineers USA 14–274), the VA National Centre for Patient Safety, the Agency for Healthcare Research and Quality (R01HS27363), the CanTest Research Collaborative funded by a Cancer Research UK Population Research Catalyst award (C8640/A23385) and the Gordon and Betty Moore Foundation.
Competing interests: None declared.
Provenance and peer review: Not commissioned; externally peer reviewed.
Supplemental material: This content has been supplied by the author(s). It has not been vetted by BMJ Publishing Group Limited (BMJ) and may not have been peer-reviewed. Any opinions or recommendations discussed are solely those of the author(s) and are not endorsed by BMJ. BMJ disclaims all liability and responsibility arising from any reliance placed on the content. Where the content includes any translated material, BMJ does not warrant the accuracy and reliability of the translations (including but not limited to local regulations, clinical guidelines, terminology, drug names and drug dosages), and is not responsible for any error and/or omissions arising from translation and adaptation or otherwise.
Ethics statements
Patient consent for publication.
Not applicable.

An official website of the Department of Health & Human Services
- Search All AHRQ Sites
- Email Updates

1. Use quotes to search for an exact match of a phrase.
2. Put a minus sign just before words you don't want.
3. Enter any important keywords in any order to find entries where all these terms appear.
- The PSNet Collection
- All Content
- Perspectives
- Current Weekly Issue
- Past Weekly Issues
- Curated Libraries
- Clinical Areas
- Patient Safety 101
- The Fundamentals
- Training and Education
- Continuing Education
- WebM&M: Case Studies
- Training Catalog
- Submit a Case
- Improvement Resources
- Innovations
- Submit an Innovation
- About PSNet
- Editorial Team
- Technical Expert Panel
Organizational learning starting points and presuppositions: a case study from a hospital’s surgical department.
Jaakkola M, Lemmetty S, Collin K, et al. Organizational learning starting points and presuppositions: a case study from a hospital’s surgical department. Learn Org. 2024;31(3):337-357. doi:10.1108/tlo-12-2022-0160.
Organizational learning is a continuous process of integrating data and knowledge to ensure improvement. This qualitative study focuses on the starting points and presuppositions of organizational learning within a surgical department. Starting points for individual learning were informal and based on day-to-day work (e.g., solving a specific problem) and organizational learning encompassed more formal and intentional practices. Factors presupposing and framing the learning process can be divided into four categories: leadership and roles, practices and resources, collaboration and climate, and motivation and activity.
Safety checklists for emergency response driving and patient transport: experiences from emergency medical services. July 7, 2021
Registered nurses' and medical doctors' experiences of patient safety in health information exchange during interorganizational care transitions: a qualitative review. November 10, 2021
Interorganizational health information exchange-related patient safety incidents: a descriptive register-based qualitative study. May 24, 2023
Register-based research of adverse events revealing incomplete records threatening patient safety. August 19, 2020
Reporting of health information technology system-related patient safety incidents: the effects of organizational justice. October 6, 2021
An analysis of electronic health record–related patient safety incidents. March 30, 2016
Preventable adverse drug events and their causes and contributing factors: the analysis of register data. February 16, 2011
Adverse events and near misses relating to information management in a hospital. June 22, 2016
COVID-19 has united patients and providers against institutional betrayal in health care: a battle to be heard, believed, and protected. August 19, 2020
Racial disparities in diagnostic delay among women with breast cancer. August 18, 2021
Frequency and severity of parenteral nutrition medication errors at a large children's hospital after implementation of electronic ordering and compounding. August 19, 2015
Weaving a healthcare tapestry of safety and communication. July 16, 2014
Does overlapping surgery result in worse surgical outcomes? A systematic review and meta-analysis. February 20, 2019
Optimizing Pediatric Patient Safety in the Emergency Care Setting. October 19, 2022
Detecting medication administration errors. September 18, 2019
The randomized AMBORA trial: impact of pharmacological/pharmaceutical care on medication safety and patient-reported outcomes during treatment with new oral anticancer agents. April 21, 2021
Nurse burnout predicts self-reported medication administration errors in acute care hospitals. January 20, 2021
A standardized formulary to reduce pediatric medication dosing errors: a mixed methods study. October 6, 2021
Errors in nurse-led triage: an observational study. December 2, 2020
Addressing mistreatment of providers by patients and family members as a patient safety event. February 16, 2022
Prescribing errors in post-COVID-19 patients: prevalence, severity, and risk factors in patients visiting a post-COVID-19 outpatient clinic. March 23, 2022
Health care quality and safety in a correctional system: creating goals and performance measures for improvement. August 17, 2022
Surgeon's narcissism, hostility, stress, bullying, meaning in life and work environment: a two-centered analysis. September 27, 2023
Patients' experiences and perspectives of patient-reported outcome measures in clinical care: a systematic review and qualitative meta-synthesis. May 11, 2022
Tools for establishing a sustainable safety culture within maternity services: a retrospective case study. April 26, 2023
How health care systems let our patients down: a systematic review into suicide deaths. July 1, 2020
Organizational and social-psychological conditions in healthcare and their importance for patient and staff safety. A critical incident study among doctors and nurses. January 21, 2015
Relationship of adverse events and support to RN burnout. October 8, 2014
Preventable mortality after common urological surgery: failing to rescue? September 3, 2014
Identifying facilitators and barriers for patient safety in a medicine label design system using patient simulation and interviews. July 23, 2014
Identifying high-risk medication: a systematic literature review. August 13, 2014
Evaluating implementation of a rapid response team: considering alternative outcome measures. May 7, 2014
Maternal sleepiness and risk of infant drops in the postpartum period. June 12, 2019
Implementing bedside handover: strategies for change management. October 27, 2010
Clinical handover of patients arriving by ambulance to the emergency department: a literature review. October 13, 2010
The impact of organisational and individual factors on team communication in surgery: a qualitative study. December 16, 2009
Why isn't 'time out' being implemented? An exploratory study. March 31, 2010
Pediatric Readiness in the Emergency Department. November 1, 2018
Partial do-not-resuscitate orders: a hazard to patient safety and clinical outcomes? March 16, 2011
Impact of a comprehensive safety initiative on patient-controlled analgesia errors. January 12, 2011
Hamilton Acute Pain Service Safety Study: using root cause analysis to reduce the incidence of adverse events. April 2, 2014
Socio-technical issues and challenges in implementing safe patient handovers: insights from ethnographic case studies. February 12, 2014
Team safety and innovation by learning from errors in long-term care settings. August 22, 2012
Quantitative assessment of workload and stressors in clinical radiation oncology. June 13, 2012
Handing over patient care: is it just the old broken telephone game? November 9, 2011
Investigating US medical students' motivation to respond to lapses in professionalism. October 3, 2018
The relationship between patient safety climate and occupational safety climate in healthcare—a multi-level investigation. August 16, 2017
Crossing the communication chasm: challenges and opportunities in transitions of care from the hospital to the primary care clinic. March 1, 2017
Patient safety culture: the impact on workplace violence and health worker burnout. February 8, 2023
How does workplace violence-reporting culture affect workplace violence, nurse burnout, and patient safety? December 7, 2022
Misreading injectable medications—causes and solutions: an integrative literature review. April 29, 2020
Work hours, work stress, and collaboration among ward staff in relation to risk of hospital-associated infection among patients. March 25, 2009
Hand-off communication: a requisite for perioperative patient safety. November 19, 2008
Bedside handover: quality improvement strategy to "transform care at the bedside." November 12, 2008
Outreach and Early Warning Systems (EWS) for the prevention of Intensive Care admission and death of critically ill adult patients on general hospital wards. August 8, 2007
What do medical records tell us about potentially harmful co-prescribing? July 18, 2007
Potassium and phosphorus repletion in hospitalized patients: implications for clinical practice and the potential use of healthcare information technology to improve prescribing and patient safety. February 14, 2007
Patient Safety Leadership WalkRounds™ at Partners HealthCare: learning from implementation. August 10, 2005
Patient safety culture in nursing: a dimensional concept analysis. July 30, 2008
Errors in the medication process: frequency, type, and potential clinical consequences. March 6, 2005
Potentially inappropriate medication use among elderly home care patients in Europe. April 15, 2005
Emergency medical services system changes reduce pediatric epinephrine dosing errors in the prehospital setting. October 25, 2006
Critical care nurses' role in rapid response teams: a qualitative systematic review. May 22, 2024
Patients' perspectives on quality and patient safety failures: lessons learned from an inquiry into transvaginal mesh in Australia. May 8, 2024
Supporting error management and safety climate in ambulatory care practices: the CIRSforte study. May 1, 2024
Organizational learning in the morbidity and mortality conference. March 27, 2024
Inter-hospital transfer is an independent risk factor for hospital-associated infection. March 20, 2024
How do we learn about error? A cross-sectional study of urology trainees. June 28, 2023
Green Cross method in a postanaesthesia care unit: a qualitative study of the healthcare professionals' experiences after 3 years, including the COVID-19 pandemic period. June 14, 2023
Patient safety trends in 2022: an analysis of 256,679 serious events and incidents from the nation’s largest event reporting database. May 17, 2023
The relationship between patient safety culture and the intentions of the nursing staff to report a near-miss event during the COVID-19 crisis. April 5, 2023
Quality and safety: learning from the past and (re)imagining the future. March 29, 2023
Evaluation of policies limiting opioid exposure on opioid prescribing and patient pain in opioid-naive patients undergoing elective surgery in a large American health system. March 8, 2023
The incidence of opioid misuse among the surgical patients with persistent opioid use. February 8, 2023
Am I safe? An interpretative phenomenological analysis of vulnerability as experienced by patients with complications following surgery. January 18, 2023
Patients' experience of patient safety information and participation in care during a hospital stay. November 16, 2022
A health system that won't learn from its mistakes. September 21, 2022
Variation in the reporting of elective surgeries and its influence on patient safety indicators. July 6, 2022
Creating a learning health system for improving diagnostic safety: pragmatic insights from US health care organizations. June 22, 2022
Learning environments, reliability enhancing work practices, employee engagement, and safety climate in VA cardiac catheterization laboratories. April 6, 2022
Morbidity and mortality caused by noncompliance with California hospital licensure: immediate jeopardies in California hospitals, 2007-2017. March 9, 2022
Failure to rescue following emergency surgery: a FRAM analysis of the management of the deteriorating patient. February 2, 2022
Filling a gap in safety metrics: development of a patient-centred framework to identify and categorise patient-reported breakdowns related to the diagnostic process in ambulatory care. October 27, 2021
Descriptive analysis of patient misidentification from incident report system data in a large academic hospital federation. October 20, 2021
Changes in hospital-acquired conditions and mortality associated with the hospital-acquired condition reduction program. September 29, 2021
Towards safer healthcare: qualitative insights from a process view of organisational learning from failure. August 25, 2021
Reducing failures in daily medical practice: healthcare failure mode and effect analysis combined with computer simulation. June 9, 2021
Learning during crisis: the impact of COVID-19 on hospital-acquired pressure injury incidence. June 2, 2021
Assessing patient safety culture in hospital settings. June 2, 2021
Achieving zero inequity: lessons learned from patient safety. May 27, 2021
Support for healthcare professionals after surgical patient safety incidents: a qualitative descriptive study in 5 teaching hospitals. May 26, 2021
To err is system: a comparison of methodologies for the investigation of adverse outcomes in healthcare. May 5, 2021
A human factors intervention in a hospital--evaluating the outcome of a TeamSTEPPS program in a surgical ward. April 14, 2021

Connect With Us
Sign up for Email Updates
To sign up for updates or to access your subscriber preferences, please enter your email address below.
Agency for Healthcare Research and Quality
5600 Fishers Lane Rockville, MD 20857 Telephone: (301) 427-1364
- Accessibility
- Disclaimers
- Electronic Policies
- HHS Digital Strategy
- HHS Nondiscrimination Notice
- Inspector General
- Plain Writing Act
- Privacy Policy
- Viewers & Players
- U.S. Department of Health & Human Services
- The White House
- Don't have an account? Sign up to PSNet
Submit Your Innovations
Please select your preferred way to submit an innovation.
Continue as a Guest
Track and save your innovation
in My Innovations
Edit your innovation as a draft
Continue Logged In
Please select your preferred way to submit an innovation. Note that even if you have an account, you can still choose to submit an innovation as a guest.
Continue logged in
New users to the psnet site.
Access to quizzes and start earning
CME, CEU, or Trainee Certification.
Get email alerts when new content
matching your topics of interest
in My Innovations.
- Cover Letters
- Jobs I've Applied To
- Saved Searches
- Subscriptions
Marine Corps
Coast guard.
- Space Force
- Military Podcasts
- Benefits Home
- Military Pay and Money
- Veteran Health Care
- VA eBenefits
- Veteran Job Search
- Military Skills Translator
- Upload Your Resume
- Veteran Employment Project
- Vet Friendly Employers
- Career Advice
- Military Life Home
- Military Trivia Game
- Veterans Day
- Spouse & Family
- Military History
- Discounts Home
- Featured Discounts
- Veterans Day Restaurant Discounts
- Electronics
- Join the Military Home
- Contact a Recruiter
- Military Fitness
Officers with Higher Rank Get Better Care than Those with Lower Ranks at Military Hospitals, Study Finds

Officers who outrank their military physicians and personnel who have been recently promoted receive better attention and care in Defense Department health facilities than lower-ranking service members, new research on military emergency room visits has found.
The study, published Thursday in the journal Science , also found racial bias in treatment and care in military ERs, with white physicians "exerting less effort" on Black patients.
While the study also found that white physicians treated higher-ranking Black patients with more care, their treatment was still only on par with lower-ranking white patients. Black military doctors treated lower-ranking patients of either race fairly equally, the study found, but they provided high-ranking Black patients "off-the-charts" care.
Read Next: Marijuana Testing for Recruits Could End Under House's Must-Pass Defense Policy Bill
The researchers, with the University of Texas at San Antonio and Carnegie Mellon University, conducted the study to further understand implicit bias in health care in civilian settings as well as military care. Stephen Schwab, the study's co-author, said that, while bias regarding gender and race is often the subject of research, the role that power dynamics play in medical services is less understood.
The military, with its obvious rank structure, presents opportunities to understand this relationship, he said.
"The military is doing everything it can to reduce these biases. Part of it is understanding the scope of the issue. It's not just race and gender, it's also power and wealth," Schwab, a retired Army lieutenant colonel who now works at the University of Texas at San Antonio, said in an interview with Military.com on Friday.
For the study, the researchers examined data from 1.5 million emergency department visits in the military health system, looking at the rank of a patient compared with the doctor's rank and examining treatment response, including resources expended such as medical tests, imaging and certain prescriptions, and outcomes, such as hospital admissions at the time of the ER visit or within 30 days afterward.
They found that higher-ranking patients received 3.6% more physician effort and resources and were 15% less likely than lower-ranking patients to have poor outcomes.
Lower-ranking patients seen by doctors attending to higher-ranking patients at the same time were 3.4% more likely to have poorer outcomes, according to the study.
"Our findings indicate that power confers nontrivial advantages: 'High-power' patients (who outrank their physician) receive more resources and have better outcomes than equivalently ranked 'low-power' patients. Patient promotions even increase physician effort. Furthermore, low-power patients suffer if their physician concurrently cares for a high-power patient," the researchers wrote.
The military health system serves nearly 1.3 million active-duty personnel of all ranks, in addition to military family members, retirees and their families, in 51 hospitals and 424 clinics. The active-duty force is 18% officer and nearly 82% enlisted, 82.5% male and 17.5% female. Roughly 69% of the force is white, while 31.2% identify as a person of color.
The research looked at how physicians responded to or treated officers of higher rank than themselves, as well as equal and lower-ranked officers, and enlisted personnel.
Additional trends that were observed included a finding that male physicians are more rank-conscious and respond to a patient's "power" more than female doctors did and showed more sex-based discrimination than female physicians.
Male physicians also were significantly more responsive to higher-ranking female patients than male patients, possibly because high-ranking women are still fairly uncommon across the services, perhaps eliciting "more respect and attention," the research said.
Schwab said the findings demonstrate that physicians are "human" and, as such, are susceptible to implicit bias. But there may be other factors at play, such as a high-ranking patient demanding care or unknowingly drawing it as leadership.
The concern with such bias is what Schwab called "the spillover effect": If physicians are spending more time with their peers or those of higher rank, then other patients are getting less attention.
"The effort has to come from somewhere," Schwab said.
Schwab said the research was supported by the military health system through access to records and data support. The study, he added, lends value to medicine as a whole because it is an opportunity to show that implicit bias exists in the profession and the perception of power plays a role.
As a retired financial officer for the military health system, Schwab said he recognized that he likely received more attentive health care in the system from his colleagues than other troops.
"It's hard to tell [bias] as an individual patient because you get the care you get, but I definitely felt I received more respect because of my circumstances," Schwab said.
He said the study was not designed to place blame on physicians; instead, it was meant to raise awareness of implicit bias to influence education and training.
"We want people to recognize that these implicit biases exist, and we can address them by developing physicians that are more representative of society or improving training for our physicians," Schwab said.
A spokesman for the Defense Health Agency said the organization is reviewing the article and its supporting materials but would not comment on the findings until they could be thoroughly reviewed.
DHA spokesman Peter Graves said the agency "is committed to delivering the highest quality of care to all of our patients, regardless of rank, race, color, sex, gender identity, religion, age or any other demographic."
"We always expect the same high standards to be applied to every patient in an exceptional way, anytime, anywhere, always," Graves said.
Related: In Reversal, Defense Department Now Wants to Bring Tricare Beneficiaries Back to Military Health System
Patricia Kime

You May Also Like

The amendment to the House Armed Services Committee's National Defense Authorization Act, or NDAA, would also make...

The lawsuit points to well-publicized issues with the Osprey's mechanics and names as defendants Bell Textron and Boeing...

A Military.com investigation in April uncovered several cases of abuse and sexual behavior between children at military child...

New research has found that younger males, including dependents, and those assigned to a state where abortion is strictly...
Military News
- Investigations and Features
- Military Opinion
Select Service
- National Guard
Most Popular Military News

Pfc. Katia Duenas-Aguilar, 23, was found dead in a residence about four miles outside of the base, according to a...

The bonuses were authorized under a law designed to provide benefits to millions of veterans affected by environmental...

Space Force Sgt. Lucas Macaj was found Thursday on Mills Glacier, near the base of Lamb's Slide within the national park.

The Pentagon said Tuesday that it believes none of the hundreds of tons of aid delivered over several days via a military...

A group of senators, led by Marsha Blackburn of Tennessee and Tommy Tuberville of Alabama, demanded "immediate action" in a...
Latest Benefits Info
- VA Home Loan: Are You Eligible?
- Burial at Sea: A Time-Honored Tradition
- VA Fertility Benefits for Military Veterans
- Virginia Veterans Rally the Troops, State Leaders in Support of Education Benefits
- 4 Tips for Flying Space-A
More Military Headlines

Bong shot down more planes than any other American pilot. Gen. Douglas MacArthur awarded him the Medal of Honor, the U.S...

The legislation would also order the services to analyze "the effect of beard growth on discipline, morale and unity within...
- Explorers Discover Possible Wreckage of World War II Ace Richard Bong's Plane in South Pacific
- 'Absolutely Fed Up': Senator Mulls Ways to Force Pentagon to Boost Incentive Pay for Guardsmen and Reservists
- Pentagon Says No Food Aid Moved Through Gaza Pier Has Made It to Palestinians
- Airmen, Space Force Guardians Could Grow Beards Under Pilot Program Proposed by House
- Air Force's Controversial Plan to Transfer National Guard Units to Space Force Gets Gutted by House
- 35 Years Later, Vice Adm. Davids Returns to Naval Academy Graduation in Historic Fashion
- USS Leyte Gulf Returns to Norfolk from Final Deployment Before Decommissioning in September
- Judge Dismisses Felony Convictions of 5 Retired Military Officers in US Navy Bribery Case
Military Benefits Updates
- Fertility Benefits for Active-Duty Service Members
- Deadly Marine Osprey Crash Triggers Wrongful Death Lawsuit Against Bell Textron, Boeing, Rolls-Royce
- Marine from Twentynine Palms Randomly Gunned Down While Sitting in Car at Park
- Last Service Member Released from Hospital After Landing Vessel Collision Injured 35 in Florida
- Coast Guard Academy Graduates Are Told They 'Are Going to Save the World'
- Chaplain for Coast Guard 7th District Fired, Marking Latest High-Profile Dismissal for Service in Recent Weeks
- US Coast Guard Says Texas Barge Collision May Have Spilled Up to 2,000 Gallons of Oil
Entertainment
- 'The Cold Blue' Gives a Legendary Filmmaker's Never-Before-Seen World War II Footage a New Life
- What Makes a War Movie a 'Classic,' According to Turner Classic Movies
- Jeff Bridges and Dave Bautista Headline All-Star Cast in New Take on 'Beowulf' Epic
- Apply now Enquire now
Study at UniSA
Accounting and Finance Business Management and HRM Marketing Property Tourism, Sports and Events
Architecture Communication Contemporary Art Creative Industries Design Film, Television and Visual Effects Journalism Urban and Regional Planning
Biomedical Science Health Science Human Movement, Sport, Clinical Exercise Physiology Laboratory Medicine Medical Radiation Science Nursing or Midwifery Nutrition and Food Sciences Occupational Therapy Pharmacy Physiotherapy Podiatry Speech Pathology
- Law & Criminal Justice
Aboriginal and Australian Studies Arts Human Services Languages Psychology Social Work
Aviation Construction Management Defence Engineering Environmental Science Information Technology Mathematics Science
- Teaching & Education
- What can I study
- Entry pathways
- Find an education agent
- Sponsorships
- Living in Adelaide
- UniSA Online
- Scholarships
- Postgraduate study
- Research degrees
- Executive Education
- Regional students
- Aboriginal students
- Discover our research Partner with us
- Research projects
- How to apply
- Check your eligibility
- Research scholarships
- Concentrations
- Cooperative Research Centres
- Research studies & volunteers
- Research experts
- Industry & collaboration
- Mawson Lakes
- Mount Gambier
- Psychology Clinic
- Health Clinics
- Disability Hub
- Wirringka Student Services
- Museums and galleries
- Industry & partnerships
- Enterprise Hub
About UniSA
- Our history
- Vice Chancellor
- Achievements
- Mission, values, vision
- Strategic action plan
- Staff directory
- UniSA Allied Health & Human Performance
- UniSA Business
- UniSA Clinical & Health Sciences
- UniSA Creative
- UniSA Education Futures
- UniSA Justice & Society
- Working at UniSA
- Publications
- Aboriginal engagement
- Login Staff Students Alumni
- Media centre
Dismissed and discharged: health systems still failing people with poor mental health
22 May 2024

Funded by mind Australia , the world first study found that people with psychosocial disabilities - people who live with disabilities as a result of poor mental health - not only experience distress when dealing with the NDIS, but also face ‘service pullback’ when they present to emergency departments when requiring emergency care.
Speaking with NDIS participants, the nationwide study found that when participants disclosed that they had NDIS support, clinicians wrongly assumed the NDIS provides medical and mental health crisis care.
It’s a concerning finding, particularly following the discrimination, non-inclusivity and lack of equality experienced by people with a disability, identified in the NDIS review and the disability royal commission .
In Australia, 1.1 million people have a psychosocial disability which causes limitations or restrictions in their everyday activities . Additional, 58% of these people also have a nervous or emotional condition, 42% have problems with memory or periods of confusion, 41% have behavioural conditions, and 40% have a mental illness (such as schizophrenia).
86% also have at least one other disabling condition (63% physical disability; 38% intellectual disability; and 33% sensory disability).
UniSA researcher and PhD candidate Heather McIntyre says that the disconnect between the NDIS and emergency departments is failing people with psychosocial disabilities.
“Time and time again we hear about people experiencing distress when they contact the NDIS – they fight to be heard, fight for support, and are often dismissed, so the last thing they need is to go through this again when they require emergency care,” McIntyre says.
“This is particularly concerning for people with a mental health condition, especially those with fluctuating psychosocial disabilities who may struggle with communication.
“Because many emergency department staff aren’t aware of the limitations of NDIS supports, they wrongly assume that the NDIS provides a higher level of care than it does.
“This leaves many people with a psychosocial disability being discharged at emergency without appropriate treatment and returned to the situation that caused them to present in the first place.
“It’s an inequitable and unsafe approach that is putting thousands of people at risk.”
McIntyre says there is an urgent need to strengthen service integration between the NDIS and emergency departments.
“Communication between the two services is not occurring seamlessly, which affects continuity of care. This needs to change,” McIntyre says.
“We must start at the pointy end: emergency department clinicians need more training and education to better understand how the NDIS works and how to best support people with a disability.
“They need to learn how to support people with neurodiversity and hearing impairments, how to build trust and how to really listen, as well as to provide low sensory environments.
“But equally, stronger connections and pathways must be established between NDIS providers and emergency departments so that everyone is on the same page.
“With budget cuts to the NDIS of 14 billion over the next four years, peoples’ disability supports will further be reduced, resulting in more emergency department presentations when supports are insufficient.
“In emergency departments we need to step up care, not ration care, if we are to support people with disabilities who already feel abandoned by the health system.”
………………………………………………………………………………………………………………………….
Notes to editors
The article is available online: McIntyre, H., Loughhead, M., Hayes, L., Allen, C., Barton-Smith, D., Bickley, B. et al. (2024) ‘ Everything would have gone a lot better if someone had listened to me’: A nationwide study of emergency department contact by people with a psychosocial disability and a National Disability Insurance Scheme plan . International Journal of Mental Health Nursing, 00, 1–12.
……………………………………………………………………………………………………………………….
Media contact: Annabel Mansfield M: +61 479 182 489 E: [email protected]
Researcher: Heather McIntyre E : [email protected]
Other articles you may be interested in
Survey reveals growing support for changing Australia Day date
Brain scans for babies reduce risk of stroke later in life
Scientists aim to stop harmful gut bacteria triggering Alzheimer’s
Australian students
Phone: +61 8 8302 2376 Enquiry: unisa.edu.au/enquiry
International students
Phone: +61 8 9627 4854 Enquiry: unisa.edu.au/enquiry

University of Birmingham

Inadequate access to simple elective surgery in developing countries is storing up future health problems for patients and may create a spiral of future health complications putting more people’s lives at risk, a new study reveals.
Analysing the experience of more than 18,000 patients in 640 hospitals across 83 countries, researchers, experts used hernia repair to represent elective health care, concluding that such treatments are essential to prevent over-reliance on emergency systems.
The study reveals that inguinal hernias are treatable with simple day-case surgery, but, if neglected, the need for more complex emergency surgery increases substantially, leading to delayed recovery and far higher total health-care costs.
Led by experts at the University of Birmingham, the NIHR Global Health Research Unit in Surgery study notes that increasing reliance on emergency care has resulted in crisis management becoming routine across a wide range of conditions that respond well to early elective treatment.
Boosting the use of elective surgery for conditions that can be fixed simple and early treatments will reduce the risk of complex, and potentially risky, emergency surgery. Dr Maria Picciochi - University of Birmingham
Study co-author Dr Maria Picciochi, from the University of Birmingham, commented: “Boosting the use of elective surgery for conditions that can be fixed simple and early treatments will reduce the risk of complex, and potentially risky, emergency surgery.”
Study co-author Prof Aneel Bhangu, from the University of Birmingham, also added: “Health policy makers can use our findings as a proxy for other elective conditions, creating a system strengthening approach to integrate surgery into the wider system of health care. This would relieve pressure on emergency pathways and reduce the health burden on society and healthcare services.”
The study shows that inguinal hernias are mostly a disease of working-age patients around the world, and, if neglected, may require bowel resection. This more complex surgical treatment leads to slow recovery and far higher total health-care costs.
Researchers also found a clear global imbalance in access to mesh repair - reflecting poor access to simple medical devices in lower-income countries. Mesh is well proven to reduce long-term hernia recurrence, is simple to place, low-cost and scaleable.
The researchers identified actionable targets for system strengthening, which include:
- Educating communities and community health workers around hernia symptoms;
- Improving referral systems and increasing mesh repair for hernias;
- Establishing a global quality improvement programme in mesh placement for hernias - strengthening supply chains, making mesh affordable and increasing training; and
- Improving capacity for simple, cost-effective surgery.
“Our study showed multiple weaknesses in access and quality in current health-care systems, with a particular disadvantage in lower-income settings,” commented Dr. Picciochi. “As a result, there was higher emergency demand, which further reduced elective capacity and might create downward spirals.
“If weak access and quality persist over several electively treatable conditions, both surgical and non-surgical, multimorbidity can also become established, which makes future elective care harder and emergency care even more complicated.”
Findings of the study and its wider implications will be discussed during the side event hosted by the NIHR Global Surgery Unit at the World Health Assembly, on 28 th May.
Featured staff

Professor Aneel Bhangu
Professor of Global Surgery
Notes for editors
For more information, please contact our Press Office . For out-of-hours enquiries, please call +44 (0)121 414 2772.
The University of Birmingham is ranked amongst the world’s top 100 institutions, its work brings people from across the world to Birmingham, including researchers and teachers and more than 8,000 international students from over 150 countries. Discover Birmingham .
‘ Access to and quality of elective care: a prospective cohort study using hernia surgery as a tracer condition in 83 countries ’ – NIHR Global Health Research Unit on Global Surgery is published in Lancet Global Health.
Participating countries included: Albania, Algeria, Argentina, Austria, Australia, Aruba, Bosnia and Herzegovina, Bangladesh, Burkina Faso, Bulgaria, Burkina Faso, Burundi, Benin, Brazil, Cambodia, Cameroon, Canada, Chile, China, Colombia, Croatia, Cyprus, Czech Republique, Dominican Republic, Egypt, Ethiopia, France, Gabon, Germany, Georgia, Ghana, Greece, Guatemala, India, Ireland, Iran, Iraq, Italy, Japan, Jordan, Kazakhstan, Kenya, Lebanon, Libya, Lithuania, Madagascar, Malaysia, Mali, Malta, Mexico, Morocco, Namibia, New Zealand, Nigeria, Oman, Pakistan, Palestine, Paraguay, Peru, Poland, Portugal, Qatar, Republic of North Macedonia, Romania, Russian Federation, Rwanda, Saudi Arabia, Serbia, Slovenia, South Africa, Spain, Sri Lanka, Sudan, Sweden, Switzerland, Syria, Thailand, Togo, Tunisia, Turkey, Uganda, United Kingdom, United States, Yemen.
The National Institute for Health and Care Research (NIHR)
The mission of the National Institute for Health and Care Research (NIHR) is to improve the health and wealth of the nation through research.
We do this by:
- Funding high quality, timely research that benefits the NHS, public health and social care;
- Investing in world-class expertise, facilities and a skilled delivery workforce to translate discoveries into improved treatments and services;
- Partnering with patients, service users, carers and communities, improving the relevance, quality and impact of our research;
- Attracting, training and supporting the best researchers to tackle complex health and social care challenges;
- Collaborating with other public funders, charities and industry to help shape a cohesive and globally competitive research system;
- Funding applied global health research and training to meet the needs of the poorest people in low and middle income countries.
- NIHR is funded by the Department of Health and Social Care. Its work in low- and middle-income countries (LMICs) is principally funded through UK Aid from the UK government.

World-leading surgical research team gets fresh funding to save lives
A world-leading global surgical research team led by the University of Birmingham has received £7 million to continue life-saving work in developing countries.
16 February 2022

COMMENTS
On arrival at the emergency department, the patient described ongoing chest pain and shortness of breath. The son reported that the patient had fallen at home 2 days before admission, but the ...
The patient was brought by ambulance to the emergency department of this hospital. ... Oliguria developed. Additional laboratory studies were obtained ... In this case, the levels of C-reactive ...
ECG Cases 49 - ECG and POCUS for Dyspnea and Chest Pain. In this ECG Cases blog, Jesse McLaren and Rajiv Thavanathan explore how ECG and POCUS complement each other for patients presenting to the emergency department with shortness of breath or chest pain. They explain complementary diagnostic insights into pericardial effusion and cardiac ...
Emergency Medicine Case Studies - LEARNing Rounds: Learn, Evaluate, Adopt, Right Now is an essential resource for a variety of emergency medicine clinicians including experienced physicians, residents, physician assistants, nurse practitioners, nurses, and medical students rotating in the emergency department. Finally, this book can be used as ...
Treatment involves supportive care and treatment of underlying causes. Case Report: A 55-year-old male dependent on a gastrojejunostomy tube presented to the emergency department for altered mental status. The patient had metabolic alkalosis, electrolyte abnormalities, and prolonged QT interval on electrocardiogram.
A 16-day-old girl is brought to the emergency department with a rash. Don't miss the diagnosis. Clinical Case, September 04, 2012. Not-to-Miss Diagnosis: 10-Year-Old With Right Knee Pain When a 10 ...
Emergency department crowding is a sentinel indicator of health system functioning. While often dismissed as mere inconvenience for patients, impact of ED crowding on avoidable patient morbidity and mortality is well documented but remains largely underappreciated. The physical and moral harm experienced by ED staff is also substantial.
2. Emergency department characteristics. According to Hall (), patients in emergency departments can be referred to an outpatient clinic or to a doctor and nurse in treatment rooms depending on the nature of the disease.This referral must be specialised by the level of urgency or by disease type (orthopaedics, for instance) and is made in a triage phase by nurses whose associated functions are ...
Background Over the last two decades, Emergency Department (ED) crowding has become an increasingly common occurrence worldwide. Crowding is a complex and challenging issue that affects EDs' capacity to provide safe, timely and quality care. This review aims to map the research evidence provided by reviews to improve ED performance. Methods and findings We performed a scoping review ...
5. Online resource allocation. In this section we present a general framework capable of representing different policies for the ED real-time resource allocation. Such policies are managed by a decision maker, which is able to consult in real time the activities to be performed and the waiting time of each patient.
Emergency departments: extremely busy places. A strong theme running across five of the systems was the busyness which acute trust and ambulance interviewees reported within the EDs. There was also some perception that this had increased over time: ... Phase 2: case studies of six emergency and urgent care systems - methods and overarching ...
The emergency department specifically deals with social injustice, health and economic disparities, violence, substance abuse, and disaster preparedness and response. This journal focuses on how emergency care affects the health of the community and population, and conversely, how these societal challenges affect the composition of the patient ...
by clicking on the category and then episode title below. The EM Cases Summaries are succinct, written, easily navigable, key point reports of each main episode podcast, authored by Our Team that you can download to your smartphone or tablet to reference and read at the bedside or at your leisure automatic download via dropbox.
According to the case study in an Emergency Department in the Silesia Province, the most common adverse event is the excessive waiting time for medical service. Value Stream Mapping (VSM) was successfully applied to reduce waiting time in all stages of medical care to implement process standardization by identifying and then eliminating waste ...
September 30, 2022. (© stock.adobe.com) In a pair of new studies, Yale researchers document a widespread and increasing level of overcrowding in America's emergency departments (EDs), a crisis that puts patient safety and access to care at risk. For the studies, the researchers examined, respectively, the progression in recent years of two ...
Community Wind Shelters: Background and Research. Because of the rising frequency of extreme weather, the Federal Emergency Management Agency (FEMA) strongly encourages homeowners and communities to build safe rooms to FEMA standards. Community shelters have been consistently needed due to the increased risk posed by strong winds and flying ...
The selection process of the Emergency Department of the Sansepolcro Hospital (EDSH) as case-study, is presented in Section 2, by briefly describing its role in the health network of the entire region. The functionality of the Emergency Department is described in Section 3, both in normal and in emergency conditions. Due to occurrence of ...
Beth Israel Lahey Health. Hospitals use specialized team, including pharmacists, to promote post-discharge care coordination. Boston Children's Hospital. "Golden Ticket" dramatically improves discharge safety. Holyoke Medical Center. Investing in high-touch care coordination to reduce emergency department revisits.
A 38-year-old man was evaluated in the emergency department because of altered mental status and a first seizure. Examination revealed an involuntary upward gaze and confusion. Laboratory evaluatio...
Equitable Care: Help foster a culture and environment that ensures that this patient population receives equal attention and resources; work to decrease biases. Physical Environment: Be aware of defined spaces for safe and private evaluation and ongoing treatment. Patient and Staff Safety: Regularly assess and communicate patient risk; know ...
The best estimates I could find, published in 2019, before the covid-19 pandemic, suggest that 10% of patients were boarded in ERs before receiving hospital care. About 30% to 50% of these patients were older adults. "It's a public health crisis," said Aisha Terry, an associate professor of emergency medicine at George Washington ...
The study aims were to evaluate the species distribution and antimicrobial resistance profile of Gram-negative pathogens isolated from specimens of intra-abdominal infections (IAI), urinary tract infections (UTI), respiratory tract infections (RTI), and blood stream infections (BSI) in emergency departments (EDs) in China. From 2016 to 2019, 656 isolates were collected from 18 hospitals across ...
Key Points. Question Is maternal influenza vaccination during pregnancy associated with a reduction in influenza-associated hospitalizations and emergency department (ED) visits in infants younger than 6 months?. Findings In this case-control study of 3764 infants younger than 6 months, maternal vaccination was associated with a reduction in influenza-associated hospitalizations and ED visits ...
People who use substances (PWUS) encounter significant barriers to accessing care for their complex health needs. As a result, emergency departments (EDs) often become the first point of healthcare access for … Read the full article ›
Design. This work will use a prospective mixed methods case study design 19 20 to collect quantitative and qualitative data in an adult and a paediatric ED. We will use both process measures (ie, tracking specific steps leading to diagnosis including interactions with tools, communications between people and monitoring elapsed time), and multiple qualitative methods (eg, field observations ...
Organizational learning is a continuous process of integrating data and knowledge to ensure improvement. This qualitative study focuses on the starting points and presuppositions of organizational learning within a surgical department. Starting points for individual learning were informal and based on day-to-day work (e.g., solving a specific problem) and organizational learning encompassed ...
For the study, the researchers examined data from 1.5 million emergency department visits in the military health system, looking at the rank of a patient compared with the doctor's rank and ...
22 May 2024 A serious disconnect between emergency departments and the NDIS is failing people with mental health conditions, as new research from the University of South Australia shows that they frequently receive inadequate care within emergency departments, potentially putting thousands of vulnerable people at risk.. Funded by mind Australia, the world first study found that people with ...
Published 21 May 2024. Simple day-case surgery can reduce the need for more complex emergency surgery. Inadequate access to simple elective surgery in developing countries is storing up future health problems for patients and may create a spiral of future health complications putting more people's lives at risk, a new study reveals.